Abstract
Human thioredoxin (hTrx), which can be secreted from cells upon stress, functions in allergic skin inflammation as a T cell antigen due to homology and cross-reactivity with the fungal allergen Mala s13 of the skin-colonizing yeast Malassezia sympodialis. Recent studies have shown that cell wall polysaccharides of Malassezia are detected by the immune system via the C-type lectin receptors Dectin-1 and Dectin-2, which are expressed on myeloid cells. Therefore, this study aimed to investigate a putative interaction between Dectin-1, Dectin-2 and the allergens Mala s13 and hTrx. Stimulation of human monocyte-derived dendritic cells or macrophages with Mala s13 or hTrx resulted in remarkable secretion of IL-1β and IL-23. Blocking experiments suggest that hTrx induces IL-23 by Dectin-1 binding and IL-1β by binding to either Dectin-1 or Dectin-2. Regarding Mala s13, Dectin-1 appears to be involved in IL-1β signaling. Interference of Syk kinase function was performed to investigate downstream signaling, which led to diminished hTrx responses. In our experiments, we observed rapid internalization of Mala s13 and hTrx upon cell contact and we were able to confirm direct interaction with Dectin-1 as well as Dectin-2 applying a fusion protein screening platform. We hypothesize that this cytokine response may result in a Th2/Th17-polarizing milieu, which may play a key role during the allergic sensitization in the skin, where allergen presentation to T cells is accompanied by microbial colonization and skin inflammation.
Subject terms: Cytokines, Inflammation, Medical research
Introduction
Autoimmunity and allergy represent two examples of an aberrant reaction of the immune system, where immune responses are mounted against harmless self or environmental antigens. A critical step during the sensitization process seems to be the generation of memory T and B cells. While allergen- and autoantigen-specific T cells are tolerogenic in healthy donors, the immune system of sensitized individuals considers allergens or autoantigens to be dangerous. The sensitization process is thought to result from a situation, where antigen recognition takes place under parallel heavy attack of the immune system. It is believed that danger signals are present under such circumstances, which influence the antigen presenting cells (APC) towards a pro-inflammatory phenotype, leading to the generation of specific pro-inflammatory T cells. This break of tolerance is regarded as a key point in the development of autoimmunity and allergy. While many molecules have been described to act as a danger signal, their potential to shape the immune system is often unclear.
Using tonsillar cells of allergic patients, it was shown that stimulation of APC via toll-like receptors (TLR) 4 and 8 as well as the cytokines IL-1β and IL-6 have the potential to break specific T cell tolerance towards several environmental allergens1. A similar mechanism is discussed for DAMPs (danger-associated molecular pattern) and PAMPs (pathogen-associated molecular pattern)2,3.
A disease setting, where allergy, DAMPs and PAMPs are in a close interaction, is atopic dermatitis (AD), the most common inflammatory skin disease worldwide4. Being our outermost barrier, the skin is colonized with a vast amount of microorganisms of which Staphylococcus aureus is the most widely studied. AD patients are also frequently colonized with and IgE-sensitized against the opportunistic yeast Malassezia sympodialis5. Antifungal treatment leads to an improvment of skin symptoms6, which may be due to the extinction of fungal allergens but also due reduced PAMP burden. Recent studies have shown that Malassezia PAMPs are recognized by Dectin-1 and Dectin-2, members of the pattern recognition receptor (PRR) family of C-type lectin receptors (CTLR), leading to NLRP3 inflammasome activation and finally IL-1β production7,8. CTLR are well-known for sensing fungal cell wall glucans or mannans, but also non-sugar molecules, such as DAMPs, have been described as ligands9–11. Generally, DAMPs like chaperones, heat-shock proteins and stress proteins have been linked to autoimmune disorders12, suggesting an intrinsic mechanism.
Interestingly, we and others showed in the past, that a genetically highly conserved human paralogue of the Malassezia allergen Mala s13, namely thioredoxin (hTrx) also acts as a DAMP on the immune system and is released upon stress from skin cells13–16. In detail, hTrx leads to the release of IL-13 and IL-10 from human peripheral blood mononuclear cells, while the IL-10 response is strikingly diminished in IgE-sensitized patients14.
To investigate whether Malassezia PAMPs and related human DAMPs may be ligands for CTLR, we performed specific binding and blocking experiments on monocyte-derived dendritic cells and macrophages as model APCs in vitro.
Finally, we show that Mala s13 and hTrx, but not Mala s6 or Mala s11, can be bound by Dectin-1 and Dectin-2. Blocking experiments suggest however that the IL-23 response to hTrx is mediated partially by Dectin-1, and the IL-1β response by Dectin-1 and -2. Regarding Mala s13, Dectin-1 appears to be involved in IL-1β signaling. Such pro-inflammatory capacities have been reported to facilitate sensitization in atopic individuals.
Results
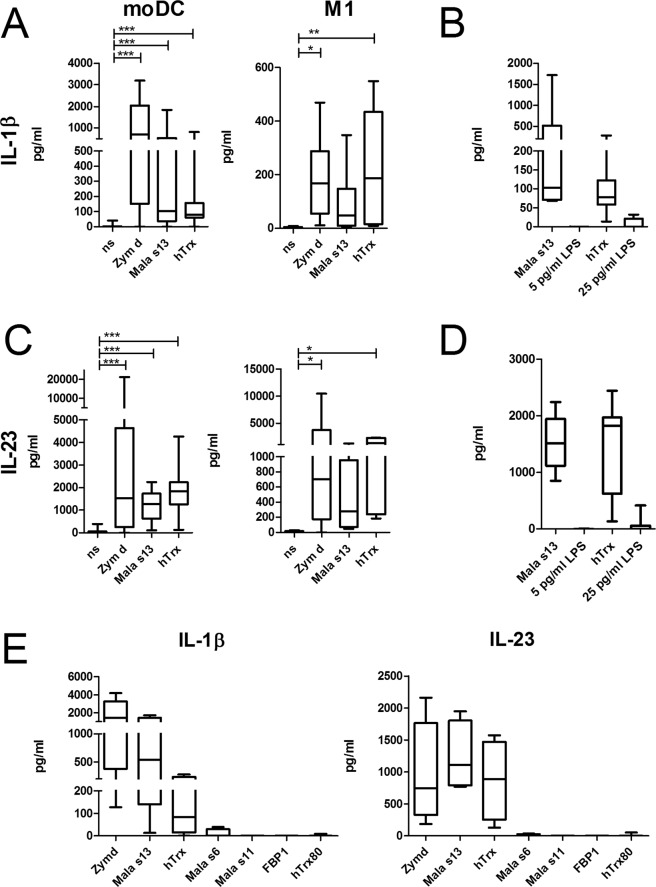
Cytokine response of myeloid cells to fungal glucans, the fungal allergen Mala s13 and its human paralogue hTrx
Monocyte-derived dendritic cells (moDC) and M1-macrophages have been shown to express the CTLR Dectin-1 and Dectin-2 and are well-studied regarding the binding of fungal glucans via the Dectin-1 receptor. In order to investigate their response to Mala s13 and hTrx, cytokine secretion was measured by ELISA after 16 h stimulation. Both cell types released considerable amounts of IL-1β and IL-23 in response to both proteins as well as to hot alkali-treated Zymosan (Zymosan depleted), a S. cerevisae-cell wall preparation that is described as a specific ligand of Dectin-1 but not of TLR (Fig. 1A,C). Remaining lipopolysaccharide (LPS)-contamination of recombinantly E. coli-expressed Mala s13 and hTrx was determined by LAL-assay. Equivalent LPS concentrations did not lead to IL-1β secretion in our assay (Fig. 1B,D); cytokine secretion in response to LPS was detectable in our system only upon a concentration of 2 ng/ml or higher (Supplemental Figure S1).
Figure 1.
Cytokine response to fungal glycans, the fungal allergen Mala s13, and its human homologue hTrx. Secretion of IL-1β (A) and IL-23 (C) was measured in moDC or M1-macrophage cell culture supernatants by ELISA 16–18 h after stimulation as depicted (moDC n = 25; M1-macrophages n = 6). IL-1β (B) and IL-23 (D) release by moDC in response to the Mala s13, hTrx and the respective LPS contamination levels in the assay, 5 pg/ml and 25 pg/ml (n = 7). (E) Cytokine response to Zymosan depleted, Mala s13, and hTrx compared to further recombinant microbial antigens (Mala s6, Mala s11, FBP1) and a truncated form of hTrx (Trx80) (n = 6).
To exclude an artefact generated by recombinantly expressed polyhistidine-tagged proteins per se, moDCs were stimulated with the Malassezia allergens Mala s6 and Mala s11 and S. aureus fibronectin-binding protein1 (FBP1) which were expressed and purified equivalently. Further, we tested whether a cleavage product of hTrx, Trx80, is sufficient for the observed cytokine release. However, neither IL-1β nor IL-23 was released by any of these antigens, suggesting a specific receptor (Fig. 1E).
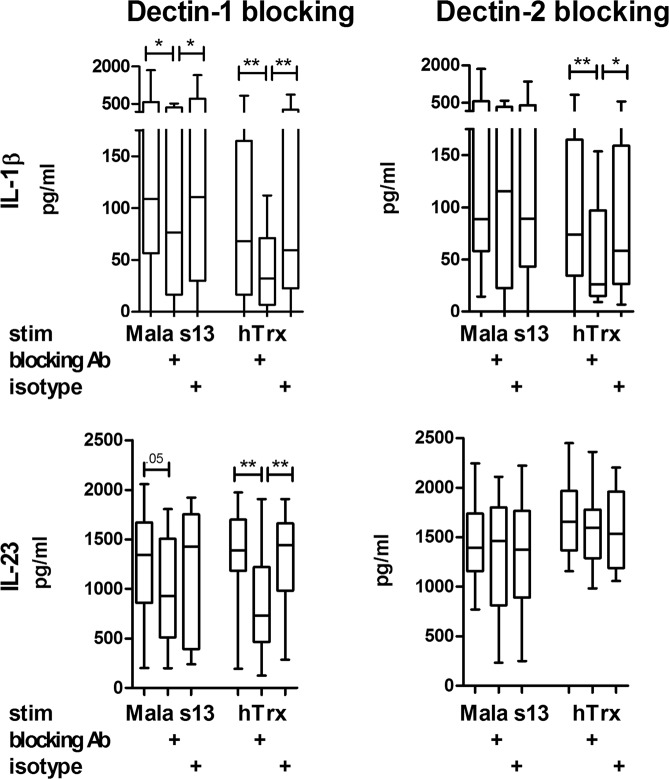
Blocking of Dectin-1 decreases cytokine response
To test whether Dectin-1 and/or Dectin-2 recognize Mala s13 and hTrx, receptor blocking applying specific antibodies was performed prior to stimulation. Blocking Dectin-1 on moDC had a clear inhibitory effect on IL-1β and IL-23 cytokine release upon hTrx stimulation. IL-1β responses to Mala s13 were also reduced significantly in our set of experiments. The blockade of Dectin-2 also impaired the IL-1β release in response to hTrx, which was significantly different from the isotype control, but not IL-23 and not the response to Mala s13 (Fig. 2).
Figure 2.
Blocking of Dectin decreases cytokine response to hTrx. Secretion of IL-1β and IL-23 was measured in moDC cell culture supernatants by ELISA 16–18 h after stimulation with Zymosan depleted, Mala s13, and hTrx with or without preliminary 1 h incubation with blocking antibodies against Dectin-1 or Dectin-2 as indicated (n = 12). Blocking antibodies were controlled applying isotype controls.
Particulate cell wall components of Saccharomyces cerevisiae (dispersable whole glucan particles, WGPd) have also been shown to specifically signal via Dectin-117, while the soluble form (WGPs) is supposed to efficiently block this process18. In our set of experiments, stimulation with WGPd led to secretion of IL-23 and IL-1β, which was at least partially blocked by WGPs (Fig. 3). To confirm the results from Dectin-1-blocking antibodies above, hTrx was applied with and without pre-incubation with WGPs (Fig. 3). While WGPs was able to reduce the IL-23 secretion significantly, the IL-1β response was reduced only by trend in this set of experiments.
Figure 3.
Blocking of Dectin-1 or Syk kinase decreases cytokine response to hTrx. Secretion of IL-1β and IL-23 was measured in moDC cell culture supernatants by ELISA 16–18 h after Saccharomyces cerevisae dispersable whole glucan particles (WGPd) and hTrx stimulation with or without preliminary 1 h incubation with S. cerevisae soluble whole glucan particles (WGPs) or piceatannol.
Blocking of Syk kinase decreases cytokine response
CTLR that possess ITAM-motifs like Dectin-1 and Dectin-2 are well-known to signal intracellularly via the Syk kinase leading to the induction of cytokines and inflammasome activation19. Effects of WGPd have been shown to be efficiently diminished upon Syk blockade by the phenolic stilbenoid piceatannol. To investigate whether hTrx signaling follows this pathway, too, we blocked Syk kinase by piceatannol upfront hTrx stimulation, and found in our set of experiments that IL-23 and IL-1β secretion were reduced significantly (Fig. 3).
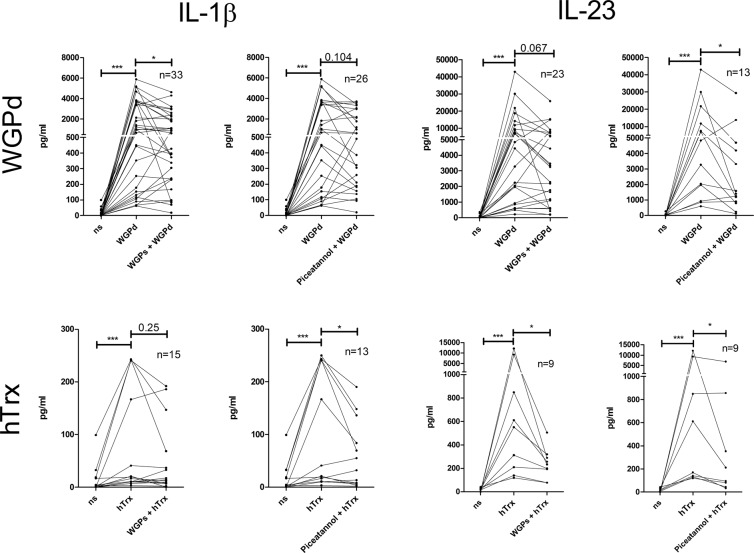
Direct binding of Mala s13 and hTrx to Dectin-1 and Dectin-2
In order to clarify whether the interaction of Mala s13/hTrx and Dectin-1 is direct or indirect, binding strength to recombinant Dectin-1- and Dectin-2-Fc chain fusion molecules was determined according to an established protocol20. In this system, the extracellular part of Dectin is fused with the Fc-fragment of human IgG1, which can be detected by a HRP-labeled secondary antibody. As a control, binding of each test antigen was also determined to the empty hFc-fragment. Specific binding to Dectin-1 and Dectin-2 was clearly detectable for Mala s13 and hTrx as well as Zymosan, but not for Mala s6 and Mala s11 (Fig. 4). All recombinant proteins were intact and were applied in equal amounts, as verified by western blotting (Figure S2).
Figure 4.
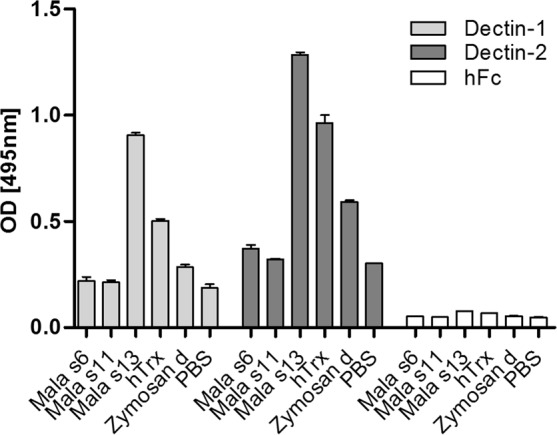
Binding of putative ligands to Dectin-1 and Dectin-2 was assessed applying a Dectin-hFc fusion protein screening platform. Bound fusion protein was assessed by an anti-hFC-antibody as optical density (OD). As a negative control, binding of each putative ligand to hFc only was tested (hFc). n = 2. All measurements were performed as duplicates. hTrx, human thioredoxin; PBS, phosphate buffered saline; Zymosan d, Zymosan depleted. Error bars represent SEM.
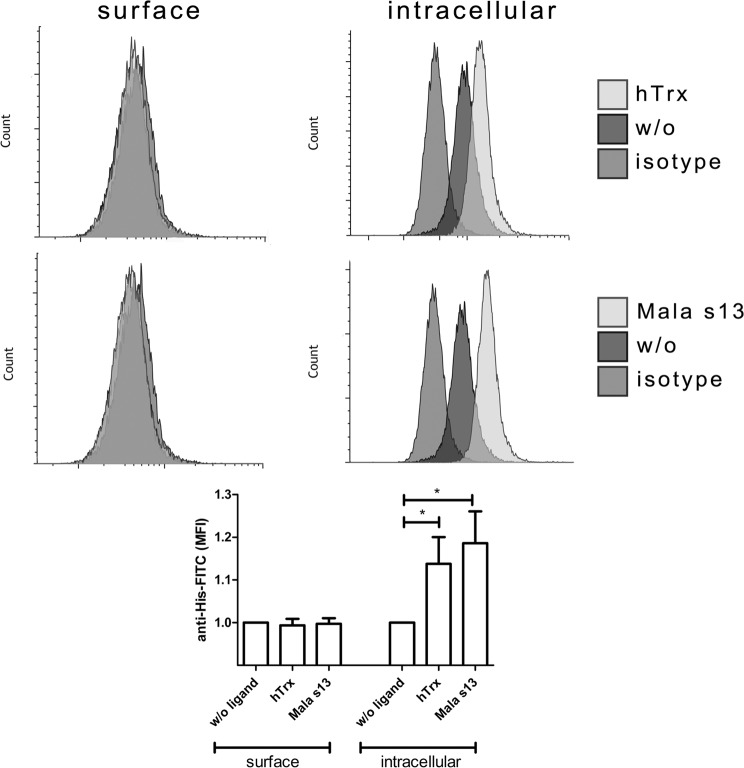
Internalization of Dectin-1 and antigens after stimulation
It has been reported that Dectin-1 and its ligands get internalized quickly upon binding21. To test if Mala s13 and hTrx follow this behavior, the internalization of the CTLR-antigen complex was investigated. After blocking to prevent unspecific binding, moDC were stimulated for 20 minutes with Mala s13 or hTrx. Since both antigens are 6xHis-tagged, detection was performed by immunofluorescence directed against the tag. Cells were stained on the cell surface first and subsequently intracellularly. The depicted increase in staining intensity when comparing surface to intracellular signals suggests the absence of both proteins on the cell surface but presence inside the cell (Fig. 5).
Figure 5.
Surface and intracellular staining of Dectin-1 ligands. Recombinant Mala s13 and hTrx were detected inside moDC 10–20 min after incubation by a fluorescently labelled anti-6xHistidine-tag antibody. Prior to that, surface staining applying the same antibody was performed to block surface-bound antigens. Exemplary stainings are shown as indicated. w/o: medium control. Plotted graph shows arithmetic mean and SEM of six independent experiments, medium control is set to 1.
Discussion
In this study we demonstrate in an in vitro model that human APC are capable of mounting a pro-inflammatory response to the fungal allergen Mala s13 as well as to its human highly-conserved paralogue, hTrx, via signaling in part through the CTLR Dectin-1 and Dectin-2. We can show strong IL-23 and IL-1β production in dendritic cells as well as macrophages, which both play important roles in the initiation and perpetuation of the skin inflammation in AD4. We show for the first time direct interaction of Mala s13 and hTrx to Dectin-1 and Dectin-2 on an established binding test platform22.
Crossreactivity between microbial and human antigens has also been described for Aspergillus fumigatus, also in the context of AD23,24. Interestingly, a recent study revealed upregulation of Dectin-1 and other pattern recognition receptors in patients suffering from aspergillosis25.
Malassezia species are part of a healthy skin microbiota and were recently identified as a target for Dectin-1, leading to the activation of the NLRP3 inflammasome and secretion of IL-1β8. Further, it has been demonstrated that Dectin-2 can also bind specifically to a Malassezia compound7,26. Since in a subgroup of AD patients Malassezia-specific IgE and T cell reactivities are observed, we hypothesize that the pro-inflammatory responses evoked via CTLR may underlie this phenomenon.
Dectin-1 has also been shown to have implications for allergic conditions, since mouse models of allergic asthma to house dust mite (HDM) showed reduced symptoms if Dectin-1 was knocked out27,28. It could be observed that parallel β-glucan signaling leads to exacerbation of allergy symptoms with a specific Th2/Th17 polarization phenotype. It could specifically be demonstrated that β-glucan can induce IL-17A directly and is furthermore able to enhance the HDM-induced secretion of IL-4 and IL-13 in a more than two-fold magnitude, resulting in a steroid-resistant phenotype of the disease28. Subsets of dendritic cells, as well as macrophages were identified as target cell populations27,29.
Within the CTLR family, Dectin-2 has been described to induce a Th2/Th17 allergic response to HDM, too, but rather by direct binding to HDM compounds26,30–32. In a previous study, we were able to confirm the presence of the Th2/17 HDM-reactive T cell subtype in patients suffering from AD33. This Th2/Th17 phenotype is in line with the cytokines detected here. While IL-23 is obligatory for survival of Th17 cells34, IL-1β has been reported as an important factor of the Th2 immune response35. In the context of allergy, Dectin-signaling may therefore promote the present type 2-response while fueling the fungus-associated Th17 axis in parallel.
CTLR are well-known for binding sugar residues and binding of Dectin-1 to β-glucan and Dectin-2 to α-mannans has been studied extensively. Therefore our findings upon stimulation with proteins may appear surprising. However, it has been demonstrated that proteins can also be for CTLR family members. For example, CLEC9A has been shown to bind F-actin, which under healthy circumstances resides inside the cell but gets exposed after cell death36. CLEC8A (also known as LOX-1 or SCARE-1) is a receptor for heat shock protein 70 (HSP70), which is a chaperone and well-described secreted alarmin37. Interestingly, CLEC8A-related proteins like Siglec, SREC-1 (SCARF-1) and FEEL-1 (SCARH-2) have also been reported to bind HSP-70. These three transmembrane receptors share homologous structures and react to low density lipoprotein (LDL) as a common ligand. Recently, Siglec-5 and Siglec-14 of the I-type lectin family have been shown to bind HSP70, too10. These examples may lead to the hypothesis that CTLR act as receptors for DAMPs and alarmins in the context of inflammation. This theory may explain the observed binding to hTrx here, since it is secreted upon stress16 and possesses distinct properties of a DAMP: we could show that healthy individuals mount a pronounced IFN-γ response accompanied by IL-10 from monocytes, while AD patients with detectable IgE-sensitization against hTrx elicit predominantly IL-13 with reduced IL-10 levels14.
It might be of interest to investigate whether the immune response described here can further be amplified via parallel signaling through other PRRs, like TLR2, TLR3, or TLR438,39. Synergistic effects have also been reported upon parallel binding of fungal components by two different CTLRs40. On the other hand, some CTLR may also counteract others41.
Our findings of an interaction of a fungal allergen/PAMP and its human paralogous DAMP with Dectin-1 and Dectin-2 may help to understand the Th2/Th17 phenotype discovered in AD patients33,42. Therefore, our data underlines the rationale for a Th17-specific therapeutical intervention. The IL-17A-targeting biological Secukinumab which is approved in the treatment of psoriasis is already under investigation in AD (NCT02594098 and NCT03568136). Further, a human anti-IL-17C antibody is currently under study (NCT02739009). IL-23 can be targeted by Ustekinumab, an anti-IL-12/IL-23 antibody directly, and is under investigation in an interventional study with AD patients (NCT01806662).
Aside from AD, further roles of hTrx and Mala s13 can be speculated for other dermatological diseases, since it was shown that keratinocytes may express Dectin-1 on their surface after stimulation with β-glucan, resulting in an immune response43. This may be crucial for patients with AD, since the allergic inflammation and the site of Malassezia colonization co-localize in this disease setting.
Material and Methods
ELISA: Cell culture supernatants were collected at indicated time points and cytokine secretion was measured by ELISA. IL-1β was determined by ELISA kit from R&D systems (Minneapolis, MN, USA) and IL-23 from affymetrix eBioscience (Santa Clara, CA, USA). Assays were conducted according to manufacturers’ instructions.
Allergens and stimuli: Recombinant Mala s6, s11, s13, and hTrx were produced as [His]6-tagged fusion proteins in Escherichia coli and purified by means of Ni2+ affinity chromatography (Qiagen, Hilden, Germany), as described previously44. FBP was produced by the same method, described by45. LPS contamination was determined by LAL test (Limulus Amebocyte Lysate, Pyrochrome, East Falmouth, MA, USA). The LPS concentration of hTrx was 10 ng/mg protein, corresponding to 25 pg/ml in the working concentration; the LPS content of Mala s13 was 1.5 ng/mg protein, corresponding to 3.75 pg/ml in the working concentration. Further, hTrx80 (Biotechne, Minneapolis, MN, USA) and Zymosan depleted (InvivoGen, San Diego, CA, USA) were included in stimulation assays.
Cell Culture: CD14-positive monocytes were isolated from buffy coats obtained from the local blood bank as well as volunteers. According to the guidelines for blood donation, the anonymous donors were healthy and had not taken any medication for four weeks before giving blood. No volunteer was under systemic immunosuppressive treatment and all blood donors provided their informed written consent. The study was conducted according to the Declaration of Helsinki Protocols and approved by the ethics committee of the Hannover Medical School (MHH). Monocytes were isolated to generate monocyte-derived human dendritic cells (MoDCs) or classical macrophages (M1). More precise, peripheral blood mononuclear cells (PBMCs) were isolated by density gradient centrifugation (Pancoll human, Pan Biotech, Aidenbach, Germany). Out of these, monocytes were isolated by CD14 labelled magnetic beads (MACS Miltenyi Biotech, Bergisch-Gladbach, Germany) following manufacturer’s instructions. Monocytes were cultured in RPMI (Biochrom, Berlin, Germany) supplemented with 5% FCS (Pan Biotech), 1 M Hepes (Biochrom), 2mM L-glutamine (Biochrom), 1% Penicillin/Streptomycin (Biochrom), 10 ng/ml recombinant human IL-4 (Biotechne) and 10 ng/ml recombinant human GM-CSF (Biotechne) for DCs for 7 days. In order to generate macrophages, the protocol was performed equivalently except the addition of IL-4. In blocking-experiments, DCs and M1 were incubated with m-anti-hDectin1- or m-anti-hDectin2-blocking antibodies (10 µg/ml, InvivoGen), whole glucan particles, soluble (WGPs, 1 µg/ml, InvivoGen), or 15 µg/ml piceatannol (Merck, Darmstadt, Germany) for 1 h and compared to isotype mIgG1 (10 µg/ml, BioLegend, San Diego, CA, USA) and mIgG2a (10 µg/ml, R&D), respectively. After incubation, cells were left unstimulated or were stimulated with 100 µg/ml Zymosan depleted (InvivoGen), 20 µg/ml whole glucan particles, dispersable (WGPd, InvivoGen), Mala s6, s11, s13, FBP1, hTrx80 (R&D), hTrx (all 2.5 µg/ml) or LPS as indicated (Sigma-Aldrich, Munich, Germany) for 16–18 h.
Flow cytometry: MoDCs were incubated with PE-labelled m-anti-hDectin-1 antibody (R&D, clone 559931) or respective mIgG2b isotype (BioLegend) for 45 minutes at 4 °C. Cells were washed three times with PBS (Pan Biotech) and analyzed on FACSCanto II (BD, Franklin Lakes, NJ, USA). 20.000 events were collected in each measurement.
Internalization: In order to detect internalization of putative Dectin-1 ligands, cell surface and intracellular immune staining was performed. moDCs were generated and stimulated as described above. 20 minutes post stimulation cells were fixed using 4% formaldehyde in PBS for 30 minutes at 4 °C. After blocking of unspecific binding, cells were stained by FITC-labelled mouse anti human 6xHistidine-epitope-tag antibodies (Acris, clone AD1.1.10) or respective isotype controls (mIgG1-FITC, Sigma-Aldrich) for 30 min on ice in PBS/0.2% gelatin. Subsequently, cells were either left untreated or treated with permeabilization buffer according to manufacturer´s instructions (Affymetrix ebioscience). A subsequent second round of staining was performed on all cells as described above in PBS/0.2% gelatin or permeabilization buffer, respectively. Cells were washed twice with PBS (Pan Biotech) or permeablilization buffer, respectively, and analyzed by flow cytometry on a FACSCanto II (BD).
Dectin-Fc binding assay: Dectin-1-Fc and Dectin-2-Fc fusion proteins were generated as described previously20,46. The sequence encoding the extracellular domain of Dectin receptors were ligated into the expression vector pFuse-hIgG1-Fc (InvivoGen, San Diego, CA) and transiently transfected into CHO-S cells using the FreeStyle Max CHO-S Expression System (Life Technologies, Darmstadt, Germany). Supernatant containing soluble Dectin-fusion proteins were purified by affinity chromatography using a protein G column (GE Healthcare, Little Chalfont, United Kingdom). For ELISA-based binding assay, test antigens were coated in a concentration of 20 µg/ml in PBS on medium-binding half area 96-well microtiter plates (Greiner Bio-One, Kremsmünster, Austria) at 4 °C overnight. Wells were washed with 0.05% Tween 20 in PBS and blocked with 1% BSA in PBS at RT for 2 h. After further washing, Dectin-1-Fc and Dectin-2-Fc were added to respective wells at a concentration of 8,4 µg/ml in lectin buffer (50 mM HEPES, 5 mM MgCl2, 5 mM CaCl2, pH 7.4) at RT for 1 h, followed by incubation with peroxidase-conjugated anti-hFc antibody (Dianova, Hamburg, Germany) 1:5000 in reagent diluent (1% BSA, 0.05% Tween 20 in PBS) at RT for 1 h. Finally, colorimetric detection was performed using o-phenylenediamine dihydrochloride as substrate and subsequent measurement at 495 nm in a Multiskan GO spectrophotometer (Thermo Scientific, Waltham, Massachusetts, USA).
Statistics: Cytokine expression in response to different stimuli was analyzed by a one-way repeated measures F test (Friedman-test) with Dunns post-testing in order to correct for repeated measures. To calculate differences between receptor- or kinase-blocking and respective controls, non-parametric paired testing (Wilcoxon-matched pairs test) was applied due to non-gaussian distribution of data. Internalization of ligands compared to the negative control was analyzed by Wilcoxon-matched pairs test as well. Binding of candidate ligands to Dectin-1 was analyzed using a one-way ANOVA with Bonferroni post-testing. (GraphPad Prism 5; GraphPad Software, San Diego, CA). Differences were considered significant if p < 0.05.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplementary information
Author Contributions
L.M.R. wrote the main manuscript text and performed the experiments leading to figure 5. M.E., G.B. and P.K. performed the experiments leading to figures 1, 2. W.C. performed the experiments leading to figure 3. M.K.R. performed the experiments leading to figure 4. L.M.R., B.L. and T.W. designed the experiments.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
L. M. Roesner and M. Ernst contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-47769-2.
References
- 1.Kucuksezer UC, et al. Triggering of specific Toll-like receptors and proinflammatory cytokines breaks allergen-specific T-cell tolerance in human tonsils and peripheral blood. J Allergy Clin Immunol. 2013;131:875–885. doi: 10.1016/j.jaci.2012.10.051. [DOI] [PubMed] [Google Scholar]
- 2.Erridge C. Endogenous ligands of TLR2 and TLR4: agonists or assistants? J Leukoc Biol. 2010;87:989–999. doi: 10.1189/jlb.1209775. [DOI] [PubMed] [Google Scholar]
- 3.Miller LS, Modlin RL. Toll-like receptors in the skin. Semin Immunopathol. 2007;29:15–26. doi: 10.1007/s00281-007-0061-8. [DOI] [PubMed] [Google Scholar]
- 4.Werfel T, et al. Cellular and molecular immunologic mechanisms in patients with atopic dermatitis. J Allergy Clin Immunol. 2016;138:336–349. doi: 10.1016/j.jaci.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Glatz M, et al. Malassezia spp.-specific immunoglobulin E level is a marker for severity of atopic dermatitis in adults. Acta Derm Venereol. 2015;95:191–196. doi: 10.2340/00015555-1864. [DOI] [PubMed] [Google Scholar]
- 6.Darabi K, Hostetler SG, Bechtel MA, Zirwas M. The role of Malassezia in atopic dermatitis affecting the head and neck of adults. J Am Acad Dermatol. 2009;60:125–136. doi: 10.1016/j.jaad.2008.07.058. [DOI] [PubMed] [Google Scholar]
- 7.Ishikawa T, et al. Identification of distinct ligands for the C-type lectin receptors Mincle and Dectin-2 in the pathogenic fungus Malassezia. Cell Host Microbe. 2013;13:477–488. doi: 10.1016/j.chom.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Kistowska M, et al. Malassezia yeasts activate the NLRP3 inflammasome in antigen-presenting cells via Syk-kinase signalling. Exp Dermatol. 2014;23:884–889. doi: 10.1111/exd.12552. [DOI] [PubMed] [Google Scholar]
- 9.Yamasaki S, et al. Mincle is an ITAM-coupled activating receptor that senses damaged cells. Nat Immunol. 2008;9:1179–1188. doi: 10.1038/ni.1651. [DOI] [PubMed] [Google Scholar]
- 10.Fong JJ, et al. Immunomodulatory activity of extracellular Hsp70 mediated via paired receptors Siglec-5 and Siglec-14. Embo J. 2015;34:2775–2788. doi: 10.15252/embj.201591407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayer S, Raulf MK, Lepenies B. C-type lectins: their network and roles in pathogen recognition and immunity. Histochem Cell Biol. 2017;147:223–237. doi: 10.1007/s00418-016-1523-7. [DOI] [PubMed] [Google Scholar]
- 12.Rajaiah R, Moudgil KD. Heat-shock proteins can promote as well as regulate autoimmunity. Autoimmun Rev. 2009;8:388–393. doi: 10.1016/j.autrev.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Limacher A, et al. Cross-reactivity and 1.4-A crystal structure of Malassezia sympodialis thioredoxin (Mala s 13), a member of a new pan-allergen family. J Immunol. 2007;178:389–396. doi: 10.4049/jimmunol.178.1.389. [DOI] [PubMed] [Google Scholar]
- 14.Hradetzky Susanne, Roesner Lennart Matthias, Heratizadeh Annice, Crameri Reto, Garbani Mattia, Scheynius Annika, Werfel Thomas. Differential cytokine induction by the human skin–associated autoallergen thioredoxin in sensitized patients with atopic dermatitis and healthy control subjects. Journal of Allergy and Clinical Immunology. 2015;135(5):1378-1380.e5. doi: 10.1016/j.jaci.2014.10.038. [DOI] [PubMed] [Google Scholar]
- 15.Hradetzky, S. et al. In Exp Dermatol Vol. 22, e2–e47 (2013).
- 16.Sahaf B, Rosen A. Secretion of 10-kDa and 12-kDa thioredoxin species from blood monocytes and transformed leukocytes. Antioxid Redox Signal. 2000;2:717–726. doi: 10.1089/ars.2000.2.4-717. [DOI] [PubMed] [Google Scholar]
- 17.Li B, et al. Yeast glucan particles activate murine resident macrophages to secrete proinflammatory cytokines via MyD88- and Syk kinase-dependent pathways. Clin Immunol. 2007;124:170–181. doi: 10.1016/j.clim.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodridge HS, et al. Activation of the innate immune receptor Dectin-1 upon formation of a ‘phagocytic synapse’. Nature. 2011;472:471–475. doi: 10.1038/nature10071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dambuza IM, Brown GD. C-type lectins in immunity: recent developments. Curr Opin Immunol. 2015;32:21–27. doi: 10.1016/j.coi.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maglinao M, et al. A platform to screen for C-type lectin receptor-binding carbohydrates and their potential for cell-specific targeting and immune modulation. J Control Release. 2014;175:36–42. doi: 10.1016/j.jconrel.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 21.in Essentials of Glycobiology (eds nd et al.) (2009).
- 22.Mayer, S. et al. C-Type Lectin Receptor (CLR)–Fc Fusion Proteins As Tools to Screen for Novel CLR/Bacteria Interactions: An Exemplary Study on Preselected Campylobacter jejuni Isolates. Frontiers in Immunology9, 10.3389/fimmu.2018.00213 (2018). [DOI] [PMC free article] [PubMed]
- 23.Mayer C, et al. Humoral and cell-mediated autoimmune reactions to human acidic ribosomal P2 protein in individuals sensitized to Aspergillus fumigatus P2 protein. J Exp Med. 1999;189:1507–1512. doi: 10.1084/jem.189.9.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmid-Grendelmeier P, et al. IgE-mediated and T cell-mediated autoimmunity against manganese superoxide dismutase in atopic dermatitis. J Allergy Clin Immunol. 2005;115:1068–1075. doi: 10.1016/j.jaci.2005.01.065. [DOI] [PubMed] [Google Scholar]
- 25.Shankar Jata, Cerqueira Gustavo C., Wortman Jennifer R., Clemons Karl V., Stevens David A. RNA-Seq Profile Reveals Th-1 and Th-17-Type of Immune Responses in Mice Infected Systemically with Aspergillus fumigatus. Mycopathologia. 2018;183(4):645–658. doi: 10.1007/s11046-018-0254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsons MW, et al. Dectin-2 regulates the effector phase of house dust mite-elicited pulmonary inflammation independently from its role in sensitization. J Immunol. 2014;192:1361–1371. doi: 10.4049/jimmunol.1301809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ito T, et al. Dectin-1 Plays an Important Role in House Dust Mite-Induced Allergic Airway Inflammation through the Activation of CD11b+ Dendritic Cells. J Immunol. 2017;198:61–70. doi: 10.4049/jimmunol.1502393. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Z, et al. beta-Glucan exacerbates allergic asthma independent of fungal sensitization and promotes steroid-resistant TH2/TH17 responses. J Allergy Clin Immunol. 2017;139:54–65 e58. doi: 10.1016/j.jaci.2016.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ito T, Hirose K, Norimoto A, Saku A, Nakajima H. Dectin-1 plays a critical role in HDM-induced PGE2 production in macrophages. Allergol Int. 2017;66S:S44–S46. doi: 10.1016/j.alit.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Barrett NA, et al. Dectin-2 mediates Th2 immunity through the generation of cysteinyl leukotrienes. J Exp Med. 2011;208:593–604. doi: 10.1084/jem.20100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clarke DL, et al. Dectin-2 sensing of house dust mite is critical for the initiation of airway inflammation. Mucosal Immunol. 2014;7:558–567. doi: 10.1038/mi.2013.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Norimoto A, et al. Dectin-2 promotes house dust mite-induced T helper type 2 and type 17 cell differentiation and allergic airway inflammation in mice. Am J Respir Cell Mol Biol. 2014;51:201–209. doi: 10.1165/rcmb.2013-0522OC. [DOI] [PubMed] [Google Scholar]
- 33.Roesner LM, et al. Der p1 and Der p2-Specific T Cells Display a Th2, Th17, and Th2/Th17 Phenotype in Atopic Dermatitis. J Invest Dermatol. 2015;135:2324–2327. doi: 10.1038/jid.2015.162. [DOI] [PubMed] [Google Scholar]
- 34.Stritesky GL, Yeh N, Kaplan MH. IL-23 promotes maintenance but not commitment to the Th17 lineage. J Immunol. 2008;181:5948–5955. doi: 10.4049/jimmunol.181.9.5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caucheteux SM, et al. IL-1beta enhances inflammatory TH2 differentiation. J Allergy Clin Immunol. 2016;138:898–901 e894. doi: 10.1016/j.jaci.2016.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang JG, et al. The dendritic cell receptor Clec9A binds damaged cells via exposed actin filaments. Immunity. 2012;36:646–657. doi: 10.1016/j.immuni.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 37.Delneste Y, et al. Involvement of LOX-1 in dendritic cell-mediated antigen cross-presentation. Immunity. 2002;17:353–362. doi: 10.1016/S1074-7613(02)00388-6. [DOI] [PubMed] [Google Scholar]
- 38.Ferwerda G, Meyer-Wentrup F, Kullberg BJ, Netea MG, Adema GJ. Dectin-1 synergizes with TLR2 and TLR4 for cytokine production in human primary monocytes and macrophages. Cell Microbiol. 2008;10:2058–2066. doi: 10.1111/j.1462-5822.2008.01188.x. [DOI] [PubMed] [Google Scholar]
- 39.Dragicevic A, et al. Signaling through Toll-like receptor 3 and Dectin-1 potentiates the capability of human monocyte-derived dendritic cells to promote T-helper 1 and T-helper 17 immune responses. Cytotherapy. 2012;14:598–607. doi: 10.3109/14653249.2012.667873. [DOI] [PubMed] [Google Scholar]
- 40.Zhu LL, et al. C-type lectin receptors Dectin-3 and Dectin-2 form a heterodimeric pattern-recognition receptor for host defense against fungal infection. Immunity. 2013;39:324–334. doi: 10.1016/j.immuni.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 41.Wevers BA, et al. Fungal engagement of the C-type lectin mincle suppresses dectin-1-induced antifungal immunity. Cell Host Microbe. 2014;15:494–505. doi: 10.1016/j.chom.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 42.Eyerich K, et al. IL-17 in atopic eczema: linking allergen-specific adaptive and microbial-triggered innate immune response. J Allergy Clin Immunol. 2009;123:59–66 e54. doi: 10.1016/j.jaci.2008.10.031. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi M, et al. Expression of toll-like receptor 2, NOD2 and dectin-1 and stimulatory effects of their ligands and histamine in normal human keratinocytes. Br J Dermatol. 2009;160:297–304. doi: 10.1111/j.1365-2133.2008.08897.x. [DOI] [PubMed] [Google Scholar]
- 44.Crameri R, et al. Humoral and cell-mediated autoimmunity in allergy to Aspergillus fumigatus. J Exp Med. 1996;184:265–270. doi: 10.1084/jem.184.1.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reginald Kavita, Westritschnig Kerstin, Linhart Birgit, Focke-Tejkl Margarete, Jahn-Schmid Beatrice, Eckl-Dorna Julia, Heratizadeh Annice, Stöcklinger Angelika, Balic Nadja, Spitzauer Susanne, Niederberger Verena, Werfel Thomas, Thalhamer Josef, Weidinger Stephan, Novak Natalija, Ollert Markus, Hirschl Alexander M., Valenta Rudolf. Staphylococcus aureus fibronectin-binding protein specifically binds IgE from patients with atopic dermatitis and requires antigen presentation for cellular immune responses. Journal of Allergy and Clinical Immunology. 2011;128(1):82-91.e8. doi: 10.1016/j.jaci.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 46.Monteiro João T., Schön Kathleen, Ebbecke Tim, Goethe Ralph, Ruland Jürgen, Baumgärtner Wolfgang, Becker Stefanie C., Lepenies Bernd. The CARD9-Associated C-Type Lectin, Mincle, Recognizes La Crosse Virus (LACV) but Plays a Limited Role in Early Antiviral Responses against LACV. Viruses. 2019;11(3):303. doi: 10.3390/v11030303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.