Case Presentation
A 65-year-old male with past medical history of hypertension, hyperlipidemia, diabetes mellitus type 2 and adrenal cortical carcinoma presented to a local hospital for symptomatic anemia requiring multiple transfusions. After stabilization and discharge, the patient was referred to our institution for further evaluation and management of a suspected gastrointestinal stromal tumor (GIST). The patient reported 6 months of early satiety and worsening dyspepsia refractory to proton pump inhibitor therapy. Abdominal computed tomography (CT) showed a 5.0 cm mass in the stomach (Fig. 1A–B). He underwent esophagogastroduodenoscopy (EGD) and endoscopic ultrasound (EUS) revealing a 5.0 × 2.3 cm poorly defined, bilobar hypoechoic mass in the gastric antrum that arose from the muscularis propria (Fig. 1C–D). Immunohistochemistry (IHC) of the core needle biopsy revealed strongly positive staining for smooth muscle actin (SMA), weakly positive staining with CD117 (c-KIT) and patchy staining of Discovered on GIST-1 (DOG-1). The staining pattern was ambiguous between myxoid GIST and plexiform fibromyxoma. Shortly thereafter, the patient presented to the emergency room with hematemesis and anemia. After resuscitation including multiple units of packed red blood cells, ongoing bleeding was seen on upper endoscopy and the patient elected to undergo surgical treatment. Open gastric wedge resection was performed. The exophytic mass was removed from the lesser curve of the stomach and the defect was closed in a primary hand-sewn fashion (Fig. 1E–F). Final gross examination revealed a 5.0-cm smooth, pink, lobular mass and histopathology demonstrated a transmural myxoid bland spindle cell lesion with prominent thin capillaries (Fig. 2A–B). The mass had luminal ulceration and infiltrated the mucosa, submucosa and muscularis propria. Final IHC stains where positive for SMA and negative for S-100, MUC-4, CD117 and DOG-1 (Fig. 2C–D). Pathology was most consistent with plexiform fibromyxoma, and not a GIST.
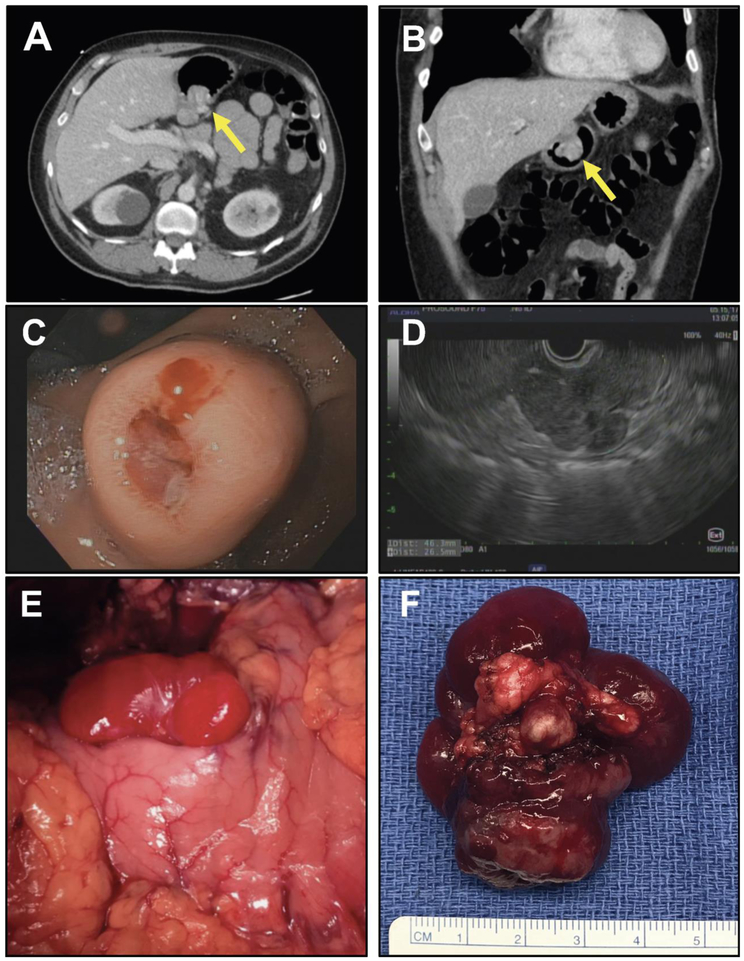
Figure 1:
65-year old male with upper gastrointestinal symptoms. (a-b) Abdominal computed tomography with 5.0-cm endophytic gastric mass. (c) Upper endoscopy shows an endophytic mass within gastric antrum with luminal ulceration. (d) Endoscopic ultrasound demonstrates submucosal location of tumor. (e) In situ location of tumor along lesser curvature of gastric antrum. (f) Explanted specimen following resection.
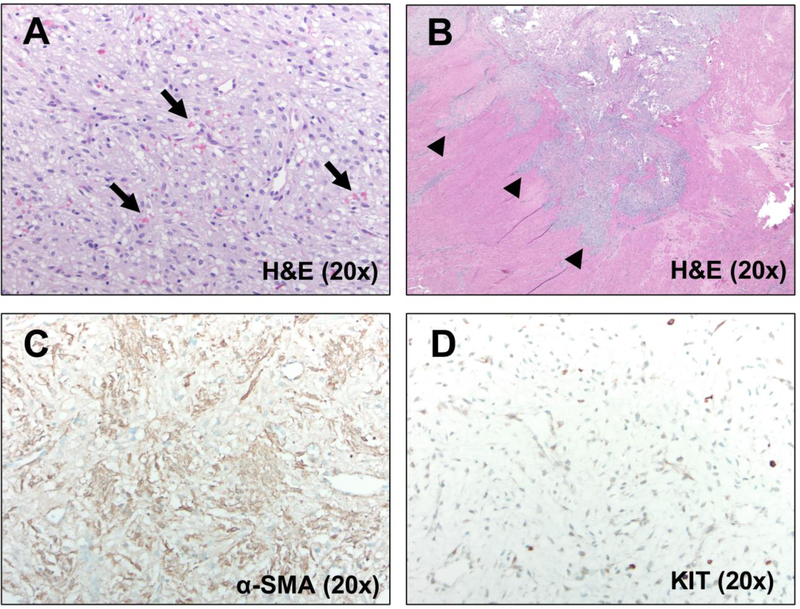
Figure 2:
Histopathologic analysis consistent with plexiform fibromyxoma. (a) Hemotoxylin and eosin (H&E) staining showing myxoid bland spindle cells and prominent thin capillaries, as well as (b) invasion of the submucosa and muscularis propria. Photomicrographs of (c) α-SMA and (d) c-KIT on immunohistochemical (IHC) staining.
Discussion
Plexiform fibromyxoma is a benign neoplasm of gastrointestinal tract with fewer than 80 cases reported in the literature. There are several noticeable characteristics of this neoplasm which include originating from the submucosal layer and gastric fundus predominance. Radiologically and endoscopically, this tumor lacks distinguishing features from other submucosal tumors such as GIST, leiomyoma, schwannoma, desmoid fibromatosis and others. However, based upon the current case, as well as review of other reported images in the literature, the serosal side of the tumor has a uniquely smooth, pink, and lobular appearance that is quite distinct from the fleshier, tan-brown, course appearance of GIST.1 Ultimately, the final diagnosis is confirmed with both microscopic examination and immunohistochemistry. The most common positive immunostains are SMA, vimentin and mixed results with CD10, desmin, calponin and caldesmon.2 The clinical presentation is usually upper gastrointestinal bleeding with symptoms varying from melena, hematemesis, epigastric pain and the most common being symptomatic anemia. Other less frequent presenting symptoms include gastric outlet obstruction and weight loss. The treatment of choice is surgical resection, although there have been reports of endoscopic resection. Ultimately, the surgical technique is dependent on the size and location of the tumor. Most studies in the literature report treatment by distal gastrectomy. Other techniques such as partial gastrectomy, wedge resection, antrectomy and subtotal gastrectomy have also been reported.3 Despite a hemorrhagic diathesis, PF is considered a benign disease with no reports of either malignant transformation or metastatic spread. In conclusion, we now report that not only histological, but also gross tumor appearance of a rose-colored tumor may distinguish plexiform fibromyxoma from GIST. Further series are needed to better understand the underlying cell of origin and risk factors for developing this rare tumor type.
Financial Support:
This work was supported by the Society for Surgery of the Alimentary Tract (SSAT) Mentored Research Award (S.B), UC San Diego GIST Research Fund (J.K.S.), NIH K08CA168999 (J.K.S.) and NIH R21CA192072 (J.K.S.).
Authors’ Disclosures: Jason Sicklick receives research funds from Foundation Medicine Inc. Amgen Pharmaceuticals and Novartis Pharmaceuticals, as well as consultant fees from Loxo, Biotheranostics, and Grand Rounds. All other authors have no relationships to disclose.
Footnotes
Conflict of Interest
J.K.S. has research funding from Novartis Pharmaceuticals, Amgen Pharmaceuticals and Foundation Medicine. J.K.S. also serves or served as Consultant to the following organizations: Grand Rounds (2015–18), and Loxo Oncology (2017–18). These disclosures had no impact on any of the work presented in this manuscript. No other authors have any conflict of interests to declare.
References:
- 1.Szurian K et al. Rarity among benign gastric tumors: Plexiform fibromyxoma - Report of two cases. World journal of gastroenterology 23, 5817–5822, doi: 10.3748/wjg.v23.i31.5817 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miettinen M, Makhlouf HR, Sobin LH & Lasota J Plexiform Fibromyxoma: A Distinctive Benign Gastric Antral Neoplasm Not to be Confused With a Myxoid Gist. The American journal of surgical pathology 33, 1624–1632, doi: 10.1097/PAS.0B013E3181AE666A (2009). [DOI] [PubMed] [Google Scholar]
- 3.Morris MW, Sullivan L, Sawaya DE, Steiner MA & Nowicki MJ Gastric plexiform fibromyxoma tumor in a child – Case report and review of the literature. Journal of Pediatric Surgery Case Reports Volume 4, Pages 38–41 (2016). [Google Scholar]