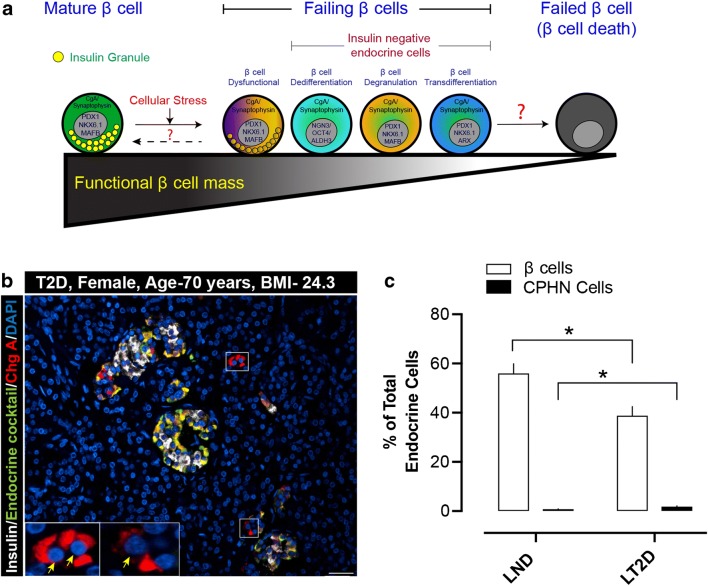
Fig. 1.
a A schematic illustrating the possible “altered differentiation” states of human pancreatic β cells. In response to cellular stresses (glucotoxicity, ER stress, immune attack or viral infection), β cells can undergo functional or morphological changes. These alterations might include insulin-positive dysfunctional β cells or insulin-negative β cells that are dedifferentiated (expressing transcription factors of endocrine progenitor cells), degranulated (“empty” β cells no longer harboring a normal complement of insulin granules), or transdifferentiated (transitioning towards a different endocrine cell subtype). At this stage, the β cells may be recognized as “failing β cells,” as they do not contain any releasable insulin. The unanswered questions are whether human β cells from those transition states can revert back towards the mature, fully functional state, or whether they will eventually fail completely and undergo apoptotic death. b Example of chromograninA-positive hormone-negative (CPHN) cells in the pancreas of a lean subject with type 2 diabetes (Age, 70 years, BMI, 24.3). The merged immunofluorescent image is a selected field of 4-μm paraffin section of pancreas stained for insulin (white), endocrine cocktail (glucagon, somatostatin, pancreatic polypeptide and ghrelin) (green), chromograninA (ChgA) (red), and DAPI (blue). The cells staining only for chromograninA and not for any of the known pancreatic hormones (CPHN cells) are therefore stained red (and indicated by yellow arrows). Inset, high-power image of the selected area (marked by white square in the low power image) indicating the CPHN cells. Scale bar, 50 μm. c Percent of β cells and CPHN cells (of total endocrine cells) in lean human subjects with no diabetes (LND) and lean human subjects with type 2 diabetes (LT2D). Data are presented as mean ± SEM, N = 10 (each group). *, p < 0.01