Candida auris is an emerging pathogen that has spread rapidly across the globe, including to Canada
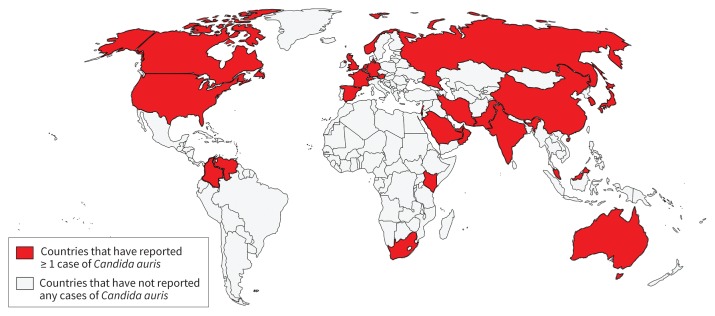
Candida auris was first described in Japan in 2009, but infections have been reported from 32 countries on 5 continents (Figure 1).1 Although the reasons are unclear, C. auris emerged in parallel on 3 continents, then spread to North America through travel.2 In Canada, 19 cases of C. auris have been identified since 2012;3 most patients had received health care abroad.
Figure 1:
Countries reporting at least 1 case of Candida auris through Apr. 15, 2019.
Candida auris can spread efficiently between patients in health care facilities
Outbreaks of C. auris infections have occurred in hospitals and long-term care facilities.4 Candida auris can colonize patient skin for months, and environmental contamination is difficult to eradicate.4 Infected and colonized patients should be isolated with contact precautions in private rooms disinfected daily with sporicides like bleach.4 Notification of infection control and public health is essential.4
Candida auris can cause invasive candidiasis in patients in hospital
Candida auris is an opportunistic pathogen that can cause invasive candidiasis, including candidemia, in patients in hospital, with a high rate of death.4 Risk factors for disease include intensive care, central lines, and antibiotic and antifungal exposure.5
Antifungal resistance of C. auris presents therapeutic challenges
Many C. auris isolates are resistant to antifungals. In most isolates, resistance is seen to fluconazole, in one-third to amphotericin B, and in about 5% to echinocandins. Very rarely, resistance occurs to all antifungal classes.2 Echinocandins are appropriate for empiric therapy pending susceptibility testing.4
Laboratory misidentification of C. auris can delay appropriate therapy and implementation of infection control precautions
Certain biochemical and matrix-assisted laser desorption/ionization time of flight (MALDI-TOF) mass spectrometry identification systems cannot accurately identify C. auris;4 laboratories should refer suspicious isolates to reference laboratories when identification is necessary. Microbiologists should be consulted if unidentified or unusual Candida spp. are isolated from patients who have received health care abroad or are unresponsive to empiric antifungals.4
Footnotes
Competing interests: Ilan Schwartz reports receiving personal fees from AVIR Pharma Inc., outside the submitted work. No other competing interests were declared.
This article has been peer reviewed.
References
- 1.Tracking Candida auris: April 30, 2019: case count updated as of March 31, 2019. Atlanta: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED); 2019. Available: www.cdc.gov/fungal/candida-auris/tracking-c-auris.html (accessed 2019 May 15). [Google Scholar]
- 2.Lockhart SR, Etienne KA, Vallabhaneni S, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis 2017;64:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharat A, Alexander DC, Dingle TC, et al. Candida auris in Canada, 2012–Feb. 2019. Proceedings from the 2019 AMMI Canada — CACMID annual conference; 2019 Apr. 3–6; Ottawa. [Google Scholar]
- 4.Tsay S, Kallen A, Jackson BR, et al. Approach to the investigation and management of patients with Candida auris, an emerging multidrug-resistant yeast. Clin Infect Dis 2018;66:306–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudramurthy SM, Chakrabarti A, Paul RA, et al. Candida auris candidaemia in Indian ICUs: analysis of risk factors. J Antimicrob Chemother 2017;72:1794–801. [DOI] [PubMed] [Google Scholar]