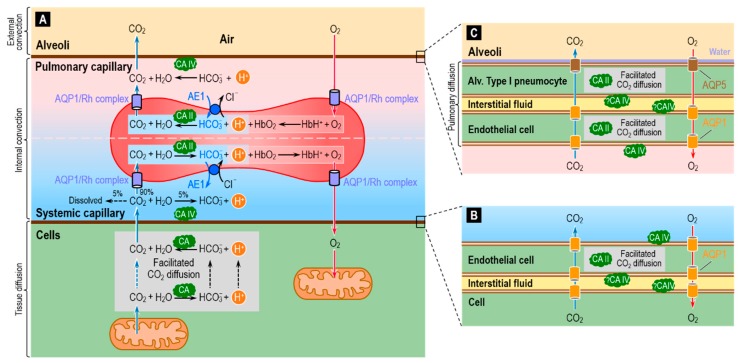
Figure 9.
Diagram of the reaction, diffusion and transport processes involved in the removal of the metabolically produced CO2 from cells to blood (systemic capillary) and from blood (pulmonary capillary) to the lung (alveoli). (A) Of the CO2 that diffuses from cells to the systemic capillary, ~10% remains in the blood plasma—as dissolved CO2 (~5%), HCO3− (~5%) or carbamino compounds (<1%)—whereas ~90% enters the RBCs, almost entirely via the water channel AQP1 [104] or the Rh complex [72]. In the cytosol of the RBCs, most CO2 rapidly combines with H2O to form HCO3− and H+, under the catalytic action of CA I (not shown) and CA II. Much of this newly formed HCO3− exits via the Cl-HCO3 exchanger AE1 [105,106]. A smaller fraction of the incoming CO2 covalently reacts with hemoglobin (Hb) to form carbamino-Hb and H+, and a tiny fraction remains dissolved in the RBC cytosol. Hb buffers nearly all of the newly formed H+ [58,107]. These events all reverse in the pulmonary capillary, where RBCs unload CO2 for diffusion into the alveolar space. Another important function of CA in RBCs is augmentation of the association and dissociation of O2 with Hb via the Bohr effect. In the systemic capillary, the entry of CO2 into RBCs causes their pH to decrease, thereby reducing the Hb-O2 binding affinity and favoring O2 unloading to the tissue. The formation of carbamino-Hb also favors O2 unloading. In the pulmonary capillary, the exit of CO2 from the RBCs has the opposite effect, favoring O2 loading from the alveoli to the pulmonary capillary. Recent evidence points toward a role of AQP1 and the Rh complex in the diffusion of O2 across the RBC membrane [108]. CA IV on the lumen side of the capillary endothelial cells may accelerate the reaction CO2 + H2O → HCO3− + H+ in the lumen of systemic capillaries, thereby maximizing flux from tissue to blood, and may accelerate the opposite reaction HCO3− + H+ → CO2 + H2O in the lumen of pulmonary capillaries, thereby maximizing CO2 flux from blood to alveoli (see Figure 3B). (B) Magnification of the different layers of the gas-exchange surface at the systemic capillary. The barrier between the RBC cytosol and capillary lumen actually consists of three plasma membranes—that of the cell that generates the CO2, and the two membranes of the endothelial cell—plus the interstitial fluid and cytosol of the endothelial cell. Cytosolic CA would facilitate CO2 diffusion through the endothelial cell (see Figure 1) and enhance diffusion across the membranes (see Figure 3B). CA IV may be present on the membranes facing the extremely thin layer of interstitial fluid, where this enzyme could also facilitate CO2 diffusion through the interstitial fluid as well as the transmembrane diffusion of CO2. Note that AQP1 or other AQPs—depending on the identity of the capillary bed—could provide a low-resistance pathway for the diffusion of CO2 and O2 across all three of these membranes. (C) Magnification of the different layers of the pulmonary capillary-alveolar gas exchange surface. This system is more complex than that in (B) because the gases must cross four cells membranes. In addition, AQP5 is present at very high densities in the alveolar side of the alveolar type I pneumocyte [109].