Abstract
Purpose
Patients with high-grade osteosarcoma undergo several chemotherapy cycles before surgical intervention. Response to chemotherapy, however, is affected by intratumor heterogeneity. In this study, we assessed the ability of a machine learning approach using baseline 18F-fluorodeoxyglucose (18F-FDG) positron emitted tomography (PET) textural features to predict response to chemotherapy in osteosarcoma patients.
Materials and Methods
This study included 70 osteosarcoma patients who received neoadjuvant chemotherapy. Quantitative characteristics of the tumors were evaluated by standard uptake value (SUV), total lesion glycolysis (TLG), and metabolic tumor volume (MTV). Tumor heterogeneity was evaluated using textural analysis of 18F-FDG PET scan images. Assessments were performed at baseline and after chemotherapy using 18F-FDG PET; 18F-FDG textural features were evaluated using the Chang-Gung Image Texture Analysis toolbox. To predict the chemotherapy response, several features were chosen using the principal component analysis (PCA) feature selection method. Machine learning was performed using linear support vector machine (SVM), random forest, and gradient boost methods. The ability to predict chemotherapy response was evaluated using the area under the receiver operating characteristic curve (AUC).
Results
AUCs of the baseline 18F-FDG features SUVmax, TLG, MTV, 1st entropy, and gray level co-occurrence matrix entropy were 0.553, 0538, 0.536, 0.538, and 0.543, respectively. However, AUCs of the machine learning features linear SVM, random forest, and gradient boost were 0.72, 0.78, and 0.82, respectively.
Conclusion
We found that a machine learning approach based on 18F-FDG textural features could predict the chemotherapy response using baseline PET images. This early prediction of the chemotherapy response may aid in determining treatment plans for osteosarcoma patients.
1. Introduction
Osteosarcoma is a malignant tumor that primarily develops in bones of patients between 5 and 25 years of age. Osteosarcoma is a type of mesenchymal tumor that frequently metastasizes to the lungs and peripheral bone. Therefore, metastatic potential is a key factor in determining the diagnosis and prognosis of osteosarcoma [1, 2]. The introduction of neoadjuvant chemotherapy (NAC) in the treatment of osteosarcoma has led to improved prognosis and enhanced patient survival. Patient prognosis after combined NAC and surgery is better than after either treatment as monotherapy [3, 4]. In general, patients with high-grade osteosarcoma have numerous cycles of NAC before surgery. However, ineffective NAC can be toxic and may increase resistance to anticancer drugs [5]. Histological assessment of response to NAC can only be performed using resected specimens; therefore, response cannot be monitored during the course of NAC.
18F-fluorodeoxyglucose (18F-FDG) positron emitted tomography (PET) scanning is used as a tool to predict prognosis and select cancer treatment, as it allows the response to be measured before anatomical changes occur during treatment [6]. Maximum standardized uptake value (SUVmax), total lesion glycolysis (TLG), and metabolic tumor volume (MTV) are analyzed by 18F-FDG PET scanning; these factors are typical indicators used to predict prognosis and survival in cancer patients [7]. 18F-FDG uptake provides quantitative information regarding metabolism and heterogeneity of the tumors [8, 9].
Characteristics of tumors include abnormal cell growth, metabolism, immunity, and metastasis due to genetic heterogeneity, which enables cells to exhibit different properties in tumor microenvironments [10]. Intratumor heterogeneity has been associated with decreased long-term survival and has been used in assessment of prognosis. Heterogeneity in medical imaging can be evaluated using quantitative analyses of global, local, and regional areas. The textural features of global areas are calculated based on the distributions of each pixel: these include the maximum, mean, and standard deviation of the SUV, as well as the skewness, kurtosis, and 1st entropy, based on histograms. Analysis of textural features in local areas is considered to reflect differences in gray levels among pixels in those areas, such as the gray level co-occurrence matrix (GLCM) [11].
In recent years, studies have been performed using textural features for evaluation of intratumor heterogeneity, as well as prediction of survival rates in pancreatic carcinoma [12], lung cancer [13], and breast cancer [14]. Notably, several researchers have reported that SUVmax, TLG, and MTV are not significantly associated with response to NAC. Similarly, the correlations between textural features and MTV are irrelevant due to increased tumor volume [15]. Quantitative analysis has advantages in the analysis of tumors of various locations and sizes; thus, it is useful for evaluation of irregular and unstructured images [16]. Studies regarding textural features have demonstrated an association between cellular proliferation, necrosis, glucose metabolism, and intratumor heterogeneity [17]. Tumor heterogeneity, proliferation, metabolism, and angiogenesis reportedly can be predicted with quantitative analysis [18].
In this study, we acquired 18F-FDG PET images of patients with high-grade osteosarcoma before and after NAC. We then assessed 18F-FDG textural features and used machine learning to predict responses to NAC.
2. Materials and Methods
2.1. Patients
This retrospective study was conducted in a cohort of 70 patients who were diagnosed with osteosarcoma based on 18F-FDG PET/CT scans during the period from June 2006 to May 2017. All patients had newly diagnosed histologically proven high-grade primary osteosarcoma and received NAC with a combination of methotrexate, adriamycin, and cisplatin. Clinical characteristics, including age, were obtained from medical records and the institutional tumor registry. An experienced pathologist evaluated histological responses to NAC in the resected primary tumor, using specimens obtained during surgical treatment, based on tumor necrosis (<90%, nonresponders; ≥90%, responders) [19]. Seventy osteosarcoma patients underwent binary classification based on tumor necrosis results: thirty-seven were responders (53%) and thirty-three were nonresponders (47%). This study was approved by the Institutional Review Board and performed in accordance with the ethical guidelines of our institutional clinical research committee.
2.2. PET/CT Imaging
PET/CT images were acquired at baseline, as well as after the first and second cycles of NAC, using a PET/CT scanner (Biograph 6 PET/CT scanner, Siemens, Malvern, PA, USA). CT imaging was performed using a 6-slice helical CT scanner with 30 mAs at 130 kVp. After the CT scan, PET scanning was performed from the base of the skull to the thigh using 3.5 min per frame in three-dimensional (3D) mode, 60 min after intravenous injection of 18F-FDG (7.4 MBq/kg). PET images were reconstructed using CT for attenuation correction (field of view, 680 × 680 mm2; voxel size, 4 × 4 × 3 mm3) and 3D ordered subsets expectation maximization algorithms.
2.3. Quantitative Analysis
Textural features were extracted from the 18F-FDG PET images at baseline and after NAC (Table 1). Intratumor heterogeneity was evaluated using quantitative analysis in global, local, and regional areas. Outlines of the 3D region of interest (ROI) were identified in 18F-FDG PET images using the region-growing algorithm. The tumor ROI was confirmed by an experienced nuclear medicine physician. Sampling for the ROI was divided into 64 gray levels, which were verified in previous studies [15]. Quantitative analysis was assessed using the Chang-Gung Image Texture Analysis toolbox (http://code.google.com/p/cgita), an open-source software package implemented in MATLAB (ver. 2012a; MathWorks Inc., Natick, MA, USA) [20]. All calculations regarding the quantitative features workflow were performed in accordance with the Image Biomarker Standardization Initiative (IBIS), and we confirm that the features comply with this guideline [21].
Table 1.
Index of textural features in global, local, and regional areas.
| Feature family | Features |
|---|---|
| Intensity histogram | SUVmax |
| SUVmean | |
| Standard deviation | |
| Total lesion glycolysis (TLG) | |
| Metabolic tumor volume (MTV) | |
| 1st entropy | |
|
| |
| Gray level co-occurrence matrix (GLCM) | Energy |
| Contrast | |
| Entropy | |
| Homogeneity | |
| Dissimilarity | |
|
| |
| Neighboring gray level dependence matrix (NGLDM) | Small number emphasis |
| Large number emphasis | |
| Coarseness | |
| Busyness | |
|
| |
| Gray level run length matrix (GLRLM) | Short run emphasis |
| Long run emphasis | |
| Gray level nonuniformity | |
| Run length nonuniformity | |
| Low gray level run emphasis | |
| High gray level run emphasis | |
|
| |
| Gray level size zone matrix (GLSZM) | Small zone emphasis |
| Large zone emphasis | |
| Gray level nonuniformity | |
| Zone size nonuniformity | |
| Low gray level zone emphasis | |
| High gray level zone emphasis | |
2.4. Machine Learning Approach
Machine learning and principal component analysis (PCA) were performed using the scikit-learn package. Machine learning algorithms in this study included linear support vector machine (SVM), random forest, and gradient boosting. All machine learning approaches were trained using 80% of the osteosarcoma patients' calculated textural features; the remaining 20% of the patients' textural features were used for the test dataset. We used k-fold cross-validation (k = 10) to overcome insufficient data and resolve overfitting of the data.
Linear SVM used the L2 penalty, which is standard in support vector classification. Random forest used 100 estimators and a select entropy criterion. The gradient boosting method used 100 estimators and a Friedman MSE criterion. We also performed the PCA method with machine learning. In this study, we applied the kernel PCA method, using the RBF kernel with 44 components.
Machine learning was performed with or without PCA to compare the receiver operating characteristic (ROC) area under the curve (AUC) for prediction of the response to NAC using baseline 18F-FDG textural features.
2.5. Statistical Analysis
Significant factors in evaluation of the response to NAC were assessed using the Mann–Whitney U test, ROC analysis, and logistic analysis. The capacities of the features for classifying responses to NAC were investigated using the Mann–Whitney U test. The AUC and sensitivity of response to NAC were evaluated using ROC curve analysis. The predicted accuracies of machine learning approaches with and without PCA were assessed using independent t-tests. Differences with p-values < 0.05 were considered statistically significant. All statistical analyses were performed using MedCalc software (version 18.6, MedCalc Software bvba, Ostend, Belgium).
3. Results
3.1. 18F-FDG PET Image of Osteosarcoma Patients
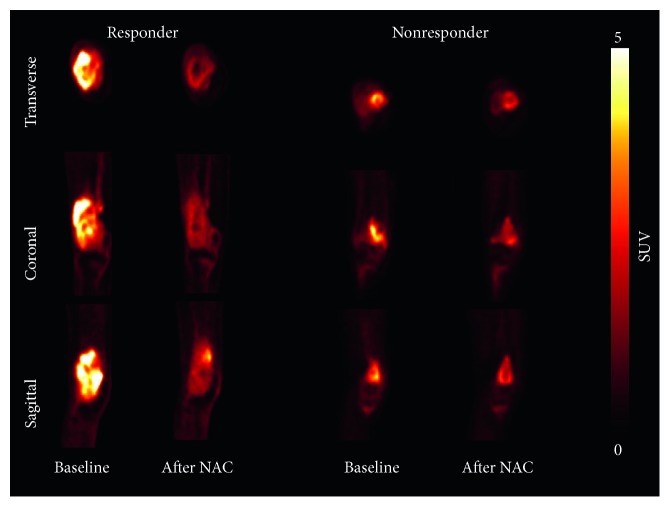
PET images in Figure 1 represent patients classified as responders or nonresponders, based on histological findings. Figure 1 depicts a responder: a 15-year-old male patient with osteosarcoma of the right femur; the SUVmax values at baseline and after NAC were 11.33 and 4.43. Figure 1 also depicts a nonresponder: an 11-year-old female patient with osteosarcoma; the SUVmax values at baseline and after NAC were 5.62 and 3.21.
Figure 1.
Representative 18F-FDG PET images of a responder and a nonresponder with osteosarcoma. Responder SUVmax values were 11.33 and 4.43 at baseline and after neoadjuvant chemotherapy (NAC), respectively. Nonresponders had SUVmax values of 5.62 and 3.21 at baseline and after NAC, respectively.
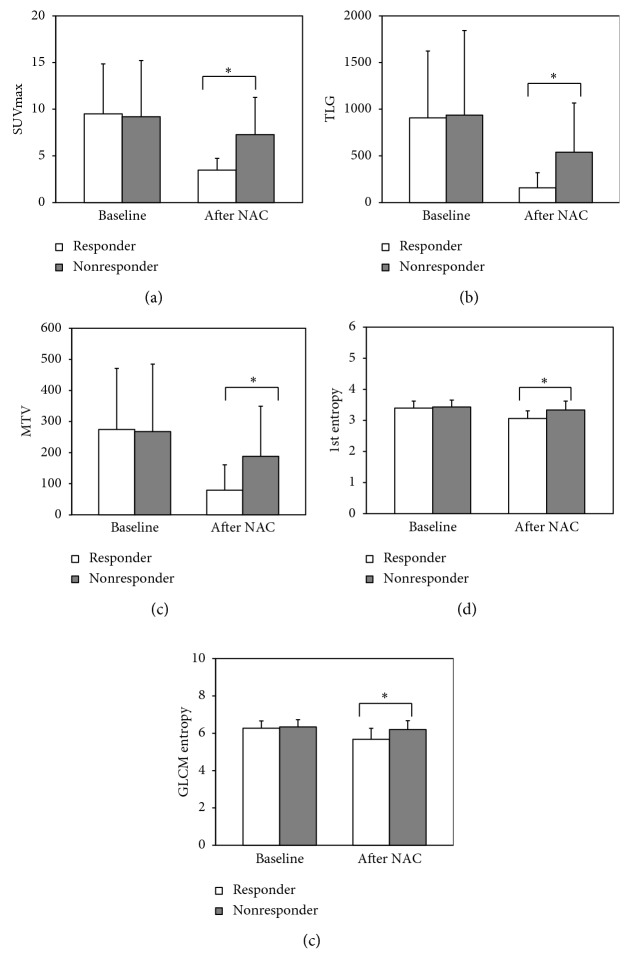
3.2. Comparison of NAC Responder and Nonresponders
The Mann–Whitney U test was used to compare each of the PET quantitative factors between responders and nonresponders at each time point (Figure 2). SUVmax decreased by 53.3% in responders, whereas it decreased by 14.5% in nonresponders. In addition, TLG and MTV both decreased in responders and nonresponders (73.6% and 25.5%, respectively; 65.1% and 22.5%, respectively). Statistical analysis of baseline values showed that SUVmax (p=0.485), TLG (p=0.616), and MTV (p=0.638) did not significantly differ between responders and nonresponders. In addition, 1st entropy change decreased by 9.4% in responders and by 2.6% in nonresponders; GLCM entropy decreased by 9.1% in responders and by 2.0% in nonresponders. These differences were not statistically significant (p=0.616 and p=0.574, respectively, between responders and nonresponders). However, after NAC, all features significantly differed between responder and nonresponder groups.
Figure 2.
Comparison of SUVmax, TLG, MTV, 1st entropy, and GLCM entropy features value for responders and nonresponders at baseline and after neoadjuvant chemotherapy (NAC).
3.3. Prediction of Response to NAC Using Textural Features AUC
ROC analysis showed that baseline 18F-FDG PET textural features had lower AUC (SUVmax: 0.553, TLG: 0.538, MTV: 0.536, 1st entropy: 0.538, and GLCM entropy: 0.543). ROC analyses of the percent changes in textural features showed that AUCs of SUVmax, TLG, MTV, 1st entropy, and GLCM entropy were 0.863, 0.816, 0.764, 0.767, and 0.775, respectively. Notably, the AUCs of percent changes between baseline and after NAC were significantly higher than the AUCs of textural features at baseline and after NAC (Table 2). Figure 3 shows that the ROC after NAC and all features can predict the chemotherapy response.
Table 2.
Receiver operating characteristic curve analysis and univariate logistic regression analysis for evaluation of response to chemotherapy.
| Variable | AUC | Sen (%) | Spe (%) | P-value |
|---|---|---|---|---|
| SUVmax | ||||
| Baseline | 0.553 | 51.61 | 67.86 | 0.488 |
| After NAC | 0.839 | 61.29 | 92.86 | <0.001∗ |
| % change | 0.863 | 93.55 | 71.43 | <0.001∗ |
|
| ||||
| TLG | ||||
| Baseline | 0.538 | 45.16 | 82.14 | 0.626 |
| After NAC | 0.816 | 77.42 | 71.43 | <0.001∗ |
| % change | 0.838 | 80.65 | 82.14 | <0.001∗ |
|
| ||||
| MTV | ||||
| Baseline | 0.536 | 45.16 | 78.57 | 0.645 |
| After NAC | 0.764 | 96.77 | 46.43 | <0.001∗ |
| % change | 0.838 | 80.65 | 82.14 | <0.001∗ |
|
| ||||
| 1st entropy | ||||
| Baseline | 0.538 | 22.58 | 92.86 | 0.616 |
| After NAC | 0.767 | 70.97 | 82.14 | <0.001∗ |
| % change | 0.713 | 70.97 | 71.43 | 0.0018∗ |
|
| ||||
| GLCM entropy | ||||
| Baseline | 0.543 | 41.94 | 75 | 0.575 |
| After NAC | 0.775 | 70.97 | 82.14 | <0.001∗ |
| % change | 0.71 | 67.74 | 75 | 0.0022∗ |
AUC, area under the curve; Sen, sensitivity; Spe, specificity; SUV, standardized uptake value; NAC, neoadjuvant chemotherapy; TLG, total lesion glycolysis; MTV, metabolic tumor volume.
Figure 3.
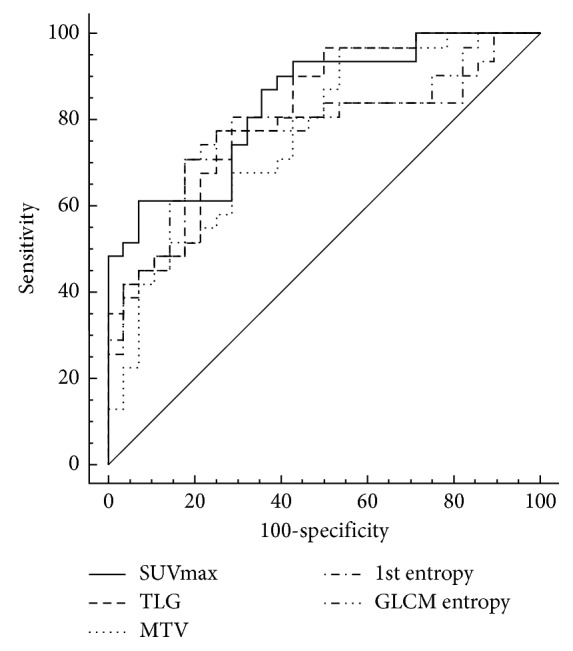
Receiver operating characteristic curves for SUVmax, TLG, MTV, 1st entropy, and GLCM entropy after neoadjuvant chemotherapy (NAC).
ROC analysis of sensitivity and specificity indicated the acceptability of the predictive model. SUVmax showed the highest sensitivity (51.61%) and 1st entropy showed the highest specificity (92.86%) in baseline 18F-FDG PET.
3.4. Prediction of Response to NAC Using Machine Learning with PCA
ROC analysis of machine learning methods without PCA showed that AUCs of linear SVM, random forest, and gradient boost were 0.54 ± 0.05, 0.58 ± 0.17, and 0.59 ± 0.12, respectively; AUCs of these methods with PCA were 0.72 ± 0.22, 0.78 ± 0.24, and 0.82 ± 0.12, respectively. The findings indicated that machine learning with PCA was superior for prediction of the response to NAC using baseline 18F-FDG PET data (Table 3).
Table 3.
Predicted mean accuracies of 10-fold validation for each machine learning approach.
| Machine learning approach | Without PCA | With PCA | P-value |
|---|---|---|---|
| Linear SVM | 0.47 ± 0.16 | 0.72 ± 0.22 | 0.0408∗ |
| Random forest | 0.62 ± 0.21 | 0.78 ± 0.24 | 0.0510 |
| Gradient boost | 0.55 ± 0.19 | 0.82 ± 0.12 | 0.0008∗ |
4. Discussion
In this study, we performed quantitative analysis using 18F-FDG PET images of patients with high-grade osteosarcoma who underwent NAC. We used conventional factors (e.g., SUVmax, MTV, and TLG) and new quantitative factors, 1st entropy and GLCM entropy.
With the increased need for prediction of the effect of NAC cancer treatment and the corresponding survival rate, prognostic factors such as imaging histograms or textural features have gained considerable interest. In particular, textural analysis of tumor heterogeneity using local and regional characteristics has been used to predict survival in patients with pancreatic [12], lung [13], and breast cancer [14]. In a study of osteosarcoma patients, Byun et al. reported prediction of the response to NAC using global textural analysis, especially SUVmax, based on changes in PET images over 1–2.5 hours. Evaluation of the response to NAC using textural analysis has been reported in patients with esophageal cancer [18] and non-small-cell lung cancer [13]. In esophageal cancer patients, response to NAC was more accurately predicted using local features, rather than global features. Similarly, in non-small-cell lung cancer patients, local textural features (e.g., contrast, coarseness, and busyness) were superior for prediction of response to NAC [18].
Tumor heterogeneity depends on a variety of tissue components, which affect the heterogeneity of glucose metabolism [11, 16]. Moreover, increased tumor heterogeneity causes poor response to NAC [22]. In the current study, assessment of tumor heterogeneity was performed using 18F-FDG PET images [12, 14]. Entropy (randomness and degree of disorder was used as a representative indicator of tumor heterogeneity. Figure 2 shows that quantitative factors decreased in responder and nonresponder groups. However, none of the assessed features were significantly different in baseline 18F-FDG PET images. In the responder group, 1st entropy and GLCM entropy were significantly different after NAC. This result indicates that change in 18F-FDG uptake heterogeneity can predict the response to NAC and that 1st entropy and GLCM entropy after 18F-FDG PET can predict the response to NAC. The percent changes between baseline and after NAC are shown in Table 2.
The percent change of SUVmax was significantly different between responder and nonresponder groups. Furthermore, SUVmax, TLG, and MTV showed increased predictability in percent change (Table 2). ROC analysis showed that AUCs of 1st entropy and GLCM entropy were not superior to those of SUVmax, TLG, and MTV (Table 2). However, combinations of these features could predict the response to NAC using machine learning methods for analysis of baseline 18F-FDG PET images. Statistical result of all quantitative factors at each time point showed that at individual time points after NAC, 1st entropy and GLCM entropy were significantly different. After NAC, changes in 18F-FDG features SUVmax and MTV were significantly different, based on ROC analysis (p > 0.05). Therefore, we recommend that 18F-FDG PET is used to more accurately evaluate changes in 18F-FDG heterogeneity and predict the response to NAC in osteosarcoma patients.
ROC analysis showed that the percent changes of 18F-FDG textural features had higher AUC values than machine learning without PCA. These results are important for predictions in osteosarcoma patients. However, there is a disadvantage in that early treatment outcomes cannot be estimated because the percent changes of textural features require acquisition of 18F-FDG at baseline and after NAC. Thus, the prediction of prognosis in osteosarcoma patients using percent change of textural features is not useful, even if the prediction exhibits high accuracy. Consequently, machine learning with PCA may be more useful to predict the response to NAC in osteosarcoma patients.
Osteosarcoma is not a common cancer: fewer than 1% of all cancer diagnoses are osteosarcoma [23] and approximately 2% of childhood cancers are osteosarcoma. Therefore, it is difficult to obtain osteosarcoma 18F-FDG PET images and the resulting 18F-FDG PET data are often insufficient for robust analysis.
In this study, machine learning approaches could predict the chemotherapy response before NAC in osteosarcoma patients. However, a major limitation of this study was the insufficient size of the cohort dataset. Because osteosarcoma is an uncommon cancer, there was a restricted amount of 18F-FDG PET data available for our analysis. Therefore, data from a large patient cohort are needed to confirm our findings and provide a more powerful predictive model.
5. Conclusion
There were no significant differences between responders and nonresponders, as measured by 18F-FDG PET at baseline and after NAC. However, the percent change in 18F-FDG heterogeneity of textural features could predict the response to NAC. ROC analysis showed that the AUC of machine learning (linear SVM, random forest, and gradient boost) could predict the response to NAC using textural features in baseline 18F-FDG. We hope that these results help osteosarcoma patients to avoid unnecessary NAC and that they aid in selection of the appropriate treatment method for patients with osteosarcoma by predicting treatment outcomes before the initiation of NAC.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (Ministry of Science and ICT) (2019M2D2A1A02057204) and the Korea Institute of Radiological and Medical Sciences (KIRAMS), funded by Ministry of Science and ICT (MSIT), Republic of Korea (no. 50462-2019).
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
No potential conflicts of interest relevant to this article exist.
Authors' Contributions
Su Young Jeong and Wook Kim contributed equally to this work.
References
- 1.Im H. J., Kim T. S., Park S.-Y., et al. Prediction of tumour necrosis fractions using metabolic and volumetric 18F-FDG PET/CT indices, after one course and at the completion of neoadjuvant chemotherapy, in children and young adults with osteosarcoma. European Journal of Nuclear Medicine and Molecular Imaging. 2012;39(1):39–49. doi: 10.1007/s00259-011-1936-4. [DOI] [PubMed] [Google Scholar]
- 2.Schulte M., Brecht-Krauss D., Werner M., et al. Evaluation of neoadjuvant therapy response of osteogenic sarcoma using FDG PET. Journal of Nuclear Medicine. 1999;40(10):1637–1643. [PubMed] [Google Scholar]
- 3.Cheon G. J., Kim M. S., Lee J. A., et al. Prediction model of chemotherapy response in osteosarcoma by 18F-FDG PET and MRI. Journal of Nuclear Medicine. 2009;50(9):1435–1440. doi: 10.2967/jnumed.109.063602. [DOI] [PubMed] [Google Scholar]
- 4.Uhl M., Saueressig U., Koehler G., et al. Evaluation of tumour necrosis during chemotherapy with diffusion-weighted MR imaging: preliminary results in osteosarcomas. Pediatric Radiology. 2006;36(12):1306–1311. doi: 10.1007/s00247-006-0324-x. [DOI] [PubMed] [Google Scholar]
- 5.Wahl R. L., Jacene H., Kasamon Y., Lodge M. A. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. Journal of Nuclear Medicine. 2009;50(S1):122S–150S. doi: 10.2967/jnumed.108.057307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krause B. J., Schwarzenböck S., Souvatzoglou M. Molecular Imaging in Oncology. Berlin, Germany: Springer; 2013. FDG PET and PET/CT. [Google Scholar]
- 7.Henriksson E., Kjellen E., Wahlberg P., Ohlsson T., Wennerberg J., Brun E. 2-Deoxy-2-[18F] fluoro-D-glucose uptake and correlation to intratumoral heterogeneity. Anticancer Res. 2007;27(4B):2155–2159. [PubMed] [Google Scholar]
- 8.Herrmann K., Benz M., Krause B., Pomykala K., Buck A., Czernin J. 18F-FDG-PET/CT in evaluating response to therapy in solid tumors: where we are and where we can go. Quarterly Journal of Nuclear Medicine and Molecular Imaging. 2011;55(6):620–632. [PubMed] [Google Scholar]
- 9.Burrell R. A., Swanton C. Tumour heterogeneity and the evolution of polyclonal drug resistance. Molecular Oncology. 2014;8(6):1095–1111. doi: 10.1016/j.molonc.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burrell R. A., McGranahan N., Bartek J., Swanton C. The causes and consequences of genetic heterogeneity in cancer evolution. Nature. 2013;501(7467):338–345. doi: 10.1038/nature12625. [DOI] [PubMed] [Google Scholar]
- 11.Haralick R. M., Shanmugam K., Dinstein I. H. Textural features for image classification. IEEE Transactions on Systems, Man, and Cybernetics. 1973;SMC-3(6):610–621. doi: 10.1109/tsmc.1973.4309314. [DOI] [Google Scholar]
- 12.Hyun S. H., Kim H. S., Choi S. H., et al. Intratumoral heterogeneity of 18F-FDG uptake predicts survival in patients with pancreatic ductal adenocarcinoma. European Journal of Nuclear Medicine and Molecular Imaging. 2016;43(8):1461–1468. doi: 10.1007/s00259-016-3316-6. [DOI] [PubMed] [Google Scholar]
- 13.Cook G. J. R., Yip C., Siddique M., et al. Are pretreatment 18F-FDG PET tumor textural features in non-small cell lung cancer associated with response and survival after chemoradiotherapy? Journal of Nuclear Medicine. 2013;54(1):19–26. doi: 10.2967/jnumed.112.107375. [DOI] [PubMed] [Google Scholar]
- 14.Soussan M., Orlhac F., Boubaya M., et al. Relationship between tumor heterogeneity measured on FDG-PET/CT and pathological prognostic factors in invasive breast cancer. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0094017.e94017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatt M., Tixier F., Cheze Le Rest C., Pradier O., Visvikis D. Robustness of intratumour 18F-FDG PET uptake heterogeneity quantification for therapy response prediction in oesophageal carcinoma. European Journal of Nuclear Medicine and Molecular Imaging. 2013;40(11):1662–1671. doi: 10.1007/s00259-013-2486-8. [DOI] [PubMed] [Google Scholar]
- 16.Chicklore S., Goh V., Siddique M., Roy A., Marsden P. K., Cook G. J. R. Quantifying tumour heterogeneity in 18F-FDG PET/CT imaging by texture analysis. European Journal of Nuclear Medicine and Molecular Imaging. 2013;40(1):133–140. doi: 10.1007/s00259-012-2247-0. [DOI] [PubMed] [Google Scholar]
- 17.Lu X., Kang Y. Hypoxia and hypoxia-inducible factors: master regulators of metastasis. Clinical Cancer Research. 2010;16(24):5928–5935. doi: 10.1158/1078-0432.ccr-10-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tixier F., Le Rest C. C., Hatt M., et al. Intratumor heterogeneity characterized by textural features on baseline 18F-FDG PET images predicts response to concomitant radiochemotherapy in esophageal cancer. Journal of Nuclear Medicine. 2011;52(3):369–378. doi: 10.2967/jnumed.110.082404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coffin C. M., Lowichik A., Zhou H. Treatment effects in pediatric soft tissue and bone tumors. American Journal of Clinical Pathology. 2005;123(1):75–90. doi: 10.1309/h0d4-vd76-0nh6-n1r6. [DOI] [PubMed] [Google Scholar]
- 20.Fang Y.-H. D., Lin C.-Y., Shih M.-J., et al. Development and evaluation of an open-source software package “CGITA” for quantifying tumor heterogeneity with molecular images. BioMed Research International. 2014;2014:9. doi: 10.1155/2014/248505.248505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zwanenburg A., Leger S., Vallières M., Löck S. Image biomarker standardisation initiative. December 2016. https://arxiv.org/abs/1612.07003.
- 22.Punt C. J. A., Koopman M., Vermeulen L. From tumour heterogeneity to advances in precision treatment of colorectal cancer. Nature Reviews Clinical Oncology. 2017;14(4):235–246. doi: 10.1038/nrclinonc.2016.171. [DOI] [PubMed] [Google Scholar]
- 23.Harrison D. J., Geller D. S., Gill J. D., Lewis V. O., Gorlick R. Current and future therapeutic approaches for osteosarcoma. Expert Review of Anticancer Therapy. 2018;18(1):39–50. doi: 10.1080/14737140.2018.1413939. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.