Abstract
Background.
Alcohol consumption in later life has increased in the past decade, and the relationship between alcohol consumption and mortality is controversial. Recent studies suggest little, if any, health benefit to alcohol. Yet most rely on single time-point consumption assessments, and minimal confounder adjustments.
Methods.
We report on 16 years of follow-up from the Health and Retirement Study (HRS) cohorts born 1931–1941 (N=7,904, baseline mean age=61, SD=3.18). Respondents were queried about drinking frequency/quantity. Mortality was established via exit interviews and confirmed with the national death index. Time-varying confounders included but were not limited to household assets, smoking, BMI, health/functioning, depression, chronic disease; time-invariant confounders included baseline age, education, sex, race.
Results.
After adjustment, current abstainers had the highest risk of subsequent mortality, consistent with sick quitters, and moderate (Men: HR=0.74, 95% C.I. 0.60–0.91; women: HR=0.82, 95% C.I. 0.63–1.07) drinking was associated with a lower mortality rate compared with occasional drinking, though smokers and men evidenced less of an inverse association. Quantitative bias analyses indicated that omitted confounders would need to be associated with ~4-fold increases in mortality rates for men and ~9-fold increases for women to change the results.
Conclusions.
There are consistent associations between moderate/occasional drinking and lower mortality, though residual confounding remains a threat to validity. Continued efforts to conduct large-scale observational studies of alcohol consumption and mortality are needed to characterize the changing patterns of consumption in older age.
Keywords: alcohol consumption, older adults, health and retirement study, mortality, moderate drinking
Introduction
The nature of the relationship between moderate drinking and mortality remains controversial. Moderate drinkers have lower mortality rates than abstainers and heavy drinkers (Brien et al., 2011; Di Castelnuovo et al., 2006; Thun et al., 1997), and evidence suggests that small amounts of alcohol may have beneficial effects on high-density lipoprotein cholesterol and cardiovascular health (Zhao et al., 2017), especially cardio-atherosclerotic disease (Bagnardi et al., 2013; Nurmi et al., 2013; Rehm et al., 2016a, 2006) at older ages. Occasional or moderate drinking is associated with a reduced risk to die from ischemic heart disease and stroke over age 60, (Blomster et al., 2014; Leong et al., 2014; Liang et al., 2012) compared with heavy drinking and complete alcohol abstention. Randomized trials find that small amounts of alcohol are associated with better cardiometabolic profiles among diabetic and stroke patients (Gepner et al., 2015; Rist et al., 2010), though sample sizes are small, benefits were only found for specific subgroups, and results may not generalize to those who have not yet experienced adverse events.
While the protective association between moderate consumption and mortality for older adults is well-replicated, experts continue to debate its validity (Connor, 2006; Greenfield and Kerr, 2014; Kerr et al., 2011; Keyes and Miech, 2013; Rehm et al., 2008; Wannamethee and Shaper, 1998), and consensus on these debates has important public health impact, given the widespread consumption of alcohol in the US (Greenfield and Kerr, 2014; Rehm et al., 2016b). Relative to abstainers and heavy drinkers, moderate drinkers are wealthier and present more protective factors for cardiometabolic health (Cerdá et al., 2011; Dawson et al., 2013; French et al., 2009; Lang et al., 2007; Naimi et al., 2005; Rehm et al., 2009; Skog, 1985), and many studies do not have comprehensive information sufficient for confounder control. Further, the extent to which associations arise because of reverse causation (individuals reducing consumption due to illness) remains a threat to validity (Licaj et al., 2016; Ortolá et al., 2018; Stockwell et al., 2016). An instrumental variable approach like Mendelian randomization, which does not rely on standard confounder control, demonstrates little evidence for a protective effect of moderate consumption on cardiovascular disease (Cho et al., 2016; Holmes et al., 2014; Millwood et al., 2019; Taylor et al., 2015).
Further, among studies that demonstrate an inverse association between moderate intake and alcohol, the association is not uniform. Previous research has found that the association is lower among African Americans and women compared with Whites and men (Fuchs et al., 2004; Rehm and Sempos, 1995; Sempos et al., 2003), as well as those with specific genetic polymorphisms (Gepner et al., 2015). However, existing evidence is based on either single time points of alcohol consumption, or in the case of genetic analyses, small sample sizes.
Finally, most epidemiological studies of alcohol and mortality have used single-time assessments of drinking, thus not able to assess the dynamics of consumption over time (Connor, 2006; Fillmore et al., 2007; Rehm et al., 2009). Indeed, a recent review and meta-analysis indicated that of over 80 studies that have examined alcohol consumption and death, only six were classified as meeting basic benchmarks of epidemiological rigor; of those six, only three had longitudinal information on consumption (Stockwell et al., 2016); those six showed little evidence for a mortality benefit of moderate consumption. Indeed, several scholars have suggested that observational studies simply cannot address questions of the relationship between alcohol consumption and mortality, given inherent biases in observational data, competing risks, and measurement error (Rehm, 2019), though methods and data quality are consistently improving, suggesting that continued focus on better uses of observational data is worth pursuing.
The largest study in the United States to assess the relationship between alcohol consumption and mortality has been the Health and Retirement Study (HRS), the data source we use in the present investigation. Previous analyses of HRS do not have consistent findings, with some analyses demonstrating no benefit to moderate drinking (Goulden, 2016) and others showing a protective effect (Nandi et al., 2014; Shaw and Agahi, 2012). However, existing analyses of HRS have not included data past 2012 and have not sufficiently included a broad range of time-varying alcohol exposures as well as time-varying confounders; inclusion of recent waves is informative as they include more deaths, and span the time period in which alcohol consumption has been increasing among older adults (Grucza et al., 2018). Thus, the present study builds on an existing evidence using HRS data to extend previous findings.
Alcohol consumption is increasing in the US, especially among adults over 60 (although it is still lower than at earlier ages (Breslow et al., 2017). Clarifying the relationship between alcohol consumption and health for older adults is thus increasingly important to achieve public health goals. As the population is living longer lives, individuals, physicians, and other stakeholders require rigorous science on the role of alcohol in promoting or deteriorating health later in life. Assessment of these risks, and how they vary by subgroups, can provide illumination on this controversial literature. The present study reports on longitudinal data from the Health and Retirement Study (HRS) from 1998 through 2014, a longitudinal, nationally-representative cohort of men and women in the US, to assess the relationship between alcohol consumption and mortality using time-varying indicators of alcohol consumption, adjustment for multiple (time-varying and constant) confounders, and assessment of heterogeneity of effects across covariates.
Materials and Methods
Sample.
The HRS is a longitudinal study of Americans over the age of 50 and their spouses. The present study draws on data from the HRS cohort interviewed biannually across the 9 waves between 1998 and 2014. The HRS cohort was originally followed starting in 1992; however, detailed alcohol consumption was consistently measured starting in 1998, thus, 1998 is the year at which we begin our time-varying assessment. However, we consider information prior to 1998 to separate current from life-time abstainers based on the questions in those surveys. Our sample includes individuals born in 1931–1941 who were included in the original HRS 1992 cohort, and responded to our baseline 1998 wave (baseline mean age=61, SD=3.18). The final sample size was 7,904, and demographic as well as other characteristics included as covariates in the present study, by gender, are described in Table 1.
Table 1:
Baseline covariates in a nationally representative longitudinal sample of adults over age 56 in the United States (N total=7,904; N men=3,619; N women=4,285) followed for an average of 15 years.
| Total sample | Men | Women | χ2, p for differences between men and women | ||
|---|---|---|---|---|---|
| N (%); mean (SD) | N (%); mean (SD) | N (%); mean (SD) | |||
| Drinking Status | Lifetime abstainer | 2,487 (31.6) | 846 (23.5) | 1,641 (38.4) | 385.02, <0.01 |
| Current abstainer | 1,513 (19.2) | 660 (18.3) | 853 (19.9) | ||
| Occasional drinker | 1,384 (17.6) | 584 (16.2) | 800 (18.7) | ||
| Moderate drinker | 2,257 (28.6) | 1,337 (37.1) | 920 (21.5) | ||
| Heavy drinker | 238 (3.0) | 174 (4.8) | 64 (1.5) | ||
| Age | Continuous | 61.24 (3.18) | 61.26 (3.17) | 61.23 (3.19) | |
| Education | Lt high school | 2,008 (25.4) | 875 (24.2) | 1,133 (26.4) | 106.94, <0.01 |
| GED | 395 (5.0) | 203 (5.6) | 192 (4.5) | ||
| High-school graduate | 2,593 (32.8) | 1,055 (29.2) | 1,538 (35.9) | ||
| Some college | 1,535 (19.4) | 702 (19.4) | 833 (19.4) | ||
| College and above | 1,373 (17.4) | 784 (21.7) | 589 (13.7) | ||
| Race/Ethnicity | White non-Hispanic | 5,798 (73.4) | 2,737 (75.6) | 3,061 (71.4) | 25.52, <0.01 |
| Black non-Hispanic | 1,266 (16) | 499 (13.8) | 767 (17.9) | ||
| Other non-Hispanic | 148 (1.9) | 69 (1.9) | 79 (1.8) | ||
| Hispanic | 691 (8.7) | 313 (8.7) | 378 (8.8) | ||
| Wealth | Scaled | 0 (1) | 0.02 (1.11) | −0.02 (0.90) | |
| Smoking | Never smoked | 2,940 (37.2) | 954 (26.4) | 1,986 (46.3) | 358.93, <0.01 |
| Former smoker | 3,380 (42.8) | 1,894 (52.3) | 1,486 (34.7) | ||
| Current smoker | 1,583 (20) | 770 (21.3) | 813 (19) | ||
| BMI | Underweight | 111 (1.4) | 31 (0.9) | 80 (1.9) | 149.5, <0.01 |
| Normal | 2,391 (30.6) | 922 (25.5) | 1,469 (34.9) | ||
| Overweight | 3,185 (40.7) | 1,715 (47.5) | 1,470 (34.9) | ||
| Obese | 2,137 (27.3) | 944 (26.1) | 1,193 (28.3) | ||
| ADL difficulties | 0 | 6,889 (87.2) | 3,220 (89) | 3,669 (85.7) | 21.44, <0.01 |
| 1 | 523 (6.6) | 210 (5.8) | 313 (7.3) | ||
| 2 | 217 (2.7) | 90 (2.5) | 127 (3.0) | ||
| 3 | 135 (1.7) | 46 (1.3) | 89 (2.1) | ||
| 4 | 86 (1.1) | 36 (1.0) | 50 (1.2) | ||
| 5 | 47 (0.6) | 16 (0.4) | 31 (0.7) | ||
| Depressive symptoms | Continuous | 1.58 (1.99) | 1.33 (1.78) | 1.78 (2.11) | |
| Arthritis | No | 7,513 (95.1) | 3,416 (94.4) | 4,097 (95.7) | 5.95, 0.01 |
| Yes | 387 (4.9) | 201 (5.6) | 186 (4.3) | ||
| Cancer | No | 7,736 (98.0) | 3,516 (97.4) | 4,220 (98.6) | 15.39, <0.01 |
| Yes | 154 (2.0) | 95 (2.6) | 59 (1.4) | ||
| Diabetes | No | 7,740 (98.0) | 3,531 (97.7) | 4,209 (98.3) | 3.54, 0.06 |
| Yes | 155 (2.0) | 83 (2.3) | 72 (1.7) | ||
| Heart disease | No | 7702 (97.5) | 3,501 (96.8) | 4,201 (98.1) | 11.89, <0.01 |
| Yes | 198 (2.5) | 115 (3.2) | 83 (1.9) | ||
| Stroke | No | 7,823 (99.0) | 3,577 (98.9) | 4,246 (99.1) | 0.57, 0.45 |
| Yes | 79 (1.0) | 40 (1.1) | 39 (0.9) | ||
| High blood pressure | No | 7,560 (95.7) | 3,466 (95.9) | 4,094 (95.6) | 0.18, 0.67 |
| Yes | 337 (4.3) | 150 (4.1) | 187 (4.4) | ||
| Lung disease | No | 7,803 (98.8) | 3,577 (98.9) | 4,226 (98.6) | 1.01, 0.32 |
| Yes | 97 (1.2) | 39 (1.1) | 58 (1.4) | ||
| Psychiatric problems | No | 7,782 (98.5) | 3,566 (98.7) | 4,216 (98.4) | 0.74, 0.39 |
| Yes | 116 (1.5) | 48 (1.3) | 68 (1.6) | ||
Measures.
Alcohol consumption.
Alcohol consumption was queried between 1992 and 1996, but were useful only to distinguish life-time from current abstainers at subsequent waves due to wording changes. Since 1998, respondents who reported consumption were queried about drinking frequency (i.e., average number of days per week alcohol was consumed in the last three months) and quantity (i.e., average number of drinks consumed on drinking days). Respondents were also asked how many days they had four or more drinks on one occasion in the last three months (binge drinking). Combining the HRS questions on binge drinking and quantity of drinks, we calculated binge drinking based on standard definitions as drinking over five drinks in a single day for men and over four drinks in a single day for women. We also calculated the average number of drinks per day by multiplying frequency and quantity and dividing the product by seven. Based on this information, respondents were classified into five groups at 1998 and following waves: lifetime abstainers, current abstainers, heavy drinkers, moderate drinkers, and occasional drinkers. Lifetime abstainers had less than 12 drinks in their lifetime. Current abstainers did not drink in the current wave, but drank in the past or we cannot rule out that they drank in the past. The degree of drinking was classified using conventional gender specific thresholds for drinks per day and binge drinking in a single day in the past three months. Heavy drinkers were defined for men as consuming more than three drinks per day or binging more than five drinks in a single day, and for women as consuming more than two drinks per day or binging more than four drinks in a single day. Moderate drinkers were defined as drinking one to two (women) or one to three (men) drinks one or more days per week, and not binging more than five drinks in a single day for men or more than four drinks in a single day for women. Occasional drinkers were defined as drinking less than one day per week (e.g. once or twice per month), not binging more than five drinks in a single day for men or more than four drinks in a single day for women, and drinking a maximum of three drinks per day for men and a maximum of two drinks per day for women. Using this categorical variable, we examined both baseline and time-varying drinking status.
Online Tables 1 and 2 provide descriptive analysis of the proportion of respondents who changed drinking status after baseline, stratified by baseline drinking status. For example, among men who reported heavy drinking at baseline, 37.4% had at least one subsequent time point in which they reported currently abstaining, 23.6% had at least one subsequent time point in which they reported occasional drinking, and 66.7% had at least one subsequent time point in which they reported moderate drinking. Among women who reported heavy drinking at baseline, 31.3% had at least one subsequent time point in which they reported currently abstaining, 21.9% had at least one subsequent time point in which they reported occasional drinking, and 71.9% had at least one subsequent time point in which they reported moderate drinking. In summary, there were substantial transitions over time in drinking status, among both men and women.
Mortality.
Respondent deaths were ascertained via study tracking and by linkage with the National Death Index (NDI). If both NDI and HRS interview reported death dates were present, precedence was given to the NDI date (Weir, 2016). If no NDI record was present, HRS interview death date was used. Among the 2,399 reported deaths in our sample, 78% had a confirmed NDI record. HRS has not released NDI-matched records after 2011, thus only the interview reported-death data were used. Death information is updated following each wave of data collection.
Time-invariant covariates.
We included gender, baseline age, education (less than high school, GED, high school graduate, some college, and college and above), and race/ethnicity (White non-Hispanic, Black non-Hispanic, Other non-Hispanic, and Hispanic), as time-invariant covariates.
Time-varying covariates.
We included a wide range of time-varying self-reported covariates. We calculated total respondent wealth dividing total value of all household assets by number of household members and adjusting for Consumer Price Index inflation (Bureau of Labor Statistics, 2018). Smoking status was coded as current, former, and never smoker. Using body mass index (BMI), we classified individuals as underweight (BMI<18.5), normal (18.5 to 24.9), overweight (25.0 to 29.9), and obese (30.0 and above). We measured health and function, including a count of difficulties with activities of daily living (walking across a room, getting in and out of bed, dressing, bathing, and eating), an 8-item reduced version of the Center for Epidemiologic Studies Depression (CES-D) scale (Andresen et al., 1994; Radloff, 1977), and a set of nine dichotomies indicating doctor-diagnosed onset of chronic diseases since previous wave (arthritis, cancer, diabetes, heart problems, stroke, high blood pressure, lung disease, and psychiatric problems).
Statistical analyses.
All analyses were stratified by gender. We began by examining survival curves for mortality based on baseline alcohol consumption category, for the overall sample. For individuals lost to follow-up, censoring time was estimated as the midpoint between the last observation time and the first missed observation. We then proceeded to estimate Cox proportional hazards models, both unadjusted and including all aforementioned time-invariant and time-varying covariates, including alcohol consumption at each wave as time-variant. Proportionality assumptions were tested; due to the complexity of the models, proportionality was marginal for some models, which should be considered a limitation. We sequentially included covariates in models, beginning with a model controlled for demographics, and iteratively adding health behavior, as well as chronic conditions (which could be both a cause of alcohol consumption, if individuals reduce drinking due to chronic disease, and a consequence of alcohol consumption, given that heavy alcohol use causes many chronic diseases). In these time varying cox proportional hazards models, respondents were included if they had at least one wave of data for each time varying covariate. For the unadjusted model this N was 7,902. For the combined models 1, 2, and 3, the respective N’s were 7,902, 7,886, and 7,601. Finally, we tested the multiplicative interaction between each covariate and baseline alcohol consumption categories in predicting mortality rates. We report beta estimates and hazard ratios, standard errors, and 95% confidence intervals. Follow-up analyses were conducted with gender and smoking interactions in the model given the strength of the interaction association. Analyses were done using Stata v15 and R software.
Additionally, we performed quantitative bias analysis (QBA) to assess how much unmeasured confounding would need to be present in order to explain the observed results (Greenland and Lash, 2008; Lash et al., 2014, 2009). At core, QBA approaches are built on the notion that we cannot rely on the estimates from observational studies to be causal. While modern statistics are well-adept at evaluating the extent to which random error and chance explain patterns of observed data, these traditional statistics are not adept at evaluating the extent to which systematic error and bias explain results. We assessed the extent to which unmeasured confounding explained our findings by varying two parameters: the strength of the association between the unknown and/or unmeasured confounders and mortality, and the distribution of these confounders between moderate consumers and abstainers. Because alcohol consumption was time-varying, we examined unequal distributions of person-time between moderate consumers and abstainers. For each scenario we conducted 1,000 simulations. We estimated two different scenarios. First, we assumed that omitted confounders would be twice as prevalent among abstainers compared with occasional drinkers (20% versus 10%); second, we assumed that omitted confounders would be three times more prevalent among abstainers compared with occasional drinkers (30% versus 10%). We report the median, the 2.5th, and the 97.5th percentile of the distribution, as well as the percentage of simulations in which we would come to a different conclusion about the relationship between alcohol consumption and mortality than is reported in our results. All code for our QBA is provided in an online supplement.
Results
Figure 1 shows the Kaplan Meier curves for baseline alcohol consumption and subsequent mortality, by sex. There were survival differences across consumption categories among both men (Wald chi-square = 76.7, df = 4) and women (Wald chi-square = 71.1, df = 4). Among men, heavy drinkers had the lowest survival until approximately 100 months (~8–9 years) after baseline, after which current abstainers had the lowest survival. Among women, current abstainers had the lowest survival throughout the study period, although rates between current, lifetime abstainers, and heavy drinkers converged at the end of the study period.
Figure 1.
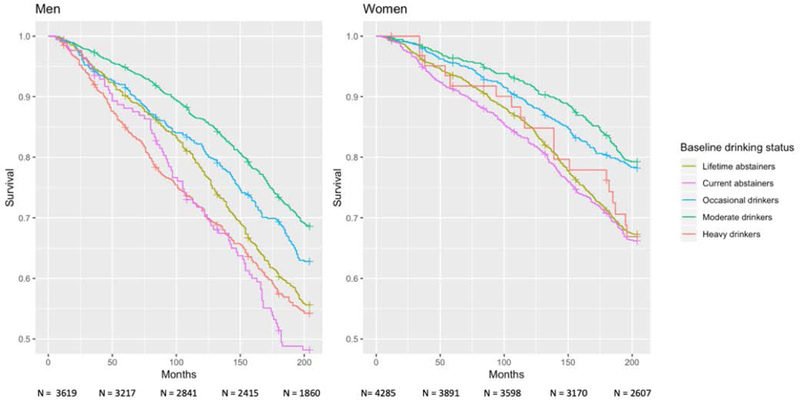
Mortality by baseline alcohol consumption category in a longitudinal sample of adults over 56 in the United States (N men=3,601; N women=4,278).
We proceeded to model alcohol consumption as a time-varying exposure and tested the association with mortality. Unadjusted results reported in Table 2 show that relative to occasional drinking, lifetime abstaining for women (men: HR=1.19, 95% C.I. 0.99–1.44; women: HR=1.71 95% C.I. 1.41–2.07), and current abstaining for men and women (men: HR=1.73, 95% C.I. 1.46–2.05; women: HR=1.98 95% C.I. 1.63–2.41), were associated with higher mortality, while moderate drinking was associated with lower mortality rates for men and women (men: HR=0.65, 95% C.I. 0.54–0.78; women: HR=0.71, 95% C.I. 0.56–0.91). Heavy drinkers on average did not have meaningfully different mortality rates than occasional drinkers.
Table 2:
Unadjusted mortality hazard ratios in a nationally representative longitudinal sample of adults over age 56 in the United States (N total=7,902; N men=3,617; N women=4,285) followed for an average of 15 years.
| Men | Women | |
|---|---|---|
| HR (95% CI) | HR (95% CI) | |
| Drinking Status | ||
| Lifetime abstainer | 1.19 (0.99, 1.44) | 1.71 (1.41, 2.07) |
| Current abstainer | 1.73 (1.46, 2.05) | 1.98 (1.63, 2.41) |
| Occasional drinker | REF | REF |
| Moderate drinker | 0.65 (0.54, 0.78) | 0.71 (0.56, 0.91) |
| Heavy drinker | 1.20 (0.88, 1.64) | 1.11 (0.59, 2.11) |
Drinking status based on time-varying variable for each participant at each wave.
Table 3a and 3b report adjusted results on the association between time-varying alcohol consumption and mortality, sequentially including both time-invariant and time-varying covariates among men (Table 3a) and among women (Table 3b). We report results controlled for demographics in model 1, adding health behaviors in model 2, adding chronic health conditions in model 3. Separating models 2 and 3 is particularly important as chronic health conditions may be mediating the association between alcohol consumption and mortality.
Table 3a:
Adjusted mortality hazard ratios in a nationally representative longitudinal sample of adults over 56 in the United States followed for an average of 15 years (men only).
| Model 1 (Demographics) | Model 2 (Demographics + health behaviors) | Model 3 (Demographics + health behaviors + chronic health conditions) | ||
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Drinking Status | Lifetime abstainer | 1.13 (0.93, 1.36) | 1.14 (0.94, 1.39) | 1.08 (0.87, 1.34) |
| Current abstainer | 1.60 (1.34, 1.89) | 1.50 (1.26, 1.80) | 1.25 (1.02, 1.53) | |
| Occasional drinker | REF | REF | REF | |
| Moderate drinker | 0.69 (0.57, 0.83) | 0.67 (0.55, 0.81) | 0.74 (0.60, 0.91) | |
| Heavy drinker | 1.23 (0.90, 1.68) | 1.04 (0.76, 1.44) | 0.97 (0.68, 1.40) | |
| Age | Continuous | 1.08 (1.06, 1.10) | 1.08 (1.06, 1.10) | 1.07 (1.05, 1.09) |
| Education | Lt high school | REF | REF | REF |
| GED | 0.79 (0.62, 1.01) | 0.79 (0.61, 1.01) | 0.79 (0.59, 1.05) | |
| High-school graduate | 0.71 (0.62, 0.83) | 0.77 (0.66, 0.90) | 0.89 (0.74, 1.07) | |
| Some college | 0.91 (0.77, 1.07) | 0.96 (0.81, 1.14) | 1.08 (0.89, 1.31) | |
| College and above | 0.60 (0.49, 0.72) | 0.63 (0.51, 0.77) | 0.75 (0.60, 0.94) | |
| Race/Ethnicity | White non-Hispanic | REF | REF | REF |
| Black non-Hispanic | 1.23 (1.06, 1.43) | 1.11 (0.95, 1.30) | 1.02 (0.84, 1.23) | |
| Other non-Hispanic | 0.98 (0.65, 1.47) | 0.89 (0.58, 1.37) | 0.84 (0.51, 1.38) | |
| Hispanic | 0.82 (0.67, 1.01) | 0.86 (0.69, 1.07) | 0.74 (0.57, 0.96) | |
| Wealth | Scaled | 0.79 (0.69, 0.92) | 0.85 (0.74, 0.98) | 0.86 (0.74, 1.00) |
| Smoking | Never smoked | REF | REF | |
| Former smoker | 1.57 (1.34, 1.84) | 1.51 (1.26, 1.80) | ||
| Current smoker | 2.10 (1.74, 2.55) | 2.12 (1.71, 2.63) | ||
| BMI | Underweight | 3.63 (2.72, 4.84) | 2.43 (1.61, 3.67) | |
| Normal | REF | REF | ||
| Overweight | 0.63 (0.55, 0.72) | 0.72 (0.62, 0.84) | ||
| Obese | 0.66 (0.56, 0.77) | 0.71 (0.59, 0.84) | ||
| ADL difficulties | 0 | REF | ||
| 1 | 1.79 (1.47, 2.19) | |||
| 2 | 2.83 (2.20, 3.63) | |||
| 3 | 2.08 (1.41, 3.06) | |||
| 4 | 3.31 (2.25, 4.86) | |||
| 5 | 2.68 (1.47, 4.90) | |||
| Depressive symptoms | Continuous | 1.10 (1.06, 1.13) | ||
| Arthritis | No | REF | ||
| Yes | 1.42 (1.06, 1.89) | |||
| Cancer | No | REF | ||
| Yes | 3.31 (2.67, 4.09) | |||
| Diabetes | No | REF | ||
| Yes | 1.35 (0.97, 1.88) | |||
| Heart disease | No | REF | ||
| Yes | 1.34 (1.01, 1.78) | |||
| Stroke | No | REF | ||
| Yes | 1.40 (0.98, 1.98) | |||
| High blood pressure | No | REF | ||
| Yes | 0.91 (0.67, 1.25) | |||
| Lung disease | No | REF | ||
| Yes | 1.83 (1.34, 2.50) | |||
| Psychiatric problems | No | REF | ||
| Yes | 1.65 (1.12, 2.42) | |||
Hazard ratios derived from a Cox proportional hazard model with the following covariates: time-varying covariates of alcohol consumption category, gender, age at baseline, race, wealth, smoking, BMI, difficulties in activities of daily living, depressive symptoms based on Center for Epidemiologic Studies Depression Scale (CES-D), arthritis since previous wave, cancer since previous wave, diabetes since previous wave, heart disease since previous wave, stroke since previous wave, high blood pressure since previous wave, lung disease since previous wave, and psychiatric problem since previous wave. (Model 1 N=3,617; Model 2 N=3,615; Model 3 N=3,401).
Table 3b:
Adjusted mortality hazard ratios in a nationally representative longitudinal sample of adults over 56 in the United States followed for an average of 15 years (women only).
| Model 1 (Demographics) | Model 2 (Demographics + health behaviors) | Model 3 (Demographics + health behaviors + chronic health conditions) | ||
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Drinking Status | Lifetime abstainer | 1.44 (1.19, 1.76) | 1.60 (1.31, 1.97) | 1.35 (1.08, 1.68) |
| Current abstainer | 1.74 (1.43, 2.12) | 1.71 (1.39, 2.10) | 1.34 (1.08, 1.67) | |
| Occasional drinker | REF | REF | REF | |
| Moderate drinker | 0.79 (0.62, 1.01) | 0.77 (0.60, 0.99) | 0.82 (0.63, 1.07) | |
| Heavy drinker | 1.25 (0.66, 2.38) | 1.11 (0.58, 2.13) | 1.07 (0.54, 2.11) | |
| Age | Continuous | 1.08 (1.06, 1.10) | 1.08 (1.06, 1.10) | 1.06 (1.04, 1.08) |
| Education | Lt high school | REF | REF | REF |
| GED | 0.62 (0.46, 0.83) | 0.72 (0.53, 0.97) | 0.78 (0.56, 1.08) | |
| High-school graduate | 0.65 (0.56, 0.75) | 0.70 (0.60, 0.82) | 0.88 (0.74, 1.04) | |
| Some college | 0.62 (0.51, 0.74) | 0.68 (0.57, 0.83) | 0.85 (0.69, 1.05) | |
| College and above | 0.46 (0.36, 0.59) | 0.50 (0.39, 0.65) | 0.60 (0.45, 0.80) | |
| Race/Ethnicity | White non-Hispanic | REF | REF | REF |
| Black non-Hispanic | 1.04 (0.90, 1.21) | 1.10 (0.94, 1.28) | 1.08 (0.91, 1.28) | |
| Other non-Hispanic | 0.71 (0.43, 1.16) | 0.76 (0.46, 1.25) | 0.86 (0.52, 1.45) | |
| Hispanic | 0.59 (0.47, 0.75) | 0.67 (0.52, 0.86) | 0.62 (0.47, 0.82) | |
| Wealth | Scaled | 0.57 (0.45, 0.73) | 0.61 (0.48, 0.78) | 0.79 (0.64, 0.97) |
| Smoking | Never smoked | REF | REF | |
| Former smoker | 1.93 (1.67, 2.23) | 1.71 (1.46, 2.00) | ||
| Current smoker | 2.35 (1.96, 2.82) | 2.45 (2.01, 2.98) | ||
| BMI | Underweight | 2.93 (2.29, 3.76) | 2.66 (2.00, 3.54) | |
| Normal | REF | REF | ||
| Overweight | 0.69 (0.59, 0.81) | 0.75 (0.63, 0.89) | ||
| Obese | 0.84 (0.72, 0.99) | 0.74 (0.62, 0.88) | ||
| ADL difficulties | 0 | REF | ||
| 1 | 2.49 (2.05, 3.01) | |||
| 2 | 2.65 (2.06, 3.41) | |||
| 3 | 3.12 (2.29, 4.25) | |||
| 4 | 3.98 (2.90, 5.48) | |||
| 5 | 6.17 (4.29, 8.89) | |||
| Depressive symptoms | Continuous | 1.08 (1.05, 1.12) | ||
| Arthritis | No | REF | ||
| Yes | 0.83 (0.55, 1.26) | |||
| Cancer | No | REF | ||
| Yes | 4.20 (3.26, 5.43) | |||
| Diabetes | No | REF | ||
| Yes | 1.06 (0.72, 1.56) | |||
| Heart disease | No | REF | ||
| Yes | 1.58 (1.19, 2.10) | |||
| Stroke | No | REF | ||
| Yes | 1.36 (0.93, 1.99) | |||
| High blood pressure | No | REF | ||
| Yes | 1.20 (0.89, 1.61) | |||
| Lung disease | No | REF | ||
| Yes | 1.21 (0.83, 1.77) | |||
| Psychiatric problems | No | REF | ||
| Yes | 0.94 (0.61, 1.44) | |||
Hazard ratios derived from a Cox proportional hazard model with the following covariates: time-varying covariates of alcohol consumption category, gender, age at baseline, race, wealth, smoking, BMI, difficulties in activities of daily living, depressive symptoms based on Center for Epidemiologic Studies Depression Scale (CES-D), arthritis since previous wave, cancer since previous wave, diabetes since previous wave, heart disease since previous wave, stroke since previous wave, high blood pressure since previous wave, lung disease since previous wave, and psychiatric problem since previous wave. (Model 1 N=4,285; Model 2 N=4,271; Model 3 N=4,200).
Our estimates were largely consistent across models. Among men (Table 3a), current abstaining remained associated with higher mortality (model 3: HR=1.25, 95% C.I. 1.02–1.53) and moderate drinking with lower mortality (model 3: HR=0.74, 95% C.I. 0.60–0.91) compared with occasional drinking. Among women (Table 3b), both lifetime abstaining (model 3: HR=1.35, 95% C.I. 1.08–1.68) and current abstaining (model 3: HR=1.34, 95% C.I. 1.08–1.67) remained associated with higher mortality.
Finally, we tested interactions between time-varying alcohol consumption and each variable in the model. For these models, sex was included as a covariate except in models where interactions between drinking status and sex were tested. Tests of all interactions are included in Online Table 3. Two interactions suggested substantial heterogeneity: smoking (HR for moderate drinking/current smoker interaction: 1.69 [95% C.I. 1.04–2.75], HR for heavy drinking/current smoker interaction: 0.33 [95% C.I. 0.13–0.86]), and gender (HR for lifetime abstaining drinking/female gender interaction: 1.40 [95% C.I. 1.04–1.90]). Figures 2 and 3 plot the hazard differences for mortality from a model including the interaction term, from a model adjusted for all covariates, for smoking (Figure 2) and gender (Figure 3). Compared to occasional drinkers who reported never smoking, occasional drinkers who currently smoke or smoked in the past have an increased risk of mortality, while moderate drinkers/never smokers have lower risk of mortality. All other groups have a higher mortality rate than occasional drinkers who currently smoke, though some hazard differences were imprecise. By gender, moderately drinking women had the lowest rate of mortality; in comparison, men had increased mortality rates regardless of drinking status, although the confidence interval for heavy drinking men was wide. Compared to occassionally drinking women, lifetime and currently abstaining women had higher mortality rates.
Figure 2.
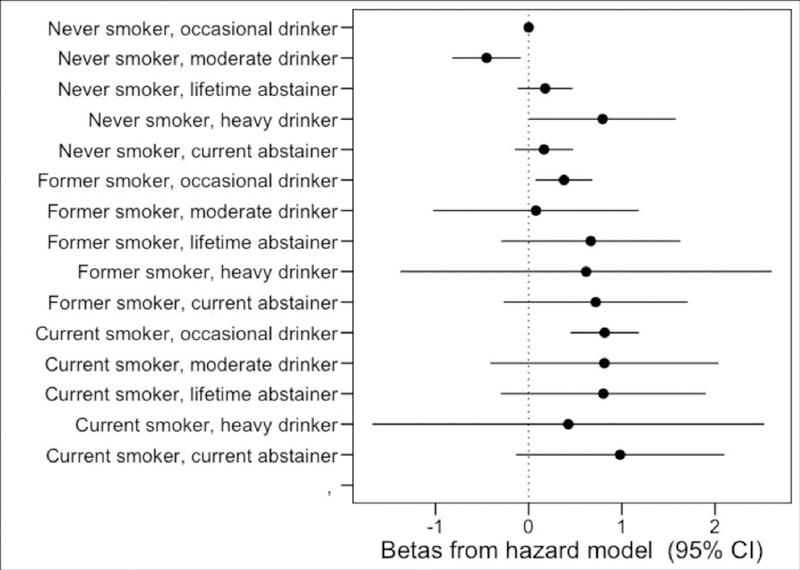
Predicted mortality hazard differences based on the interaction of average drinking status across waves and average smoking status across waves in a longitudinal sample of adults over 56 in the United States (N=7,904). Referent group for each hazard ratio is never smoker/occasional drinkers. Hazard differences derived from a Cox proportional hazard model with and interaction term between alcohol consumption and smoking (P<0.01 for the interaction), an interaction term between alcohol consumption and gender, and the following covariates: gender, age at baseline, race, wealth, smoking, BMI, difficulties in activities of daily living, depressive symptoms based on Center for Epidemiologic Studies Depression Scale (CES-D), arthritis since previous wave, cancer since previous wave, diabetes since previous wave, heart disease since previous wave, stroke since previous wave, high blood pressure since previous wave, lung disease since previous wave, and psychiatric problem since previous wave.
Figure 3.
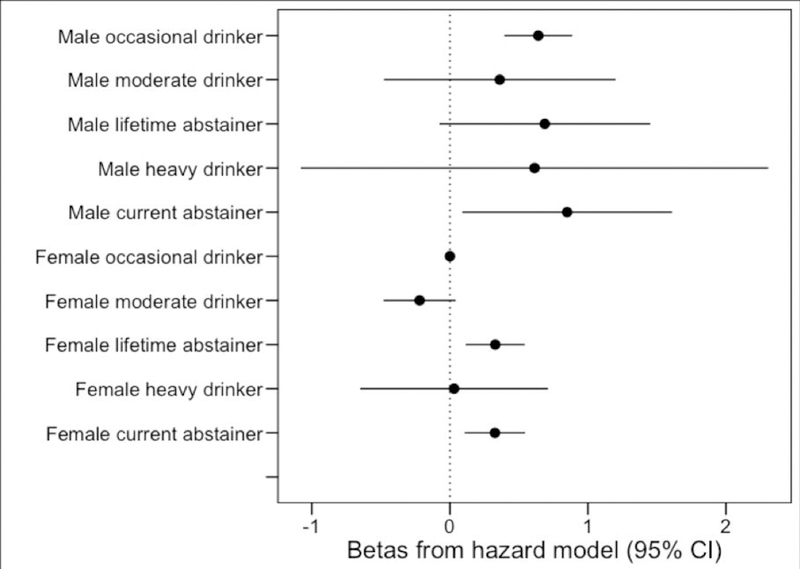
Predicted mortality hazard differences based on the interaction of average drinking status across waves and gender in a longitudinal sample of adults over 56 in the United States (N=7,904). Referent group for each hazard ratio is moderate drinkers/women. Hazard differences derived from a Cox proportional hazard model with and interaction term between alcohol consumption and smoking, an interaction term between alcohol consumption and gender (P<0.01 for the interaction), and the following covariates: gender, age at baseline, race, wealth, smoking, BMI, difficulties in activities of daily living, depressive symptoms based on Center for Epidemiologic Studies Depression Scale (CES-D), arthritis since previous wave, cancer since previous wave, diabetes since previous wave, heart disease since previous wave, stroke since previous wave, high blood pressure since previous wave, lung disease since previous wave, and psychiatric problem since previous wave.
Sensitivity Analysis: Quantitative Bias Analysis
We determined how strong residual, uncontrolled confounding would need to be in order to explain the association between lifetime abstention and mortality, compared with occasional drinking. We assessed the change in the hazard ratio for the association between alcohol abstention and mortality, compared to occasional drinking, based on a range of associations between unmeasured confounding and mortality, as well as differences in the prevalence of unmeasured confounding between occasional consumers and abstainers. Results are shown in Online Table 4. We first assumed that confounders would be twice as prevalent among occasional drinkers compared with abstainers, with a prevalence of 20% among occasional drinkers and 10% among long term abstainers. With this distribution, confounders would need to increase the mortality rate by 4-fold for men and 9-fold for women before more than half of the 1,000 simulations had a hazard ratio above 1.0. If we increase the difference between occasional consumers and abstainers in the distribution of unmeasured confounders, the magnitude of association between unmeasured confounders and mortality needed to nullify observed associations decreases. With a prevalence of 30% among abstainers and 10% among moderate consumers, unmeasured confounders need to increase the mortality rate by 3-fold for men and 4-fold for women before more than half of the 1,000 simulations had hazard ratios above 1.0.
Discussion
The present study used national data from the US on adults >56 years for the first time followed across an ~15 years to examine the association between alcohol consumption and mortality, incorporating the time-varying nature of alcohol consumption and a wide range of well-measured potential confounders. We found that individuals who reported consuming alcohol moderately or occasionally had, on average, lower mortality rates than both recent and lifetime abstainers. This association held while controlling for a wide range of both time-varying and time-invariant confounders, including self-reported chronic health problems and difficulties in daily living activities, mental health, and BMI, as well as multiple indicators of socio-economic status. Further, we found there was variation in the magnitude of these associations by smoking status and gender, with smokers and men evidencing less of a mortality decrease than nonsmokers and women, respectively.
While numerous studies have examined the relationship between alcohol consumption and mortality, methodological limitations have abounded. In a recent meta-analysis (Stockwell et al., 2016), Stockwell and colleagues noted that of 87 studies, at least 65 used a reference group of abstainers that included former drinkers, suggesting the potential for selection bias (Licaj et al., 2016; Ortolá et al., 2018). Similar biases were highlighted in an additional meta-analysis examining alcohol consumption and cardiovascular disease (Zhao et al., 2017). Selection bias and residual confounding across studies of consumption and mortality have routinely been identified (Naimi et al., 2017, 2005). Given that many individuals stop drinking alcohol due to the onset of illness or other health concerns (Dawson et al., 2013; Naimi et al., 2017; Rehm et al., 2016b), former drinkers are a group at much higher mortality risk than lifetime abstainers (Fillmore et al., 2007; Rehm et al., 2008). Indeed, our analyses showed that “current” abstainers, a group who reported drinking at one or more previous waves of data collection but not the focal wave, had the highest mortality rates of all groups (suggesting that this association may be indicative of reverse causation). Further, the association between current abstention and mortality, compared with lifetime abstention, substantially diminished when controlling for multiple morbidities, which would be expected if health problems underlie the decision not to drink alcohol.
We found an inverse association for moderate and occasional drinkers compared with lifetime abstention. The meta-analytic estimate produced by Stockwell et al., when no abstainer biases were present in the analyzed studies, suggested that occasional and low-volume drinkers had 0.94 and 0.90 times the mortality rate compared with lifetime abstainers, whereas our estimates indicated that similar levels of drinking were associated with 0.74 and 0.82 times the mortality rate, among men and women, respectively. Several explanations may underlie these differences. First, as Stockwell et al. note, few studies in the literature adequately addressed abstainer biases (only four studies out of 87, for example, were included in the estimates of occasional drinking), thus additional data points are necessary. Second, our analysis of the HRS has substantially longer follow-up than previous studies from the literature. These results are in line with other reports from HRS showing a protective effect of moderate drinking (Nandi et al., 2014; Shaw and Agahi, 2012), though adding 8–10 years of follow-up data, as well as more comprehensive confounder assessments. Existing literature is largely based on single time points of assessment of alcohol use; in Online Table 5, we analyzed the HRS data with only the baseline assessment of alcohol consumption as a predictor, rather than allowing alcohol use to time vary. Of interest, the results are aligned with the Stockwell et al. meta-analysis, with the effect size for moderate drinking at 0.81 (95% C.I. 0.68–0.96) among men and 0.93 (95% C.I. 0.76, 1.15) among women. Thus, including of time-varying alcohol use increased the effect size of the association between alcohol consumption and mortality.
Yet, while the HRS provides potential improvements over some prior literature, residual confounding and selection biases remain probable, suggesting again that observational data, even high-quality longitudinal data such as HRS, should be interpreted with serious cauation.. Results are inconsistent with larger data sources with single time-points of alcohol consumption compared with later death; for example, a recent large pooled analysis of 599,912 current drinkers from more than 80 prospective studies documented no mortality benefit even at low levels of consumption for all-cause mortality (Wood et al., 2018), though the majority of the study participants were only assessed for alcohol consumption at one time point. Further, Wood et al. 2018 documented a stronger moderate drinking association when former and lifetime abstainers are included in comparisons. A recent meta-analysis of prospective studies found no level of alcohol that was protective against major causes of death (GBD 2016 Alcohol Collaborators, 2018), suggesting that in totality studies lean towards no benefit. And indeed, as demonstrated in Online Table 5, when only using one-time assessments of the HRS data to analyze the association between alcohol consumption and mortality, similar results emerge. Further, these results are not in line with Mendelian randomization studies (Cho et al., 2016; Holmes et al., 2014; Millwood et al., 2019; Taylor et al., 2015) which use instrumental variable approaches to overcome the often intractable confounding in observational designs; however, these approaches have been criticized as well for the stringentness of assumptions necessary for causal inference that are difficult to meet for behaviorally- and socially-driven exposures such as alcohol consumption. As such, continued research using more and better data sources are needed.
While the long timespan of the HRS is indeed a strength, heavy drinkers did not have a higher risk of mortality compared to abstainers, as would be expected from previous longitudinal studies (Rehm et al., 2009; Rehm and Sempos, 1995). Measurement error due to self-report, or continued issues of reverse causation (e.g., binge drinking requires a relatively high level of health at older age to engage in it) should be considered when interpreting these results. Yet other risk factors in the data are associated with mortality in ways that are consistent with previous research. We note that obesity was not associated with mortality in these data; while obesity is associated with higher mortality in general population adult samples (Flegal et al., 2005; Masters et al., 2013), it is widely acknowledged that obesity is inconsistently and narrowly associated with mortality in older age, due in part to selection and reverse causation (e.g., those who are older and with higher levels of chronic disease may have less body mass) (reviewed in (Winter et al., 2014)). In summary, data from HRS are of high quality for observational research in a national context, and yet as any observational data, the potential for selection factors and measurement error remain a concern for validity.
Additionally, we found evidence of effect measure modification by smoking status and gender. Of course, cigarette smoking is a substantial risk factor for cardiovascular disease as well as most other adverse health outcomes (Doll et al., 1994), thus the finding that smokers do not evidence a mortality benefit from moderate drinking perhaps points to the robustness of the present analyses. Results also indicate that men who heavily drink show higher mortality than women. Given that within the heavy drinker category, men have a greater number of total drinks as well as frequency (Keyes et al., 2011), it could be that the ‘dose’ of alcohol is higher for men than women, even within group. Indeed, in the HRS data among the heavy drinking group, men had an average of 7.3 drinks per drinking day and women had 4.2 drinks per drinking day at baseline, and men had higher quantity than women at each subsequent wave. No other covariates significantly modified the relationship between consumption and mortality. This was surprising, especially for covariates such as race, which has been demonstrated in previous studies to modify the relationship (Kerr et al., 2011; Stockwell et al., 2016; Zhao et al., 2017), as well as other risk factors such as BMI and chronic disease, which we would expect to mitigate any mortality benefit from alcohol consumption similar to smoking. In summary, these data suggest that the inverse association between moderate alcohol consumption and mortality is consistent across a number of independent risk factors, but modified by competing risks for mortality such as smoking, as well as alcohol dose.
In addition to potential limitations of the HRS cohort described above, several other limitations should be considered. Alcohol consumption data is self-reported and may have measurement error, but it is the best available information from survey data as cumulative alcohol consumption is difficult to biologically validate. Alcohol consumption was measured every two years, on average; beverage patterns may change across a two-year window which would not be captured by the HRS assessments. However, we note that few prior studies of the relationship between consumption and mortality have included regular, systematic and time-varying assessments of drinking, especially across 15 years of follow-up. Finally, the relationships between alcohol consumption and mortality in older age may be clarified further by not only characterizing alcohol consumption as a dynamic exposure, but explicitly modeling trajectories of alcohol use over time (e.g. using sequence analysis), which is an important future direction.
In summary, the associations indicating potential health benefits of moderate drinking are increasingly viewed with skepticism. The role of moderate drinking in mortality continues to be debated. There are many health conditions for which no safe dose of alcohol has been found (George and Figueredo, 2011; Patra et al., 2010; Samokhvalov et al., 2010; Taylor et al., 2009) and for which even low amounts of drinking appear to increase risk (Bagnardi et al., 2013). Nevertheless, the HRS is among the largest and most well-designed cohorts of older adults anywhere in the world, and within these data, we do find substantial associations between occasional and moderate drinking and lower mortality rates, compared to lifetime abstainers. Further analyses focused on the measurement and reduction of abstainer biases are necessary to accumulate a well-understood body of work in this area.
Supplementary Material
Acknowledgements:
Funding: Funding was contributed by the Robert N. Butler Columbia Aging Center, the National Institute of Health (Keyes: K01AA021511), and Comisión Nacional de Investigación Científica y Tecnológica (Calvo: FONDECYT Regular #1181009).
Footnotes
Conflict of interest: The authors report no conflicts of interest.
Contributor Information
Katherine M. Keyes, Department of Epidemiology, Columbia University, New York, NY; Robert N. Butler Columbia Aging Center, Columbia University, New York, NY; Society and Health Research Center, Facultad de Humanidades Universidad Mayor, Santiago, Chile.
Esteban Calvo, Department of Epidemiology, Columbia University, New York, NY; Robert N. Butler Columbia Aging Center, Columbia University, New York, NY; Society and Health Research Center, Facultad de Humanidades Universidad Mayor, Santiago, Chile.
Katherine A. Ornstein, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine, Mount Sinai, New York, NY
Caroline Rutherford, Department of Epidemiology, Columbia University, New York, NY.
Matthew P. Fox, Departments of Epidemiology and Global Health, Boston University, Boston, MA
Ursula M. Staudinger, Robert N. Butler Columbia Aging Center, Columbia University, New York, NY; Department of Sociomedical Sciences, Columbia University, New York, NY
Linda P. Fried, Department of Epidemiology, Columbia University, New York, NY; Robert N. Butler Columbia Aging Center, Columbia University, New York, NY
References
- Andresen EM, Malmgren JA, Carter WB, Patrick DL (1994) Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med [PubMed]
- Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C (2013) Light alcohol drinking and cancer: A meta-analysis. Ann Oncol [DOI] [PubMed]
- Blomster JI, Zoungas S, Chalmers J, Li Q, Chow CK, Woodward M, Mancia G, Poulter N, Williams B, Harrap S, Neal B, Patel A, Hillis GS (2014) The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes. Diabetes Care 37:1353–1359. [DOI] [PubMed] [Google Scholar]
- Breslow RA, Castle IJP, Chen CM, Graubard BI (2017) Trends in Alcohol Consumption Among Older Americans: National Health Interview Surveys, 1997 to 2014. Alcohol Clin Exp Res 41:976–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA (2011) Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 342:d636–d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (2018) CPI Inflation Calculator Available https://www.bls.gov/data/inflation_calculator.htm Accessed March 1, 2018.
- Cerdá M, Johnson-Lawrence VD, Galea S (2011) Lifetime income patterns and alcohol consumption: Investigating the association between long- and short-term income trajectories and drinking. Soc Sci Med 73:1178–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho Y, Shin S-Y, Won S, Relton CL, Davey Smith G, Shin M-J (2016) Alcohol intake and cardiovascular risk factors: A Mendelian randomisation study. Sci Rep 5:18422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J (2006) The life and times of the J-shaped curve. Alcohol Alcohol 41:583–584. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF (2013) Prospective correlates of drinking cessation: Variation across the life-course. Addiction 108:712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, De Gaetano G (2006) Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch Intern Med [DOI] [PubMed]
- Doll R, Peto R, Wheatley K, Gray R, Sutherland I (1994) Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ 309:901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W (2007) Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol 17:S16–23. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH, J B, HW M, BV S, DL M, KM F, AA H, KM F, KM F, DB A, JR B, AH M, B R, SR S, MH G, A E, A M, BB C, CS C, CM L, EL K, AM M, EL K, EW G, SR M, RS C, AR D, WC W, KR F, RP T, UA A, PT K, HE M, SW F, N H-N, WJ S, A H, TL V, JM D (2005) Excess Deaths Associated With Underweight, Overweight, and Obesity. JAMA [DOI] [PubMed]
- French MT, Popovici I, Maclean JC (2009) Do alcohol consumers exercise more? findings from a national survey. Am J Heal Promot [DOI] [PMC free article] [PubMed]
- Fuchs FD, Chambless LE, Folsom AR, Eigenbrodt ML, Duncan BB, Gilbert A, Szklo M (2004) Association between alcoholic beverage consumption and incidence of coronary heart disease in whites and blacks: the Atherosclerosis Risk in Communities Study. Am J Epidemiol 160:466–474. [DOI] [PubMed] [Google Scholar]
- GBD 2016 Alcohol Collaborators (2018) Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392:1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Figueredo VM (2011) Alcoholic cardiomyopathy: A review. J Card Fail [DOI] [PubMed]
- Gepner Y, Golan R, Harman-Boehm I, Henkin Y, Schwarzfuchs D, Shelef I, Durst R, Kovsan J, Bolotin A, Leitersdorf E, Shpitzen S, Balag S, Shemesh E, Witkow S, Tangi-Rosental O, Chassidim Y, Liberty IF, Sarusi B, Ben-Avraham S, Helander A, Ceglarek U, Stumvoll M, Blüher M, Thiery J, Rudich A, Stampfer MJ, Shai I (2015) Effects of initiating moderate alcohol intake on cardiometabolic risk in adults with type 2 diabetes: A 2-year randomized, controlled trial. Ann Intern Med 163:569–579. [DOI] [PubMed] [Google Scholar]
- Goulden R (2016) Moderate Alcohol Consumption Is Not Associated with Reduced All-cause Mortality. Am J Med 129:180–186.e4. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Kerr WC (2014) Physicians’ prescription for lifetime abstainers aged 40 to 50 to take a drink a day is not yet justified. Alcohol Clin Exp Res 38:2893–2895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Lash TL (2008) Bias analysis. Mod Epidemiol 345–380.
- Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, Hartz S, Virdi G, Bierut LJ (2018) Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol Clin Exp Res [DOI] [PMC free article] [PubMed]
- Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, Prieto-Merino D, Dehghan A, Trompet S, Wong A, Cavadino A, Drogan D, Padmanabhan S, Li S, Yesupriya A, Leusink M, Sundstrom J, Hubacek JA, Pikhart H, Swerdlow DI, Panayiotou AG, Borinskaya SA, Finan C, Shah S, Kuchenbaecker KB, Shah T, Engmann J, Folkersen L, Eriksson P, Ricceri F, Melander O, Sacerdote C, Gamble DM, Rayaprolu S, Ross OA, McLachlan S, Vikhireva O, Sluijs I, Scott RA, Adamkova V, Flicker L, Bockxmeer FM v., Power C, Marques-Vidal P, Meade T, Marmot MG, Ferro JM, Paulos-Pinheiro S, Humphries SE, Talmud PJ, Leach IM, Verweij N, Linneberg A, Skaaby T, Doevendans PA, Cramer MJ, Harst P v., Klungel OH, Dowling NF, Dominiczak AF, Kumari M, Nicolaides AN, Weikert C, Boeing H, Ebrahim S, Gaunt TR, Price JF, Lannfelt L, Peasey A, Kubinova R, Pajak A, Malyutina S, Voevoda MI, Tamosiunas A, Maitland-van der Zee AH, Norman PE, Hankey GJ, Bergmann MM, Hofman A, Franco OH, Cooper J, Palmen J, Spiering W, Jong PA d., Kuh D, Hardy R, Uitterlinden AG, Ikram MA, Ford I, Hypponen E, Almeida OP, Wareham NJ, Khaw K-T, Hamsten A, Husemoen LLN, Tjonneland A, Tolstrup JS, Rimm E, Beulens JWJ, Verschuren WMM, Onland-Moret NC, Hofker MH, Wannamethee SG, Whincup PH, Morris R, Vicente AM, Watkins H, Farrall M, Jukema JW, Meschia J, Cupples LA, Sharp SJ, Fornage M, Kooperberg C, LaCroix AZ, Dai JY, Lanktree MB, Siscovick DS, Jorgenson E, Spring B, Coresh J, Li YR, Buxbaum SG, Schreiner PJ, Ellison RC, Tsai MY, Patel SR, Redline S, Johnson AD, Hoogeveen RC, Hakonarson H, Rotter JI, Boerwinkle E, Bakker PIW d., Kivimaki M, Asselbergs FW, Sattar N, Lawlor DA, Whittaker J, Davey Smith G, Mukamal K, Psaty BM, Wilson JG, Lange LA, Hamidovic A, Hingorani AD, Nordestgaard BG, Bobak M, Leon DA, Langenberg C, Palmer TM, Reiner AP, Keating BJ, Dudbridge F, Casas JP (2014) Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 349:g4164–g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J (2011) Racial and ethnic differences in all-cause mortality risk according to alcohol consumption patterns in the national alcohol surveys. Am J Epidemiol [DOI] [PMC free article] [PubMed]
- Keyes KM, Li G, Hasin DS (2011) Birth Cohort Effects and Gender Differences in Alcohol Epidemiology: A Review and Synthesis. Alcohol Clin Exp Res [DOI] [PMC free article] [PubMed]
- Keyes KM, Miech R (2013) Commentary on Dawson et al. (2013): Drink to your health? Maybe not. Addiction [DOI] [PMC free article] [PubMed]
- Lang I, Wallace RB, Huppert FA, Melzer D (2007) Moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence. Age Ageing 36:256–261. [DOI] [PubMed] [Google Scholar]
- Lash TL, Fox MP, Fink AK (2009) Applying Quantitative Bias Analysis to Epidemiologic Data, Statistics for Biology and Health New York, NY, Springer New York. [Google Scholar]
- Lash TL, Fox MP, Maclehose RF, Maldonado G, Mccandless LC, Greenland S (2014) Good practices for quantitative bias analysis. Int J Epidemiol 43:1969–1985. [DOI] [PubMed] [Google Scholar]
- Leong DP, Smyth A, Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Anand SS, Yusuf S (2014) Patterns of alcohol consumption and myocardial infarction risk: Observations from 52 countries in the INTERHEART case-control study. Circulation 130:390–398. [DOI] [PubMed] [Google Scholar]
- Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK, Ontarget, Investigators T (2012) Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 184:E857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licaj I, Sandin S, Skeie G, Adami HO, Roswall N, Weiderpass E (2016) Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open [DOI] [PMC free article] [PubMed]
- Masters RK, Reither EN, Powers DA, Yang YC, Burger AE, Link BG (2013) The impact of obesity on US mortality levels: The importance of age and cohort factors in population estimates. Am J Public Health [DOI] [PMC free article] [PubMed]
- Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, Bennett DA, Chen Y, Dong C, Hu R, Zhou G, Yu B, Jia W, Parish S, Clarke R, Davey Smith G, Collins R, Holmes MV, Li L, Peto R, Chen Z (2019) Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500,000 men and women in China. Lancet 393:1831–1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Brown DW, Brewer RD, Giles WH, Mensah G, Serdula MK, Mokdad AH, Hungerford DW, Lando J, Naimi S, Stroup DF (2005) Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med 28:369–373. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Stockwell T, Zhao J, Xuan Z, Dangardt F, Saitz R, Liang W, Chikritzhs T (2017) Selection biases in observational studies affect associations between ‘moderate’ alcohol consumption and mortality. Addiction 112:207–214. [DOI] [PubMed] [Google Scholar]
- Nandi A, Glymour MM, Subramanian SV. (2014) Association among socioeconomic status, health behaviors, and all-cause mortality in the United States. Epidemiology [DOI] [PubMed]
- Nurmi K, Virkanen J, Rajamäki K, Niemi K, Kovanen PT, Eklund KK (2013) Ethanol inhibits activation of NLRP3 and AIM2 inflammasomes in human macrophages - A novel anti-inflammatory action of alcohol. PLoS One 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortolá R, García-Esquinas E, López-García E, León-Muñoz LM, Banegas JR, Rodríguez-Artalejo F (2018) Alcohol consumption and all-cause mortality in older adults in Spain: an analysis accounting for the main methodological issues. Addiction [DOI] [PubMed]
- Patra J, Taylor B, Irving H, Roerecke M, Baliunas D, Mohapatra S, Rehm J (2010) Alcohol consumption and the risk of morbidity and mortality for different stroke types - a systematic review and meta-analysis. BMC Public Health 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L (1977) The CES-D scale: A self report depression scale for research in the general population. Appl Psychol Meas 1:385–401. [Google Scholar]
- Rehm J (2019) Why the relationship between level of alcohol-use and all-cause mortality cannot be addressed with meta-analyses of cohort studies. Drug Alcohol Rev 38:3–4. [DOI] [PubMed] [Google Scholar]
- Rehm J, Greenfield TK, Kerr W (2006) Patterns of drinking and mortality from different diseases-an overview. Contemp Drug Probl 33:205–235. [Google Scholar]
- Rehm J, Irving H, Ye YY, Kerr WC, Bond J, Greenfield TK (2008) Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am J Epidemiol 168:866–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet [DOI] [PubMed]
- Rehm J, Roerecke M, Room R (2016a) All-cause mortality risks for “moderate drinkers”: What are the implications for burden-of-disease studies and low risk–drinking guidelines? J Stud Alcohol Drugs 77:203–204. [DOI] [PubMed] [Google Scholar]
- Rehm J, Sempos CT (1995) Alcohol consumption and all‐cause mortality. Addiction 90:471–480. [DOI] [PubMed] [Google Scholar]
- Rehm J, Shield KD, Roerecke M, Gmel G (2016b) Modelling the impact of alcohol consumption on cardiovascular disease mortality for comparative risk assessments: An overview. BMC Public Health 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rist PM, Berger K, Buring JE, Kase CS, Gaziano JM, Kurth T (2010) Alcohol consumption and functional outcome after stroke in men. Stroke [DOI] [PMC free article] [PubMed]
- Samokhvalov AV, Irving HM, Rehm J (2010) Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 17:706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sempos CT, Rehm J, Wu T, Crespo CJ, Trevisan M (2003) Average volume of alcohol consumption and all-cause mortality in African Americans: the NHEFS cohort. Alcohol Clin Exp Res 27:88–92. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Agahi N (2012) A prospective cohort study of health behavior profiles after age 50 and mortality risk. BMC Public Health [DOI] [PMC free article] [PubMed]
- Skog O‐J (1985) The Collectivity of Drinking Cultures: A Theory of the Distribution of Alcohol Consumption. Br J Addict 80:83–99. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T (2016) Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 77:185–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AE, Lu F, Carslake D, Hu Z, Qian Y, Liu S, Chen J, Shen H, Smith GD (2015) Exploring causal associations of alcohol with cardiovascular and metabolic risk factors in a Chinese population using Mendelian randomization analysis. Sci Rep 5:14005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor B, Irving HM, Baliunas D, Roerecke M, Patra J, Mohapatra S, Rehm J (2009) Alcohol and hypertension: Gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction [DOI] [PubMed]
- Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, Doll R (1997) Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med 337:1705–14. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG (1998) Alcohol, coronary heart disease and stroke: an examination of the J-shaped curve. Neuroepidemiology 17:288–295. [DOI] [PubMed] [Google Scholar]
- Weir D (2016) Validating mortality ascertainment in the Health and Retirement Study Available https://hrs.isr.umich.edu/sites/default/files/biblio/Weir_mortality_ascertainment.pdf Accessed March 1, 2018.
- Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA (2014) BMI and all-cause mortality in older adults: A meta-analysis. Am J Clin Nutr [DOI] [PubMed]
- Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S, Astle W, Stevens D, Koulman A, Selmer RM, Verschuren WMM, Sato S, Njølstad I, Woodward M, Salomaa V, Nordestgaard BG, Yeap BB, Fletcher A, Melander O, Kuller LH, Balkau B, Marmot M, Koenig W, Casiglia E, Cooper C, Arndt V, Franco OH, Wennberg P, Gallacher J, de la Cámara AG, Völzke H, Dahm CC, Dale CE, Bergmann MM, Crespo CJ, van der Schouw YT, Kaaks R, Simons LA, Lagiou P, Schoufour JD, Boer JMA, Key TJ, Rodriguez B, Moreno-Iribas C, Davidson KW, Taylor JO, Sacerdote C, Wallace RB, Quiros JR, Tumino R, Blazer DG, Linneberg A, Daimon M, Panico S, Howard B, Skeie G, Strandberg T, Weiderpass E, Nietert PJ, Psaty BM, Kromhout D, Salamanca-Fernandez E, Kiechl S, Krumholz HM, Grioni S, Palli D, Huerta JM, Price J, Sundström J, Arriola L, Arima H, Travis RC, Panagiotakos DB, Karakatsani A, Trichopoulou A, Kühn T, Grobbee DE, Barrett-Connor E, van Schoor N, Boeing H, Overvad K, Kauhanen J, Wareham N, Langenberg C, Forouhi N, Wennberg M, Després J-P, Cushman M, Cooper JA, Rodriguez CJ, Sakurai M, Shaw JE, Knuiman M, Voortman T, Meisinger C, Tjønneland A, Brenner H, Palmieri L, Dallongeville J, Brunner EJ, Assmann G, Trevisan M, Gillum RF, Ford I, Sattar N, Lazo M, Thompson SG, Ferrari P, Leon DA, Smith GD, Peto R, Jackson R, Banks E, Di Angelantonio E, Danesh J, Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group AM, Kaptoge S, Butterworth A, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S, Astle W, Stevens D, Koulman A, Selmer RM, Verschuren M, Sato S, Njølstad I, Woodward M, Veikko S, Nordestgaard BG, Yeap BB, Flecther A, Melander O, Kuller LH, Balkau B, Marmot M, Koenig W, Casiglia E, Cooper C, Arndt V, Franco OH, Wennberg P, Gallacher J, Cámara AG de la, Völzke H, Dahm CC, Dale CE, Bergmann M, Crespo C, Schouw YT van der, Kaaks R, Simons LA, Lagiou P, Schoufour JD, Boer JM, Key TJ, Rodriguez B, Moreno-Iribas C, Davidson KW, Taylor JO, Sacerdote C, Wallace RB, Quiros JR, Rimm EB, Tumino R, III DGB, Linneberg A, Daimon M, Panico S, Howard B, Skeie G, Salomaa V, Strandberg T, Weiderpass E, Nietert PJ, Psaty BM, Kromhout D, Salamanca-Fernandez E, Kiechl S, Krumholz HM, Grioni S, Palli D, Huerta JM, Price J, Sundström J, Arriola L, Arima H, Travis RC, Panagiotakos DB, Karakatsani A, Trichopoulou A, Kühn T, Grobbee DE, Barrett-Connor E, Schoor N van, Boeing H, Overvad K, Kauhanen J, Wareham N, Langenberg C, Forouhi N, Wennberg M, Després J-P, Cushman M, Cooper JA, Rodriguez CJ, Sakurai M, Shaw JE, Knuiman M, Voortman T, Meisinger C, Tjønneland A, Brenner H, Palmieri L, Dallongeville J-P, Brunner EJ, Assmann G, Trevisan M, Gillumn RF, Ford IF, Sattar N, Lazo M, Thompson S, Ferrari P, Leon DA, Smith GD, Peto R, Jackson R, Banks E, Angelantonio E Di, Danesh J (2018) Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet (London, England) 391:1513–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T (2017) Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies. J Stud Alcohol Drugs 78:375–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


