Figure 1.
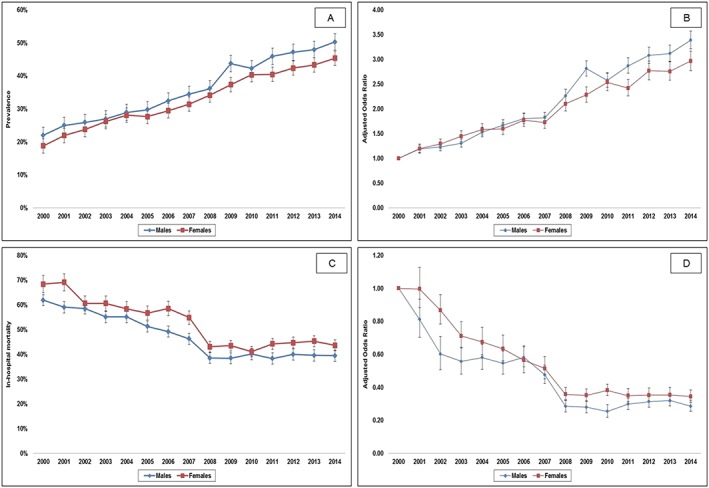
Unadjusted and adjusted 15 year temporal trends for the prevalence and in‐hospital mortality of AKI stratified by sex in AMI‐CS. (A) Unadjusted temporal trends of AKI stratified by sex in AMI‐CS (P < 0.001 for trend); (B) adjusted temporal trends of AKI stratified by sex in AMI‐CS* (P < 0.001 for trend); (C) unadjusted temporal trends in the in‐hospital mortality of AKI stratified by sex in AMI‐CS (P < 0.001 for trend); and (D) adjusted temporal trends of in‐hospital mortality of AKI stratified by sex in AMI‐CS^ (P < 0.001 for trend). *Adjusted for age, race, primary payer, socio‐economic status, hospital location/teaching status, hospital bedsize, hospital region, and co‐morbidity (referent year 2000). ^Adjusted for age, race, primary payer, socio‐economic status, hospital location/teaching status, hospital bedsize, hospital region, co‐morbidity, acute respiratory failure, acute hepatic failure, acute haematologic failure, acute neurologic failure, cardiac arrest, type of AMI, use of coronary angiography, percutaneous coronary intervention, invasive haemodynamic monitoring, mechanical circulatory support, invasive mechanical ventilation, and haemodialysis (referent year 2000). AKI, acute kidney injury; AMI‐CS, acute myocardial infarction‐related cardiogenic shock.
