Abstract
Objective
Adverse events (AEs) associated with short-term corticosteroid use for respiratory conditions in young children.
Design
Systematic review of primary studies.
Data sources
Medline, Cochrane CENTRAL, Embase and regulatory agencies were searched September 2014; search was updated in 2017.
Eligibility criteria
Children <6 years with acute respiratory condition, given inhaled (high-dose) or systemic corticosteroids up to 14 days.
Data extraction and synthesis
One reviewer extracted with another reviewer verifying data. Study selection and methodological quality (McHarm scale) involved duplicate independent reviews. We extracted AEs reported by study authors and used a categorisation model by organ systems. Meta-analyses used Peto ORs (pORs) and DerSimonian Laird inverse variance method utilising Mantel-Haenszel Q statistic, with 95% CI. Subgroup analyses were conducted for respiratory condition and dose.
Results
Eighty-five studies (11 505 children) were included; 68 were randomised trials. Methodological quality was poor overall due to lack of assessment and inadequate reporting of AEs. Meta-analysis (six studies; n=1373) found fewer cases of vomiting comparing oral dexamethasone with prednisone (pOR 0.29, 95% CI 0.17 to 0.48; I2=0%). The mean difference in change-from-baseline height after one year between inhaled corticosteroid and placebo was 0.10 cm (two studies, n=268; 95% CI −0.47 to 0.67). Results from five studies with heterogeneous interventions, comparators and measurements were not pooled; one study found a smaller mean change in height z-score with recurrent high-dose inhaled fluticasone over one year. No significant differences were found comparing systemic or inhaled corticosteroid with placebo, or between corticosteroids, for other AEs; CIs around estimates were often wide, due to small samples and few events.
Conclusions
Evidence suggests that short-term high-dose inhaled or systemic corticosteroids use is not associated with an increase in AEs across organ systems. Uncertainties remain, particularly for recurrent use and growth outcomes, due to low study quality, poor reporting and imprecision.
Keywords: corticosteroids, asthma, bronchiolitis, croup, paediatrics, safety
Strengths and limitations of this study.
Examined safety outcomes associated with short-term corticosteroid use across multiple common acute respiratory conditions in young children.
Broad range of adverse events (AEs) captured across organ systems.
Inconsistent definitions, assessments and reporting of AEs.
Extensive variation in corticosteroid formulations and dosages within and between studies.
Did not examine long-term corticosteroid use (>14 days).
Introduction
Corticosteroids are the cornerstone of treatment for many common paediatric respiratory conditions including croup and asthma.1–3 These conditions often result in presentation to urgent and emergency care settings, in otherwise healthy children. Previous studies examining corticosteroid use in chronic asthma have demonstrated the potential for short-term and long-term adverse events (AEs), particularly growth inhibition, bone disease and adrenal suppression.4–6 While corticosteroids have demonstrated effectiveness for the acute treatment of many respiratory indications, clinicians are faced with considerable uncertainty regarding short-term safety, particularly among the youngest children.1
Previous systematic reviews have examined corticosteroids in preschool or school-aged asthma or wheezing4 7 8; however, most focused on efficacy and were restricted to randomised controlled trials (RCTs). These reviews also focused on a specific underlying condition, disease severity, or particular corticosteroid, and mostly for longer-term administration (eg, for recurrent, persistent or chronic asthma). Current guidance on systematic assessment of harms highlights the need to include data from observational studies when considering safety outcomes.9 As well, it has been suggested that it may be useful to have a wider view of the evidence across a number of similar indications.10 Recent knowledge synthesis approaches have studied specific safety outcomes across conditions to increase power, with the assumption that some safety outcomes are not confounded by condition.10 Such a comprehensive approach to knowledge synthesis in this area is critical to inform treatment decisions, reduce practice variation and optimise management of young children who seek care due to acute respiratory illness.
The goal of this study was to synthesise evidence regarding the safety of short course corticosteroid use in young children (<6 years) with acute respiratory conditions.
Methods
This review followed internationally recommended methods and standards for systematic reviews.11–13 An a priori protocol was developed (available from authors).
Patient and public involvement
Patients and/or the public were not involved in the design or conduct of this systematic review.
Literature search
Original database searches were conducted September 2014 in Ovid Medline, the Cochrane Central Register of Controlled Trials (CENTRAL) via Wiley Cochrane Library, and Ovid Embase. Additional sources included regulatory agency databases: Drugs@FDA, Health Canada’s Drug Products Database and the European Medicines Agency’s European Public Assessment Reports. Search strategies combined index terms and keywords for respiratory illnesses, children and drug classes identified in the Global Initiative for Asthma (GINA)14 guidelines. Study design filters were applied to limit results to RCTs and observational studies. Update searches were executed in Medline and CENTRAL in February 2016, and then again in July 2017. Detailed search strategies are in online supplementary file 1.
bmjopen-2018-028511supp001.pdf (123.9KB, pdf)
Eligibility criteria
We included primary studies involving population (P): children up to six years old; intervention (I): treated with single or recurrent systemic (any dose) or high-dose inhaled (as defined by the GINA guidelines14) corticosteroids for up to 14 days; comparator (C): any comparator; outcome (O): any AE; timing (T): any timing; and, setting (S): any inpatient or outpatient setting providing care to children with an acute respiratory condition. See online supplementary file 2 for detailed eligibility criteria.
bmjopen-2018-028511supp002.pdf (111.6KB, pdf)
Given the lack of standardised terminology for safety, we gathered information on all potentially drug-related harm outcomes15 from studies including, but not limited to: adverse drug reactions, adverse drug events, medication errors, side effects and potential adverse drug events. For consistency, these outcomes are referred to in the manuscript as AEs. Studies that did not report or mention AEs were excluded. Due to resource constraints and mean age of the studies, no attempt was made to contact study authors if no harms were reported in the text, or when there was potentially missing data; such efforts are unlikely to yield additional data.
Study selection
Two reviewers independently screened the titles and abstracts of all records using a priori selection criteria. Full texts of potentially eligible studies were reviewed by two reviewers independently using a standard form. Disagreements were resolved through consensus or consultation with a third reviewer.
Data extraction
One reviewer extracted data using a structured form, with verification by a second reviewer. Data were extracted on study characteristics (design features), patient characteristics (age, sex, baseline characteristics), respiratory conditions, interventions (type, dose, duration, route of administration, timing, cointerventions, rescue medications), outcomes (types and timing), care setting, funding sources and results.
AEs were extracted as reported by study authors and categorised using a published model based on organ systems (see Results section).16 A panel of clinicians with specialties in paediatrics, emergency medicine, respiratory medicine and clinical pharmacology rated each AE in order of clinical severity independent of knowledge of the study results.
Assessment of methodological quality
Two reviewers independently assessed the methodological quality of studies using the McMaster Quality Assessment Scale for Harms (McHarm)17; disagreements were resolved through discussion.
Data synthesis
A comparative summary of AEs for studies with more than one treatment arm was presented to provide an overall picture of which interventions had a high risk of specific AEs. Risk differences were pooled using the DerSimonian Laird inverse variance random-effects method utilising the Mantel-Haenszel Q statistic. Binary data were also pooled using the Peto ORs (pORs) fixed-effects method.18 Studies that reported at least one event in at least one treatment arm were included in the analysis of pORs and all comparative studies were used for analysis of RD. One AE (growth) was reported as a continuous outcome and data were pooled using a DerSimonian Laird inverse variance random effects method as a mean difference (MD; in cm). The I2 statistic was presented to quantify the magnitude of statistical heterogeneity between studies; while the I2 has the potential to be misinterpreted, it is the standard in the field and we chose to present the statistic for informational purposes.19 Subgroup analyses from study-level data were conducted for respiratory condition and dose (single vs multidose) using Cochran’s Q (α=0.05) to detect statistical heterogeneity. Studies contributing no numerical data for analysis (eg, single arm studies, studies that reported no AEs overall) are summarised in online supplementary file 3. Assessment of small-study bias (for meta-analyses with at least eight studies) was planned using the funnel plot and Egger’s test20; however, this was not conducted due to inadequate number of studies for each outcome. Analyses were conducted using Review Manager V.5.3 (Cochrane Collaboration).21 Graphs were constructed using TIBCO Spotfire S+Workbench V.3.4.22
bmjopen-2018-028511supp003.pdf (411.9KB, pdf)
Results
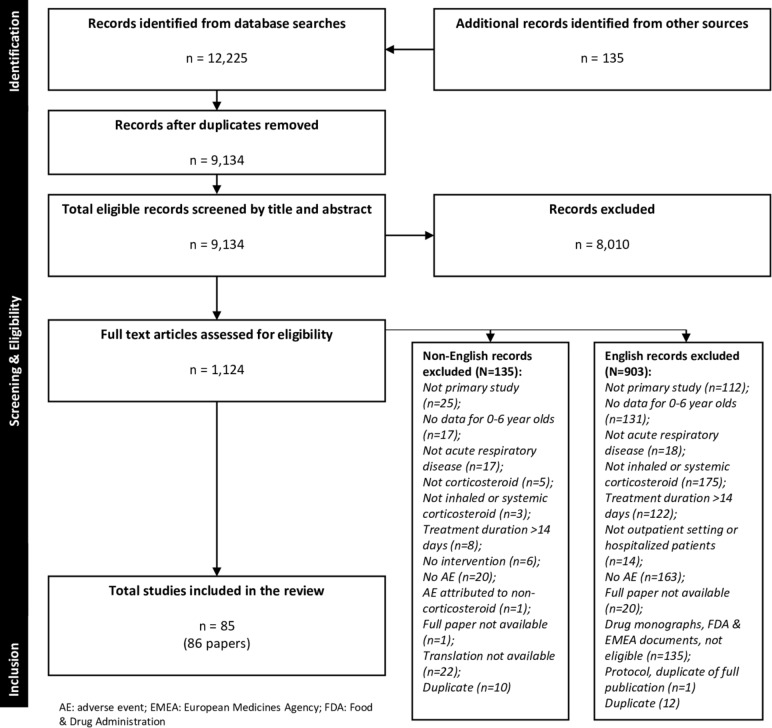
Database and grey literature searches yielded 9134 records. Eighty-six papers (85 studies)23–108 involving 11 505 participants were included (figure 1). Characteristics of the included studies are in online supplementary file 3. There was large variation in corticosteroid type, dose, duration and route of administration, both for systemic and inhaled corticosteroids. Methodological quality of studies was poor overall due to inadequate reporting of how AEs were defined and collected (table 1; online supplementary file 4).
Figure 1.
PRISMA study flow selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Summary of methodological quality assessments
| McHarm* criteria | Rating | No of studies (%†) |
| (1) Were the harms PRE-DEFINED using standardised or precise definitions? | Yes | 6 (7) |
| No | 79 (93) | |
| Unsure | 0 | |
| (2) Were SERIOUS events precisely defined? | Yes | 2 (2) |
| No | 83 (98) | |
| Unsure | 0 | |
| (3) Were SEVERE events precisely defined? | Yes | 0 |
| No | 85 (100) | |
| Unsure | 0 | |
| (4) Were the number of DEATHS in each study group specified OR were the reason(s) for not specifying them given? | Yes | 10 (12) |
| No | 75 (88) | |
| Unsure | 0 | |
| (5) Was the mode of harms collection specified as ACTIVE? | Yes | 46 (54) |
| No | 37 (44) | |
| Unsure | 2 (2) | |
| (6) Was the mode of harms collection specified as PASSIVE? | Yes | 11 (13) |
| No | 73 (86) | |
| Unsure | 1 (1) | |
| (7) Did the study specify WHO collected the harms? | Yes | 22 (26) |
| No | 63 (74) | |
| Unsure | 0 | |
| (8) Did the study specify the TRAINING or BACKGROUND of who ascertained the harms? | Yes | 20 (24) |
| No | 65 (76) | |
| Unsure | 0 | |
| (9) Did the study specify the TIMING and FREQUENCY of collection of the harms? | Yes | 39 (46) |
| No | 45 (53) | |
| Unsure | 1 (1) | |
| (10) Did the author(s) use STANDARD scale(s) or checklist(s) for harms collection? | Yes | 6 (7) |
| No | 76 (89) | |
| Unsure | 3 (4) | |
| (11) Did the authors specify if the harms reported encompass ALL the events collected or a selected SAMPLE? | Yes | 80 (94) |
| No | 2 (2) | |
| Unsure | 3 (4) | |
| (12) Was the NUMBER of participants that withdrew or were lost to follow-up specified for each study group? | Yes | 24 (28) |
| No | 61 (72) | |
| Unsure | 0 | |
| (13) Was the TOTAL NUMBER of participants affected by harms specified for each study arm? | Yes | 16 (19) |
| No | 69 (81) | |
| Unsure | 0 | |
| (14) Did the author(s) specify the NUMBER for each TYPE of harmful event for each study group? | Yes | 43 (51) |
| No | 39 (46) | |
| Unsure | 3 (4) | |
| (15) Did the author(s) specify the type of analyses undertaken for harms data? | Yes | 10 (12) |
| No | 75 (88) | |
| Unsure | 0 |
*Methodological quality of publications/studies as assessed by the McHarm scale.17
†Sum of percentages may not total 100 due to rounding.
bmjopen-2018-028511supp004.pdf (159.9KB, pdf)
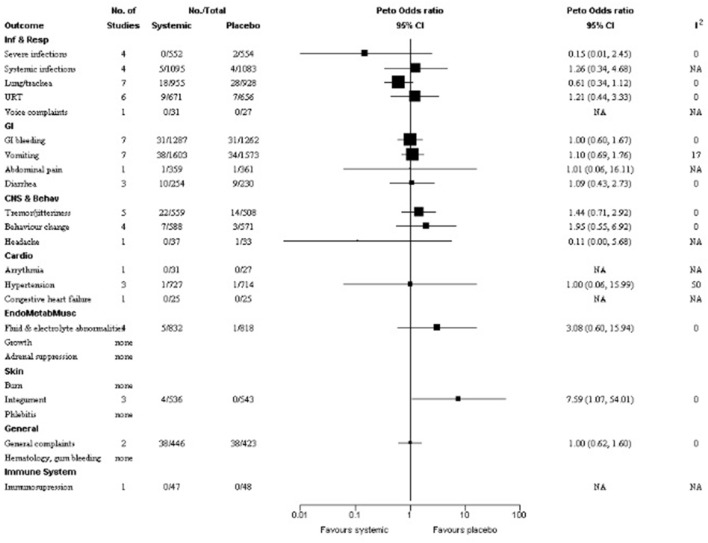
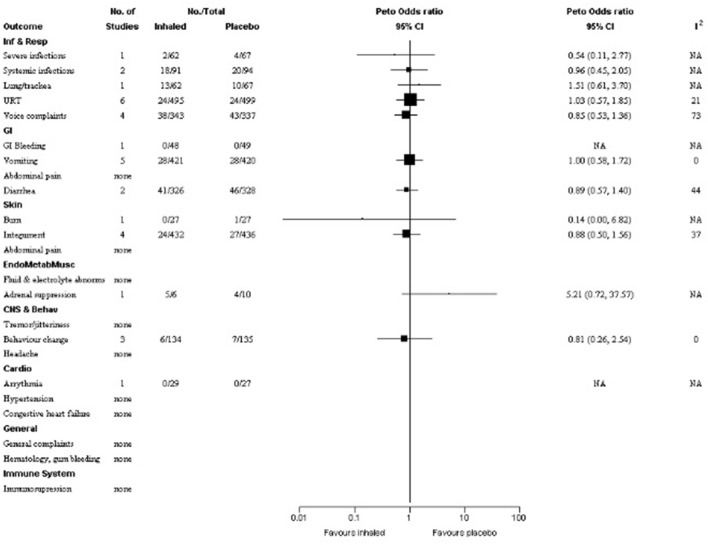
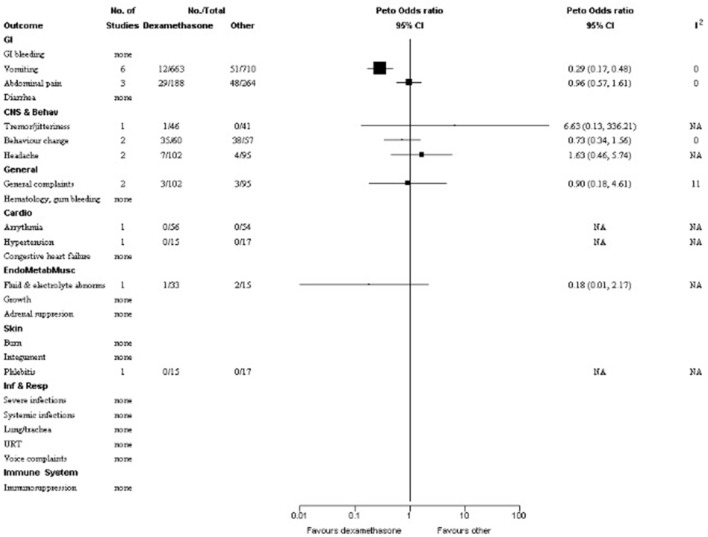
Adverse events
Results below are presented according to the categories in table 2. Figures 2, 3 and 4 display forest plots of AEs comparing systemic corticosteroid to placebo, inhaled corticosteroid to placebo, and systemic dexamethasone to another systemic corticosteroid, respectively. Results of meta-analyses and subgroup analyses are in online supplementary file 5, with effect estimates and 95% CIs. Forest plots from meta-analyses are in online supplementary file 6. There was large variation in the number of studies and number of patients with available data for meta-analysis across comparisons and outcomes. Further, for four safety outcomes there were no events in both study arms (double-zero) across studies. In most cases, the subgroup analyses by dose and condition did not differ substantially from the overall results. Studies reporting no AEs overall are summarised in online supplementary file 7.
Table 2.
Number of studies and participants reporting adverse events*
| Organ system | AE—category | AE—specific | No of studies | No of participants |
| Infection and respiratory GI |
Severe infections | 5 | 1235 | |
| (1) | Sepsis | 1 | 32 | |
| (2) | Superinfection | 2 | 354 | |
| (3) | UTI | 1 | 720 | |
| (4) | Streptococcal infection | 1 | 129 | |
| Systemic infections | 5 | 1635 | ||
| (1) | Fever | 3 | 963 | |
| (2) | Common viral/bacterial/fungal infection | 2 | 792 | |
| (3) | Varicella | 3 | 1449 | |
| Lung/trachea | 10 | 2053 | ||
| (1) | Empyema | 1 | 600 | |
| (2) | Pneumonia | 8 | 2051 | |
| (3) | Respiratory distress | 2 | 2 | |
| Upper respiratory tract | 14 | 2457 | ||
| (1) | Bacterial tracheitis | 5 | 1023 | |
| (2) | Sinusitis | 2 | 849 | |
| (3) | Croup | 2 | 131 | |
| (4) | Viral parotitis | 1 | 27 | |
| (5) | Pharyngitis | 1 | 129 | |
| (6) | Persistent cough | 1 | 27 | |
| (7) | Oral thrush | 3 | 837 | |
| (8) | Otitis media | 4 | 1173 | |
| (9) | Ear, nose, throat infection | 3 | 862 | |
| (10) | Nasal discharge | 1 | 720 | |
| (11) | Eye discharge | 1 | 720 | |
| Voice complaints | 5 | 794 | ||
| GI bleeding | 8 | 2669 | ||
| (1) | Bleeding | 5 | 1577 | |
| (2) | Gross hematochezia | 1 | 118 | |
| (3) | Occult blood in stools | 2 | 292 | |
| (4) | Dark stools | 1 | 800 | |
| Vomiting | 27 | 6067 | ||
| (1) | Vomiting | 24 | 5983 | |
| (2) | Nausea | 6 | 586 | |
| (3) | Palatability | 3 | 170 | |
| Abdominal pain | 5 | 1332 | ||
| Diarrhoea | 8 | 1346 | ||
| (1) | Diarrhoea | 7 | 1217 | |
| (2) | Gastroenteritis | 1 | 129 | |
| CNS and behaviour | Tremor/jitteriness | 8 | 1274 | |
| (1) | Tremor | 7 | 1226 | |
| (2) | Jittery | 1 | 48 | |
| Behaviour change | 14 | 2078 | ||
| (1) | Violent behaviour | 1 | 198 | |
| (2) | Mood change | 7 | 1430 | |
| (3) | Hyperactivity | 2 | 268 | |
| (4) | Restlessness | 3 | 297 | |
| (5) | New sleep problems | 3 | 408 | |
| (6) | Emotional distress due to nebulizer mask | 1 | 82 | |
| (7) | Psychosis | 1 | 1 | |
| Headache | 3 | 291 | ||
| Dermatological | Burn | 1 | 198 | |
| Integument | 10 | 1954 | ||
| (1) | Hives | 2 | 199 | |
| (2) | Rash | 8 | 1954 | |
| (3) | Eczema | 1 | 129 | |
| (4) | Eye irritation | 2 | 211 | |
| (5) | Tongue irritation | 1 | 82 | |
| (6) | Positive weal | 1 | 1 | |
| (7) | Bleeding from ear | 1 | 720 | |
| Phlebitis | 1 | 32 | ||
| Endocrine/metabolic and musculoskeletal | Fluid and electrolyte abnormalities | 7 | 1849 | |
| (1) | Hyperkalemia | 1 | 800 | |
| (2) | Hyperglycemia | 3 | 154 | |
| (3) | Glycosuria | 1 | 125 | |
| (4) | Sodium retention | 1 | 50 | |
| (5) | Dehydration | 1 | 720 | |
| Growth | 6 | 731 | ||
| Adrenal suppression | 5 | 249 | ||
| Bone health | 5 | 579 | ||
| Cardiovascular | Arrhythmia | 3 | 312 | |
| (1) | Tachycardia | 2 | 178 | |
| (2) | Palpitations | 1 | 134 | |
| Hypertension | 5 | 1491 | ||
| Congestive heart failure | 1 | 50 | ||
| General | General complaints | 5 | 1146 | |
| (1) | Dizziness | 1 | 87 | |
| (2) | Pallor | 2 | 869 | |
| (3) | Excessive urination | 1 | 134 | |
| (4) | Normal tooth eruption | 1 | 56 | |
| Haematology, gum bleeding | 1 | 1 | ||
| Immune system and oncology | Immunosuppression | 4 | 147 | |
| (1) | Immunosuppression | 3 | 146 | |
| (2) | Tumour cell proliferation | 1 | 1 |
*Each adverse event was clustered into its related organ system; a panel of clinicians ranked each AE category and its corresponding adverse events in order of clinical significance/severity. The organ systems are presented in order of frequency of reporting, beginning with the most frequently reported (ie, infection and respiratory).
AE, adverse event; CNS, central nervous system; GI, gastrointestinal; URT, upper respiratory tract.
Figure 2.
Forest plot of adverse events—systemic versus placebo.
Figure 3.
Forest plot of adverse events—inhaled versus placebo.
Figure 4.
Forest plot of adverse events—dexamethasone versus other.
bmjopen-2018-028511supp005.pdf (217.8KB, pdf)
bmjopen-2018-028511supp006.pdf (1.5MB, pdf)
bmjopen-2018-028511supp007.pdf (88.1KB, pdf)
Infections and respiratory system
The number of studies contributing to each meta-analysis ranged from one to seven (range 58–2178 children). There were no statistically significant differences between: (1) systemic corticosteroid compared with placebo for severe infections,30 74 96 99 systemic infections,30 40 43 83 infections of the lung/trachea30 40 54 74 96 98 105 and the upper respiratory tract,30 43 54 65 67 74 and voice complaints43 (estimated pORs between 0.15 and 1.26) and (2) inhaled corticosteroid compared with placebo for severe infections,45 systemic infections,43 45 lung/trachea,45 infections of the upper respiratory tract37 44 45 65–67 or voice complaints37 43 100 101 (estimated pORs between 0.54 and 1.51). No study comparing dexamethasone with another corticosteroid reported infections or respiratory AEs.
Gastrointestinal tract
The number of studies contributing to each meta-analysis ranged from one to seven (range 97–3176 children). There were no statistically significant differences between: (1) systemic corticosteroid and placebo for gastrointestinal (GI) bleeding,30 32 40 65 83 87 105 vomiting,30 38 40 42 70 81 83 abdominal pain30 or diarrhoea42 77 105 and (2) inhaled corticosteroid and placebo for GI bleeding,65 vomiting37 45 69 85 101 or diarrhoea.37 45 Estimated pORs for both comparisons ranged from 0.89 to 1.10.
Meta-analysis of six studies (1373 children)25 27 41 49 52 80 found fewer cases of vomiting in patients who received dexamethasone compared with another corticosteroid, although the number of events was small (12/663 vs 51/710 cases; pOR 0.29, 95% CI 0.17 to 0.48; I2=0%). These studies focused on asthma (n=3),27 41 80 croup (n=2)49 52 or both (n=1)25; all compared oral dexamethasone with oral prednisone. No statistically significant difference was found for abdominal pain between dexamethasone and another corticosteroid.25 27 52
CNS and behaviour effects
The number of studies for each meta-analysis ranged from one to five (range 70–1159 children). The estimated pORs for the systemic corticosteroid and placebo were 1.44 for tremor/jitteriness,38 55 70 77 83 1.95 for behaviour change30 42 67 77 and 0.11 for headache,38 with no statistically significant differences. There were also no differences between inhaled corticosteroid and placebo for behaviour change67 85 101; and dexamethasone and another corticosteroid for behaviour change,52 57 headache27 52 or tremor/jitteriness,52 the latter with an estimated pOR of 6.63 from a small study (n=87) with only one reported event.
Dermatologic conditions
The number of studies per meta-analysis ranged from one to four (range 32–1079 children). There were no statistically significant differences between: (1) systemic corticosteroid and placebo for rash and hives,30 42 67 albeit with an estimated pOR of 7.59 (4/536 vs 0/543; 95% CI 1.07 to 54.01) and (2) inhaled corticosteroid and placebo for rash,37 45 85 hives67 and burning sensation68 (estimated pORs 0.88 and 0.14, respectively). No events of phlebitis were reported comparing dexamethasone to another corticosteroid. 57
Endocrine/metabolic and musculoskeletal systems
There were no statistically significant differences for electrolyte abnormalities between systemic corticosteroid and placebo (estimated pOR 3.08)30 47 83 102 and dexamethasone to another corticosteroid (estimated pOR 0.18).102
Pooled data for linear growth between inhaled corticosteroid and placebo included two studies (n=263) using recurrent doses for acute wheeze with follow-up at one year.28 45 The estimated change-from-baseline height was small (MD 0.10 cm; 95% CI −0.47 to 0.67; I2=9%). Five studies reported measurements of growth (height and weight) ranging from one to three years of follow-up, which could not be pooled due to heterogeneous interventions, comparators or outcome measurements.29 31 45 58 71 Three studies included data on inhaled corticosteroid versus placebo. One RCT on asthma58 (n=20) comparing budesonide and placebo found no signs of growth retardation by height measurements at 12 months or after up to six treatments. An RCT of episodic wheeze29 (n=294) found height at three years of age was unaffected in children receiving budesonide or placebo. One RCT of inhaled fluticasone propionate at very high doses (1500 μg per day during upper respiratory infections) versus placebo in recurrent wheeze45 reported additional outcome data on height that was not pooled in the meta-analysis mentioned above. There was a smaller mean change in height z score in the corticosteroid group over one year (MD −0.24; 95% CI −0.40 to −0.08; adjusted results).45 Furthermore, mean weight was significantly lower at one-year follow-up in the fluticasone group (n=62) versus placebo (n=67); two children given fluticasone and one given placebo met criteria for ‘failure to thrive’.45 Finally, two small trials did not report group differences for other comparisons: total and mean height growth (at 8–19 months) for intravenous dexamethasone versus inhaled budesonide in asthma (n=18)71; weight and height gains at 2 years for theophylline and metaproterenol with or without systemic prednisone on prevention of wheeze during upper respiratory infections in asthma (n=32).31
Five studies reported on adrenal function/suppression, with few children contributing data for this outcome.45 57 58 71 89 The RCT of high-dose inhaled fluticasone propionate versus placebo (99 children with data)45 found no significant differences between groups in basal cortisol (baseline and 12 months). Another RCT in asthma reported no differences in serum cortisol and urinary cortisol/creatinine after 10 days of inhaled budesonide or placebo (16 children with data). A subgroup who received oral betamethasone (n=9) showed significant changes from baseline after three days, but no differences at 12–14 days.58 Two studies included comparisons between different corticosteroids. One RCT89 in acute asthma compared intravenous prednisolone (n=20) with nebulised budesonide (n=30) and found significant levels of suppressed serum cortisol in the prednisolone group, although not considered pathologic by the study authors. Although another RCT57 comparing intramuscular dexamethasone with oral prednisone for asthma (n=32) found lower median urinary cortisol/creatinine in the former group at day 14, there was no statistically significant difference. An RCT71 comparing intravenous dexamethasone (n=9) with inhaled budesonide (n=9) found no significant differences between groups from baseline for blood pressure and blood glucose measurements.
Five studies reported on bone health biomarkers, three of which compared inhaled corticosteroids and placebo; no pooled analyses were performed.29 45 58 61 92 One RCT29 compared inhaled budesonide (n=294) with placebo in episodic wheeze and found no effect on bone mineral density over three years. The RCT comparing high-dose inhaled fluticasone propionate with placebo (n=59 children with data) in viral wheeze45 reported no statistically significant differences between groups in lumbar bone mineral density, bone mineral content or bone age at 12 months. A small RCT58 comparing inhaled budesonide with placebo (n=20) in asthma found transient decreased levels of bone and collagen markers post-treatment and in a subset of children who received oral betamethasone, with no difference between groups. A study of patients with acute respiratory illness92 compared hydrocortisone (n=28), methylprednisone (n=21) and controls (n=51) and found decreased levels of osteocalcin and alkaline phosphatase in younger children 2 days post-treatment; these effects were reversed 12 days after treatment. A non-randomised controlled trial of 36 asthma patients61 compared intravenous methylprednisolone of three different durations and found that all had decreasing levels of serum osteocalcin that correlated with increasing duration of treatment.
Cardiovascular system
No significant differences were found between systemic corticosteroid and placebo in three bronchiolitis studies reporting hypertension (estimated pOR 1).32 40 83 Single studies with up to 110 children did not report events for arrhythmia43 and congestive heart failure47 (systemic or inhaled corticosteroid vs placebo); and arrhythmia27 or hypertension57 (dexamethasone with another corticosteroid).
General AEs/other symptoms
Meta-analyses included a total of two studies (range 197–869 children). There were no statistically significant differences between: (1) systemic corticosteroid and placebo for pallor70 83 and (2) dexamethasone and another corticosteroid for dizziness52 or excessive urination.27 No study comparing inhaled corticosteroid with placebo reported general AEs.
Immune system and oncology
One study (95 participants)39 compared systemic corticosteroid and placebo and found no occurrences of immunosuppression. No other study reported immune system-related AEs.
Discussion
This systematic review of studies in which short-course corticosteroids were administered to children under six years of age for acute respiratory conditions, included 85 studies involving more than11 000 patients. These studies used a variety of delivery routes, doses, formulations and duration of corticosteroids. Overall, the evidence suggests that short-term corticosteroid use is not associated with a significant increase in AEs across organ systems. However, given the low quality of included studies, the heterogeneous and poor reporting of AEs, and the lack of precision of results, considerable uncertainties remain regarding the safety of high-dose inhaled or systemic corticosteroids for these indications in this age range.
A common concern when using corticosteroids in young children is effect on growth. Results from a single, small trial (n=129) of recurrent high-dose inhaled fluticasone propionate in wheezing preschoolers were heterogeneous across outcome measures, but suggested a small significant risk of growth suppression.45 Observational data have also suggested that multiple corticosteroid bursts can increase the risk of growth suppression, fractures, bone mineral accretion and osteopenia in children with underlying respiratory disease.5 6 109 Conversely, a pooled analysis using change-from-baseline linear growth did not find significant differences, although the other included study used a substantially lower equivalent dose of inhaled corticosteroid.110 Further, results from individual studies reporting transient differences in bone and adrenal biomarkers are of unclear clinical relevance, particularly for previously healthy children and single use. This calls for caution and monitoring of linear growth, particularly when use of high-dose inhaled or systemic corticosteroid is recurrent.
We found no other statistically significant differences between systemic or inhaled corticosteroid and placebo, or between dexamethasone and other systemic corticosteroid, including subgroup analyses by respiratory condition or dose, for AEs across organ systems. Due to small sample sizes and low number of events, these results should be interpreted with caution. While we found increased pORs when comparing systemic corticosteroids for behavioural outcomes such as tremor/jitteriness and behaviour change, there were wide CIs around estimates. No study examined neurodevelopmental outcomes after corticosteroid administration; ideally, studies should assess children for potentially related long-term AEs using validated instruments in this domain. Results from case series and case reports added anecdotal evidence of rare cases of hypersensitivity, infection or behavioural AEs, which have been described.111 112 While the estimated increased pOR for rash and hives was close to statistical significance, no other differences were found in systemic or severe infections as well as immunosuppression.
This review did not ascertain a clear safety advantage between systemic or inhaled corticosteroids compared with placebo. When comparing between different systemic corticosteroids, evidence favoured oral dexamethasone over oral prednisone for vomiting (pOR 0.029; 95% CI 0.17 to 0.48; I2=0%). Differences in palatability and tolerability between corticosteroids are well known to parents, healthcare providers and researchers, and can influence adherence to medication in children.113 Further, different specific formulations of corticosteroid (eg, prednisolone tablets vs prednisolone syrup) have been shown to influence taste and vomiting.25 However, cost and access to better tolerated formulations may be problematic. Subgroup analyses also found no significant differences between groups by respiratory condition or dose (single vs multiple) for these outcomes. Due to extensive variation in dosing within and across studies, we were unable to analyse data or draw further conclusions with respect to dosage or differences between specific molecules. It should be noted that among the eight RCTs35 43 46 51 65 67 71 89 directly comparing systemic and inhaled routes of corticosteroid administration, none contributed meaningful data for meta-analysis. The decision to initiate corticosteroid and the selection of drug, dose and mode of administration must consider these uncertainties on harms, as well as existing evidence on comparative potency and clinical effectiveness. The risk–benefit rationale is less established for repeated acute use in younger children, such as in recurrent wheezing.114
Strengths and limitations
We conducted a comprehensive systematic review of the literature following rigorous methods, including grey literature, to minimise potential for publication and selection bias. We examined safety outcomes across multiple acute respiratory conditions using ‘baskets’ of outcomes in each organ system to increase our ability to detect rare events and the precision of our estimates.16 This approach is reflective of clinical practice where corticosteroids are used across many respiratory diseases, even if the evidence base is not entirely robust for children. A recent systematic review also assessed the toxicity of short-course oral corticosteroids in children across clinical conditions.115 However, there was scarce overlap in respiratory conditions across included studies, and authors mostly provided estimates of the incidence of AEs within treatment groups rather than comparative treatment effects. Studies in adults have also adopted similar approaches to estimate incidence rates of AEs. For example, findings from a recent retrospective cohort in adults showed a significant increase in rates of sepsis, venous thromboembolism and fracture.116
This review was limited by the quality of the primary literature, particularly regarding the definition, assessment and reporting of AEs. This underscores the challenges researchers encounter when attempting to synthesise safety data due to sparse and poor reporting,117 and highlights the urgent need to enhance detection and reporting of AEs. For example, it is worthwhile noting that 26 studies reported ‘no AEs’ or ‘no significant AE’ which could not be included in pooled estimates; this may be a reflection of these studies being under-powered to detect statistically significant findings (especially for rare AEs) and/or AEs that may or may not be considered of special interest and/or clinically important. Such blanket statements are problematic for interpretation, highlighting the need for study authors to clearly report AEs of interest pre-study and post-study conduct. Common nomenclature (eg, www.meddra.org) and standardised approaches to collection of AE data should be implemented to help draw comparisons across studies. Further, safety reporting was not a primary focus of the studies, AEs were rarely defined a priori, and methods for ascertaining AEs were usually absent. While the McHarm scale is recommended to be used in conjunction with other quality assessment tools to evaluate the broader elements of study quality, we used it exclusively to assess methodological quality since the primary focus of this review was on AEs. The AEs reported typically reflect what is detected by a healthcare provider; it is difficult to discern what is reported by patients as well as what patients consider important. The duration of surveillance of most studies was insufficient to detect many of the long-term AEs potentially associated with corticosteroid use. Although the present study suggests that single doses of systemic or inhaled corticosteroids may result in few AEs, recurrent courses may lead to long-term risks, as cumulative dosing has been shown to be a determinant of safety.109 Finally, there was variation within and across studies with respect to maintenance corticosteroids, and concomitant and rescue medications. Due to the variation in corticosteroids and extensive range of AEs reported (including when a single study contributes to an outcome or in cases of zero events, where meta-analysis was not feasible or meaningful) among varied study designs of overall poor quality, we did not attempt to rate the quality of the body of the evidence using the Grading of Recommendations Assessment, Development and Evaluation118 approach.
Conclusion
This is the most comprehensive systematic review to date examining the safety of corticosteroids for managing acute respiratory conditions among young children, an age group of great clinical concern. While the existing evidence suggests that short-term high-dose inhaled or systemic corticosteroids is not associated with an increase in AEs across organ systems, uncertainties remain due to low quality of studies, poor reporting and lack of precision of results. Importantly, these results can help guide future research in the collection and reporting of AEs, particularly concerning measures of growth and behavioural outcomes; this in turn is needed to help inform shared decision-making between clinicians and parents/caregivers of young children.
Supplementary Material
Acknowledgments
We gratefully acknowledge the following individuals for their contributions: Megan Nuspl, Sanjaya Dhakal and Pritam Chordiya for assisting with screening, initial data extraction and verification, and article retrieval; Marc Parsons for assisting with data extraction and verification, and quality assessment; and, Jack Yeung, Marta Oleszczuk and Igor Pravdivyi for assistance with translations. MN, SD, PC and MP received remuneration for their work from a Canadian Institutes of Health Research (CIHR) grant (funding reference number KRS134306). JY, MO and IP did not receive remuneration for the translation work.
Footnotes
Contributors: RMF, AW, BV, SA, ACP, ASS, BHR, DWJ, DA, TPK and LH critically reviewed and contributed to drafts of the report. RF conducted the literature searches. AW conducted screening, quality assessments and data extraction. AW and BV conducted data synthesis/analysis. RMF, AW, BV, SA, ACP, ASS, BHR, DWJ, DA, TPK and LH contributed to interpretation of results. All of the authors approved the final version of this report.
Funding: This study was funded by a Knowledge Synthesis Grant from CIHR (funding reference number KRS134306). The funder had no role in the design of the study, the collection, analysis or interpretation of data, the writing of the report or the decision to submit the paper for publication.
Competing interests: All authors declare funding from CIHR for the submitted work. LH was funded in part by a New Investigator Salary Award from the CIHR. ACP is supported by a Tier II University of Ottawa Research Chair Award. BHR was supported by a Tier I Canada Research Chair in Evidence-based Emergency Medicine from CIHR. The remaining authors have no financial relationships relevant to this manuscript to disclose. DWJ, TPK and ACP are also authors on some of the included studies.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: LH had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Data for this systematic review (using published data) are available from the corresponding author upon reasonable request.
Patient consent for publication: Not required.
References
- 1. de Benedictis FM, Bush A. Corticosteroids in respiratory diseases in children. Am J Respir Crit Care Med 2012;185:12–23. 10.1164/rccm.201107-1174CI [DOI] [PubMed] [Google Scholar]
- 2. Johnson D. Croup. BMJ Clin Evid 2009;2009. [PMC free article] [PubMed] [Google Scholar]
- 3. Russell KF, Liang Y, O’Gorman K, et al. . Glucocorticoids for croup. Cochrane Database Syst Rev 2011;1:CD001955. [DOI] [PubMed] [Google Scholar]
- 4. Adams NP, Bestall JC, Jones P, et al. . Fluticasone at different doses for chronic asthma in adults and children. Cochrane Database Syst Rev 2008:CD003534 10.1002/14651858.CD003534.pub3 [DOI] [PubMed] [Google Scholar]
- 5. Kelly HW, Sternberg AL, Lescher R, et al. . Effect of inhaled glucocorticoids in childhood on adult height. N Engl J Med 2012;367:904–12. 10.1056/NEJMoa1203229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Staa TP, Cooper C, Leufkens HG, et al. . Children and the risk of fractures caused by oral corticosteroids. J Bone Miner Res 2003;18:913–8. 10.1359/jbmr.2003.18.5.913 [DOI] [PubMed] [Google Scholar]
- 7. Castro-Rodriguez JA, Rodrigo GJ. Efficacy of inhaled corticosteroids in infants and preschoolers with recurrent wheezing and asthma: a systematic review with meta-analysis. Pediatrics 2009;123:e519–e525. 10.1542/peds.2008-2867 [DOI] [PubMed] [Google Scholar]
- 8. Zhang L, Axelsson I, Chung M, et al. . Dose response of inhaled corticosteroids in children with persistent asthma: a systematic review. Pediatrics 2011;127:129–38. 10.1542/peds.2010-1223 [DOI] [PubMed] [Google Scholar]
- 9. Loke YK, Price D, Herxheimer A. Systematic reviews of adverse effects: framework for a structured approach. BMC Med Res Methodol 2007;7:1–9. 10.1186/1471-2288-7-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Singh JA, Wells GA, Christensen R, et al. . Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev 2011;2:CD008794 10.1002/14651858.CD008794.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Higgins J, Green S. The Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [updated March 2011]. The Cochrane Collaboration. 2011. www.cochrane-handbook.org
- 12. Moher D, Liberati A, Tetzlaff J, et al. . PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 13. Zorzela L, Loke YK, Ioannidis JP, et al. . PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ 2016;352:i157 10.1136/bmj.i157 [DOI] [PubMed] [Google Scholar]
- 14. Global Initiative for Asthma. Global strategy for asthma management and prevention. http://www.ginasthma.org (Accessed 12 Jan 2018).
- 15. Nebeker JR, Barach P, Samore MH. Clarifying adverse drug events: a clinician’s guide to terminology, documentation, and reporting. Ann Intern Med 2004;140:795–801. 10.7326/0003-4819-140-10-200405180-00009 [DOI] [PubMed] [Google Scholar]
- 16. Tugwell P, Judd MG, Fries JF, et al. . Powering our way to the elusive side effect: a composite outcome ’basket' of predefined designated endpoints in each organ system should be included in all controlled trials. J Clin Epidemiol 2005;58:785–90. 10.1016/j.jclinepi.2004.11.028 [DOI] [PubMed] [Google Scholar]
- 17. Chou R, Aronson N, Atkins DL, et al. . Assessing harms when comparing medication interventions Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality (US), 2008. [Google Scholar]
- 18. Bradburn MJ, Deeks JJ, Berlin JA, et al. . Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med 2007;26:53–77. 10.1002/sim.2528 [DOI] [PubMed] [Google Scholar]
- 19. Hedges LV. Comment on ’Misunderstandings about Q and "Cochran’s Q Test" in meta analysis'. Stat Med 2016;35:496–7. 10.1002/sim.6763 [DOI] [PubMed] [Google Scholar]
- 20. Egger M, Davey Smith G, Schneider M, et al. . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. The Cochrane Collaboration. Review Manager (RevMan) [computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, 2014. [Google Scholar]
- 22. TS Inc. TIBCO Spotfire S+ Workbench, Version 3.4 [statistical software], 1996. [Google Scholar]
- 23. Alangari AA, Malhis N, Mubasher M, et al. . Budesonide nebulization added to systemic prednisolone in the treatment of acute asthma in children: a double-blind, randomized, controlled trial. Chest 2014;145:772–8. 10.1378/chest.13-2298 [DOI] [PubMed] [Google Scholar]
- 24. Alansari K, Sakran M, Davidson BL, et al. . Oral dexamethasone for bronchiolitis: a randomized trial. Pediatrics 2013;132:e810–e816. 10.1542/peds.2012-3746 [DOI] [PubMed] [Google Scholar]
- 25. Aljebab F, Alanazi M, Choonara I, et al. . Observational study on the palatability and tolerability of oral prednisolone and oral dexamethasone in children in Saudi Arabia and the UK. Arch Dis Child 2018;103:83–8. 10.1136/archdischild-2017-312697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alshehr M, Almegamsi T, Hammdi A. Efficacy of a small dose of oral dexamethasone in croup. Biomed Res 2005;16:65–72. [Google Scholar]
- 27. Altamimi S, Robertson G, Jastaniah W, et al. . Single-dose oral dexamethasone in the emergency management of children with exacerbations of mild to moderate asthma. Pediatr Emerg Care 2006;22:786–93. 10.1097/01.pec.0000248683.09895.08 [DOI] [PubMed] [Google Scholar]
- 28. Bacharier LB, Phillips BR, Zeiger RS, et al. . Episodic use of an inhaled corticosteroid or leukotriene receptor antagonist in preschool children with moderate-to-severe intermittent wheezing. J Allergy Clin Immunol 2008;122:1127–35. 10.1016/j.jaci.2008.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bisgaard H, Hermansen MN, Loland L, et al. . Intermittent inhaled corticosteroids in infants with episodic wheezing. N Engl J Med 2006;354:1998–2005. 10.1056/NEJMoa054692 [DOI] [PubMed] [Google Scholar]
- 30. Bjornson CL, Klassen TP, Williamson J, et al. . Pediatric emergency research canada network. A randomized trial of a single dose of oral dexamethasone for mild croup. N Engl J Med 2004;351:1306–13. [DOI] [PubMed] [Google Scholar]
- 31. Brunette MG, Lands L, Thibodeau LP. Childhood asthma: prevention of attacks with short-term corticosteroid treatment of upper respiratory tract infection. Pediatrics 1988;81:624–9. [PubMed] [Google Scholar]
- 32. Buckingham SC, Jafri HS, Bush AJ, et al. . A randomized, double-blind, placebo-controlled trial of dexamethasone in severe respiratory syncytial virus (RSV) infection: effects on RSV quantity and clinical outcome. J Infect Dis 2002;185:1222–8. 10.1086/340024 [DOI] [PubMed] [Google Scholar]
- 33. Bülow SM, Nir M, Levin E, et al. . Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics 1999;104:e77 10.1542/peds.104.6.e77 [DOI] [PubMed] [Google Scholar]
- 34. Chang AB, Clark R, Sloots TP, et al. . A 5- versus 3-day course of oral corticosteroids for children with asthma exacerbations who are not hospitalised: a randomised controlled trial. Med J Aust 2008;189:306–10. [DOI] [PubMed] [Google Scholar]
- 35. Chen ZG, Li M, Chen H, et al. . [Efficacy of pulmicort suspension plus salbutamol and ipratropium bromide for management of acute asthma exacerbation in children: a comparative study]. Nan Fang Yi Ke Da Xue Xue Bao 2008;28:470–2. [PubMed] [Google Scholar]
- 36. Chub-Uppakarn S, Sangsupawanich P. A randomized comparison of dexamethasone 0.15 mg/kg versus 0.6 mg/kg for the treatment of moderate to severe croup. Int J Pediatr Otorhinolaryngol 2007;71:473–7. 10.1016/j.ijporl.2006.11.016 [DOI] [PubMed] [Google Scholar]
- 37. Clavenna A, Sequi M, Cartabia M, et al. . Effectiveness of nebulized beclomethasone in preventing viral wheezing: an RCT. Pediatrics 2014;133:e505–12. 10.1542/peds.2013-2404 [DOI] [PubMed] [Google Scholar]
- 38. Connett GJ, Warde C, Wooler E, et al. . Prednisolone and salbutamol in the hospital treatment of acute asthma. Arch Dis Child 1994;70:170–3. 10.1136/adc.70.3.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Connolly JH, Field CM, Glasgow JF, et al. . A double blind trial of prednisolone in epidemic bronchiolitis due to respiratory syncytial virus. Acta Paediatr Scand 1969;58:116–20. 10.1111/j.1651-2227.1969.tb04693.x [DOI] [PubMed] [Google Scholar]
- 40. Corneli HM, Zorc JJ, Mahajan P, et al. . A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med 2007;357:331–9. 10.1056/NEJMoa071255 [DOI] [PubMed] [Google Scholar]
- 41. Cronin JJ, McCoy S, Kennedy U, et al. . A randomized trial of single-dose oral dexamethasone versus multidose prednisolone for acute exacerbations of asthma in children who attend the emergency department. Ann Emerg Med 2016;67:593–601. 10.1016/j.annemergmed.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 42. Csonka P, Kaila M, Laippala P, et al. . Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection-induced lower airway disease: a randomized, placebo-controlled trial. J Pediatr 2003;143:725–30. 10.1067/S0022-3476(03)00498-0 [DOI] [PubMed] [Google Scholar]
- 43. Daugbjerg P, Brenøe E, Forchhammer H, et al. . A comparison between nebulized terbutaline, nebulized corticosteroid and systemic corticosteroid for acute wheezing in children up to 18 months of age. Acta Paediatr 1993;82:547–51. 10.1111/j.1651-2227.1993.tb12750.x [DOI] [PubMed] [Google Scholar]
- 44. Dawson KP, Sharpe C. A comparison of the acceptability of prednisolone tablets and prednisolone sodium phosphate solution in childhood acute asthma. Aust J Hosp Pharm 1993;23:320–3. [Google Scholar]
- 45. Ducharme FM, Lemire C, Noya FJ, et al. . Preemptive use of high-dose fluticasone for virus-induced wheezing in young children. N Engl J Med 2009;360:339–53. 10.1056/NEJMoa0808907 [DOI] [PubMed] [Google Scholar]
- 46. Eboriadou M, Chryssanthopoulou D, Stamoulis P, et al. . The effectiveness of local corticosteroids therapy in the management of mild to moderate viral croup. Minerva Pediatr 2010;62:23–8. [PubMed] [Google Scholar]
- 47. Eden AN, Kaufman A, Yu R. Corticosteroids and croup. Controlled double-blind study. JAMA 1967;200:403–4. [PubMed] [Google Scholar]
- 48. Escobedo Chavez E, Garcia Mun̄iz LO, Thompson Chagoyan O, et al. . Steroids and inhalation therapy in the management of acute asthma in children. Current Therapeutic Research 1992;52:7–12. 10.1016/S0011-393X(05)80430-8 [DOI] [Google Scholar]
- 49. Fifoot AA, Ting JY. Comparison between single-dose oral prednisolone and oral dexamethasone in the treatment of croup: a randomized, double-blinded clinical trial. Emerg Med Australas 2007;19:51–8. 10.1111/j.1742-6723.2006.00919.x [DOI] [PubMed] [Google Scholar]
- 50. Fitzgerald D, Mellis C, Johnson M, et al. . Nebulized budesonide is as effective as nebulized adrenaline in moderately severe croup. Pediatrics 1996;97:722–5. [PubMed] [Google Scholar]
- 51. Francis P, Geelhoed G, Harris MA, et al. . Effect of nebulised fluticasone propionate 1 mg twice daily compared with oral prednisolone in pre-school children aged 48 months or less with an acute exacerbation of asthma [abstract]. Eur Respir J 1997(Suppl 25):275s. [Google Scholar]
- 52. Garbutt JMC, Bridget C, Sterkel R, et al. . The comparative effectiveness of prednisolone and dexamethasone for children with croup: A community-based randomized trial. Clin Pediatr 2013;52:1014–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ghirga G, Ghirga P, Fagioli S, et al. . Intermittent treatment with high dose nebulized beclomethasone for recurrent wheezing in infants due to upper respiratory tract infection. Minerva Pediatr 2002;54:217–20. [PubMed] [Google Scholar]
- 54. Gill N, Sirizzotti N, Johnson D, et al. . Endogenous glucocorticoid response to single-dose dexamethasone for croup in children: a pharmacodynamic study. Pediatr Emerg Care 2017;11:1 10.1097/PEC.0000000000001142 [DOI] [PubMed] [Google Scholar]
- 55. Goebel J, Estrada B, Quinonez J, et al. . Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr 2000;39:213–20. 10.1177/000992280003900404 [DOI] [PubMed] [Google Scholar]
- 56. Grant CC, Duggan AK, Santosham M, et al. . Oral prednisone as a risk factor for infections in children with asthma. Arch Pediatr Adolesc Med 1996;150:58–63. 10.1001/archpedi.1996.02170260062010 [DOI] [PubMed] [Google Scholar]
- 57. Gries DM, Moffitt DR, Pulos E, et al. . A single dose of intramuscularly administered dexamethasone acetate is as effective as oral prednisone to treat asthma exacerbations in young children. J Pediatr 2000;136:298–303. 10.1067/mpd.2000.103353 [DOI] [PubMed] [Google Scholar]
- 58. Hedlin G, Svedmyr J, Ryden AC. Systemic effects of a short course of betamethasone compared with high-dose inhaled budesonide in early childhood asthma. Acta Paediatr 1999;88:48–51. 10.1111/j.1651-2227.1999.tb01267.x [DOI] [PubMed] [Google Scholar]
- 59. Husby S, Agertoft L, Mortensen S, et al. . Treatment of croup with nebulised steroid (budesonide): a double blind, placebo controlled study. Arch Dis Child 1993;68:352–5. 10.1136/adc.68.3.352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Inglis AF. Herpes simplex virus infection. A rare cause of prolonged croup. Arch Otolaryngol Head Neck Surg 1993;119:551–2. 10.1001/archotol.1993.01880170075016 [DOI] [PubMed] [Google Scholar]
- 61. Jan JS, Wu WF. Acute effect of glucocorticoid treatment on serum osteocalcin levels in asthmatic children. J Microbiol Immunol Infect 2000;33:25–8. [PubMed] [Google Scholar]
- 62. Jartti T, Nieminen R, Vuorinen T, et al. . Short- and long-term efficacy of prednisolone for first acute rhinovirus-induced wheezing episode. J Allergy Clin Immunol 2015;135:691–8. 10.1016/j.jaci.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jartti T, Lehtinen P, Vanto T, et al. . Evaluation of the efficacy of prednisolone in early wheezing induced by rhinovirus or respiratory syncytial virus. Pediatr Infect Dis J 2006;25:482–8. 10.1097/01.inf.0000215226.69696.0c [DOI] [PubMed] [Google Scholar]
- 64. Jartti T, Lehtinen P, Vanto T, et al. . Efficacy of prednisolone in children hospitalized for recurrent wheezing. Pediatr Allergy Immunol 2007;18:326–34. 10.1111/j.1399-3038.2007.00512.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Johnson DW, Jacobson S, Edney PC, et al. . A comparison of nebulized budesonide, intramuscular dexamethasone, and placebo for moderately severe croup. N Engl J Med 1998;339:498–503. 10.1056/NEJM199808203390802 [DOI] [PubMed] [Google Scholar]
- 66. Johnson DW, Schuh S, Koren G, et al. . Outpatient treatment of croup with nebulized dexamethasone. Arch Pediatr Adolesc Med 1996;150:349–55. 10.1001/archpedi.1996.02170290015002 [DOI] [PubMed] [Google Scholar]
- 67. Klassen TP, Craig WR, Moher D, et al. . Nebulized budesonide and oral dexamethasone for treatment of croup: a randomized controlled trial. JAMA 1998;279:1629–32. 10.1001/jama.279.20.1629 [DOI] [PubMed] [Google Scholar]
- 68. Klassen TP, Feldman ME, Watters LK, et al. . Nebulized budesonide for children with mild-to-moderate croup. N Engl J Med 1994;331:285–9. 10.1056/NEJM199408043310501 [DOI] [PubMed] [Google Scholar]
- 69. Klassen TP, Watters LK, Feldman ME, et al. . The efficacy of nebulized budesonide in dexamethasone-treated outpatients with croup. Pediatrics 1996;97:463–6. [PubMed] [Google Scholar]
- 70. Kuyucu S, Unal S, Kuyucu N, et al. . Additive effects of dexamethasone in nebulized salbutamol or L-epinephrine treated infants with acute bronchiolitis. Pediatr Int 2004;46:539–44. 10.1111/j.1442-200x.2004.01944.x [DOI] [PubMed] [Google Scholar]
- 71. Lai ST, Hua YM, Lai YS, et al. . Comparison of nebulized budesonide with intravenous dexamethasone in the treatment of young children hospitalized with acute asthma. J Med Sci 2005;25:223–8. [Google Scholar]
- 72. Langton Hewer S, Hobbs J, Reid F, et al. . Prednisolone in acute childhood asthma: clinical responses to three dosages. Respir Med 1998;92:541–6. 10.1016/S0954-6111(98)90305-5 [DOI] [PubMed] [Google Scholar]
- 73. Lee KM, Lin YZ, Huang FY. Steroid-induced acute psychosis in a child with asthma: report of one case. Acta Paediatr Taiwan 2001;42:169–71. [PubMed] [Google Scholar]
- 74. Leer JA, Green JL, Heimlich EM, et al. . A controlled, collaborative study in 297 infants and children. Am J Dis Child 1969;117:495–503. [PubMed] [Google Scholar]
- 75. Lehmann S, Ott H. Glucocorticoid hypersensitivity as a rare but potentially fatal side effect of paediatric asthma treatment: a case report. J Med Case Rep 2008;2:186 10.1186/1752-1947-2-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Leipzig B, Oski FA, Cummings CW, et al. . A prospective randomized study to determine the efficacy of steroids in treatment of croup. J Pediatr 1979;94:194–6. 10.1016/S0022-3476(79)80821-5 [DOI] [PubMed] [Google Scholar]
- 77. Lin YZ, Hsieh KH, Chen W, et al. . Clinical trial of corticosteroid and beta-2 bronchodilator in acute wheezing infants. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1991;32:333–40. [PubMed] [Google Scholar]
- 78. Lucas-Bouwman ME, Roorda RJ, Jansman FG, et al. . Crushed prednisolone tablets or oral solution for acute asthma? Arch Dis Child 2001;84:347–8. 10.1136/adc.84.4.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nahum A, Garty BZ, Marcus N, et al. . Severe hypersensitivity reactions to corticosteroids in children. Pediatr Emerg Care 2009;25:339–41. 10.1097/PEC.0b013e3181a34901 [DOI] [PubMed] [Google Scholar]
- 80. Paniagua N, Munoz N, Lopez R, et al. . Randomized trial of two doses of oral dexamethasone versus prednisone/prednisolone for children with acute asthma exacerbations in pediatric emergency department. Eur J Pediatr Conference: 6th Congress of the European Academy of Paediatric Societies Switzerland 2016;175:1480. [Google Scholar]
- 81. Panickar J, Lakhanpaul M, Lambert PC, et al. . Oral prednisolone for preschool children with acute virus-induced wheezing. N Engl J Med 2009;360:329–38. 10.1056/NEJMoa0804897 [DOI] [PubMed] [Google Scholar]
- 82. Panigada S, Sacco O, Girosi D, et al. . Corticosteroids may favor proliferation of thoracic inflammatory myofibroblastic tumors. Pediatr Pulmonol 2014;49:E109–E111. 10.1002/ppul.22977 [DOI] [PubMed] [Google Scholar]
- 83. Plint AC, Johnson DW, Patel H, et al. . Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med 2009;360:2079–89. 10.1056/NEJMoa0900544 [DOI] [PubMed] [Google Scholar]
- 84. Razi CH, Akelma AZ, Harmanci K, et al. . The addition of inhaled budesonide to standard therapy shortens the length of stay in hospital for asthmatic preschool children: a randomized, double-blind, placebo-controlled trial. Int Arch Allergy Immunol 2015;166:297–303. 10.1159/000430443 [DOI] [PubMed] [Google Scholar]
- 85. Roberts GW, Master VV, Staugas RE, et al. . Repeated dose inhaled budesonide versus placebo in the treatment of croup. J Paediatr Child Health 1999;35:170–4. 10.1046/j.1440-1754.1999.t01-1-00335.x [DOI] [PubMed] [Google Scholar]
- 86. Roorda RJ, Walhof CM. Effects of inhaled fluticasone propionate administered with metered dose inhaler and spacer in mild to moderate croup: a negative preliminary report. Pediatr Pulmonol 1998;25:114–7. [DOI] [PubMed] [Google Scholar]
- 87. Roosevelt G, Sheehan K, Grupp-Phelan J, et al. . Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet 1996;348:292–5. 10.1016/S0140-6736(96)02285-4 [DOI] [PubMed] [Google Scholar]
- 88. Sadowitz PD, Page NE, Crowley K. Adverse effects of steroid therapy in children with pharyngitis with unsuspected malignancy. Pediatr Emerg Care 2012;28:807–9. 10.1097/PEC.0b013e31826288e5 [DOI] [PubMed] [Google Scholar]
- 89. Saito M, Kikuchi Y, Kawarai Lefor A, et al. . High-dose nebulized budesonide is effective for mild asthma exacerbations in children under 3 years of age. Eur Ann Allergy Clin Immunol 2017;49:22–7. [PubMed] [Google Scholar]
- 90. Schuh S, Coates AL, Dick P, et al. . A single versus multiple doses of dexamethasone in infants wheezing for the first time. Pediatr Pulmonol 2008;43:844–50. 10.1002/ppul.20845 [DOI] [PubMed] [Google Scholar]
- 91. Schuh S, Willan AR, Stephens D, et al. . Can montelukast shorten prednisolone therapy in children with mild to moderate acute asthma? A randomized controlled trial. J Pediatr 2009;155:795–800. 10.1016/j.jpeds.2009.06.008 [DOI] [PubMed] [Google Scholar]
- 92. Siomou E, Challa A, Tzoufi M, et al. . Biochemical markers of bone metabolism in infants and children under intravenous corticosteroid therapy. Calcif Tissue Int 2003;73:319–25. 10.1007/s00223-002-2099-x [DOI] [PubMed] [Google Scholar]
- 93. Sparrow A, Geelhoed G. Prednisolone versus dexamethasone in croup: a randomised equivalence trial. Arch Dis Child 2006;91:580–3. 10.1136/adc.2005.089516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Stafford L, Hope ME, Janney EP, et al. . Comparison of paediatric steroid mixtures. The Australian Journal of Hospital Pharmacy 1998;28:246–9. 10.1002/jppr1998284246 [DOI] [Google Scholar]
- 95. Storr J, Barrell E, Barry W, et al. . Effect of a single oral dose of prednisolone in acute childhood asthma. Lancet 1987;1:879–82. 10.1016/S0140-6736(87)92857-1 [DOI] [PubMed] [Google Scholar]
- 96. Sumboonnanonda A, Suwanjutha S, Sirinavin S. Randomized controlled trial of dexamethasone in infectious croup. J Med Assoc Thai 1997;80:262–5. [PubMed] [Google Scholar]
- 97. Sung L, Osmond MH, Klassen TP. Randomized, controlled trial of inhaled budesonide as an adjunct to oral prednisone in acute asthma. Acad Emerg Med 1998;5:209–13. 10.1111/j.1553-2712.1998.tb02614.x [DOI] [PubMed] [Google Scholar]
- 98. Super DM, Cartelli NA, Brooks LJ, et al. . A prospective randomized double-blind study to evaluate the effect of dexamethasone in acute laryngotracheitis. J Pediatr 1989;115:323–9. 10.1016/S0022-3476(89)80095-2 [DOI] [PubMed] [Google Scholar]
- 99. Sussman S, Grossman M, Magoffin R, et al. . Dexamethasone (16-alpha-methyl, 9-alpha-fluoroprednisolone) in obstructive respiratory tract infections in children. a controlled study. Pediatrics 1964;34:851–5. [PubMed] [Google Scholar]
- 100. Svedmyr J, Nyberg E, Asbrink-Nilsson E, et al. . Intermittent treatment with inhaled steroids for deterioration of asthma due to upper respiratory tract infections. Acta Paediatr 1995;84:884–8. 10.1111/j.1651-2227.1995.tb13786.x [DOI] [PubMed] [Google Scholar]
- 101. Svedmyr J, Nyberg E, Thunqvist P, et al. . Prophylactic intermittent treatment with inhaled corticosteroids of asthma exacerbations due to airway infections in toddlers. Acta Paediatr 1999;88:42–7. 10.1111/j.1651-2227.1999.tb01266.x [DOI] [PubMed] [Google Scholar]
- 102. Tagarro A, Pérez L, Quintero VM, et al. . Dexamethasone does not reduce length of hospitalization or recurrent wheezing 1 year after early bronchiolitis. Minerva Pediatr 2014;66:131–40. [PubMed] [Google Scholar]
- 103. Tal A, Bavilski C, Yohai D, et al. . Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics 1983;71:13–18. [PubMed] [Google Scholar]
- 104. Tamura A, Matsubara K, Tanaka T, et al. . Methylprednisolone pulse therapy for refractory Mycoplasma pneumoniae pneumonia in children. J Infect 2008;57:223–8. 10.1016/j.jinf.2008.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Teeratakulpisarn J, Limwattananon C, Tanupattarachai S, et al. . Efficacy of dexamethasone injection for acute bronchiolitis in hospitalized children: a randomized, double-blind, placebo-controlled trial. Pediatr Pulmonol 2007;42:433–9. 10.1002/ppul.20585 [DOI] [PubMed] [Google Scholar]
- 106. van Woensel JB, Wolfs TF, van Aalderen WM, et al. . Randomised double blind placebo controlled trial of prednisolone in children admitted to hospital with respiratory syncytial virus bronchiolitis. Thorax 1997;52:634–7. 10.1136/thx.52.7.634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Webb MS, Henry RL, Milner AD. Oral corticosteroids for wheezing attacks under 18 months. Arch Dis Child 1986;61:15–19. 10.1136/adc.61.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Zhang L, Ferruzzi E, Bonfanti T, et al. . Long and short-term effect of prednisolone in hospitalized infants with acute bronchiolitis. J Paediatr Child Health 2003;39:548–51. 10.1046/j.1440-1754.2003.00212.x [DOI] [PubMed] [Google Scholar]
- 109. Kelly HW, Van Natta ML, Covar RA, et al. . Effect of long-term corticosteroid use on bone mineral density in children: a prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) study. Pediatrics 2008;122:e53–e61. 10.1542/peds.2007-3381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Fuhlbrigge AL, Kelly HW. Inhaled corticosteroids in children: effects on bone mineral density and growth. Lancet Respir Med 2014;2:487–96. 10.1016/S2213-2600(14)70024-4 [DOI] [PubMed] [Google Scholar]
- 111. Aljebab F, Choonara I, Conroy S. Systematic Review of the Toxicity of Long-Course Oral Corticosteroids in Children. PLoS One 2017;12:e0170259 10.1371/journal.pone.0170259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Vatti RR, Ali F, Teuber S, et al. . Hypersensitivity reactions to corticosteroids. Clin Rev Allergy Immunol 2014;47:26–37. 10.1007/s12016-013-8365-z [DOI] [PubMed] [Google Scholar]
- 113. Rieder M. Size and taste matters: recent progress in the development of age-appropriate medicines for children. Pharmaceut Med 2018;32:21–30. 10.1007/s40290-017-0218-2 [DOI] [Google Scholar]
- 114. Beigelman A, Durrani S, Guilbert TW. Should a preschool child with acute episodic wheeze be treated with oral corticosteroids? A Pro/Con Debate. J Allergy Clin Immunol Pract 2016;4:27–35. 10.1016/j.jaip.2015.10.017 [DOI] [PubMed] [Google Scholar]
- 115. Aljebab F, Choonara I, Conroy S. Systematic review of the toxicity of short-course oral corticosteroids in children. Arch Dis Child 2016;101:365–70. 10.1136/archdischild-2015-309522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Waljee AK, Rogers MA, Lin P, et al. . Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ 2017;357:j1415 10.1136/bmj.j1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Hartling L, Ali S, Dryden DM, et al. . How safe are common analgesics for the treatment of acute pain for children? a systematic review. Pain Res Manag 2016;2016:1–15. 10.1155/2016/5346819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Guyatt GH, Oxman AD, Vist GE, et al. . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-028511supp001.pdf (123.9KB, pdf)
bmjopen-2018-028511supp002.pdf (111.6KB, pdf)
bmjopen-2018-028511supp003.pdf (411.9KB, pdf)
bmjopen-2018-028511supp004.pdf (159.9KB, pdf)
bmjopen-2018-028511supp005.pdf (217.8KB, pdf)
bmjopen-2018-028511supp006.pdf (1.5MB, pdf)
bmjopen-2018-028511supp007.pdf (88.1KB, pdf)