Abstract
Background:
Ulnar collateral ligament (UCL) reconstruction of the elbow is commonly performed on professional baseball pitchers. Recent reports have suggested that revision rates are on the rise and may be higher than previously thought.
Purpose:
To provide a comprehensive report on current trends, surgical techniques, and outcomes of revision UCL reconstructions performed on professional baseball pitchers between 2010 and 2016.
Study Design:
Case series; Level of evidence, 4.
Methods:
The Major League Baseball Health and Injury Tracking System (HITS) was used to compile records of all revision UCL reconstructions performed on professional baseball pitchers between 2010 and 2016. Player data and outcomes were obtained from HITS, and surgical details were obtained from operative reports. Descriptive statistical analysis was performed on epidemiologic data. Outcomes (return to play [RTP] rates, RTP times, subsequent injuries, and subsequent surgeries) were compared across the most common surgical techniques (docking vs modified Jobe) and graft sources (palmaris longus autograft vs hamstring autograft).
Results:
A total of 69 professional baseball pitchers underwent revision UCL reconstruction from 2010 to 2016 at an average of 1424 days (47 months) after their primary surgery. A trend was seen toward increasing numbers of revision surgeries over time (R2 = 0.441; P = .104). The most commonly used tunnel configuration was the modified Jobe technique (n = 41; 59.4%), and the most commonly used graft was hamstring autograft (n = 34; 49.3%). A majority (76.6%) of pitchers achieved RTP, and 55.3% were able to return to the same level of play. Mean time to RTP was 436 days (14.5 months) for players with a palmaris longus autograft versus 540 days (18 months) for those with a hamstring autograft (P = .108). Further, the mean time to RTP was 423 days (14 months) for the docking technique versus 519 days (17 months) for the modified Jobe technique (P = .296). Similar rates of subsequent injuries and surgeries were noted between the 2 revision techniques and 2 most commonly used graft constructs.
Conclusion:
Revision UCL reconstruction showed relatively high RTP rates (77%), but only 55% of players returned to their same level of play. Mean time to RTP was shorter than that found in other, smaller investigations. Although general trends were seen toward decreased time to RTP for the docking technique and palmaris longus autograft, these differences did not reach statistical significance.
Keywords: ulnar collateral ligament reconstruction, revision, Tommy John surgery, return to play, professional baseball
Surgical reconstruction of the medial ulnar collateral ligament (UCL) of the elbow, colloquially referred to as “Tommy John surgery,” has become more prevalent over the past 2 decades among professional baseball pitchers.4,20,30,31 An estimated 25% of Major League Baseball (MLB) pitchers and 15% of Minor League Baseball (MiLB) pitchers report having previously undergone the procedure.5 Although it is well established that the incidence of primary UCL reconstruction is rising, recent epidemiologic data have shown that revision rates may be increasing at a rate that outpaces primary procedures.7,21 Although these increasing rates are well documented at the professional level (MLB and MiLB), even more concerning is that the greatest increase in surgical rates has been observed in adolescent and teenage players.12,15 As pitchers are starting to undergo primary UCL surgery at younger ages, concern has arisen that many will be more likely to require revision surgery at an earlier age as well.
Sustained rates of return to play (RTP) among MLB pitchers who have undergone revision UCL reconstruction range from 42.3% to 78.0%,17,21,24,25 and the average time to RTP after revision UCL reconstruction ranges from 18.9 to 20.76 months.17,21 A number of studies have shown that revision UCL reconstruction results in decreased RTP rates and shortened careers following return, compared with primary reconstruction.6,17,21,25 Although player performance metrics for both primary and revision UCL reconstruction have been shown to decline following surgery,17,21,24 more robust outcomes and performance data are needed for players undergoing revision surgery.
For primary UCL reconstructions, 2 commonly used techniques are the docking technique and the modified Jobe technique.29 The most commonly used grafts are either the palmaris longus tendon or one of the hamstring tendons (gracilis vs semitendinosus).2,18,19,29 However, no consensus is available regarding optimal surgical technique, graft selection, tunnel configuration, or other surgical variables for revision UCL reconstruction. These data are critical because an improved understanding of the epidemiologic patterns, surgical practices, and outcomes data for revision UCL reconstruction in professional baseball pitchers will help guide clinical practice and optimize results. Accordingly, the purposes of this study were to (1) discuss surgical trends in revision UCL reconstruction among professional baseball pitchers over time, (2) identify the most commonly used surgical techniques in terms of graft type and tunnel configuration for revision surgery, and (3) describe overall outcomes of the procedure and compare them across the most commonly used surgical techniques and graft types.
Methods
The MLB Health and Injury Tracking System (HITS) was accessed to identify all professional baseball (MLB and MiLB) pitchers who were listed as undergoing revision UCL reconstruction between 2010 (the first year HITS was established) and 2016. Nonpitchers were excluded. Player demographics, injury characteristics, surgical details, and player outcomes were analyzed. All data were obtained and analyzed in a completely anonymous and de-identified fashion. Because of the de-identified nature of the data, institutional review board approval was waived by the Mayo Clinic.
Player demographics included age at the time of surgery, throwing side dominance, pitching role (starter vs reliever), date of first professional contract, level of play (MLB vs MiLB), retirement date (if retired prior to 2017), date of primary surgery, and date of revision surgery. Operative reports were reviewed to determine the following surgical details: type of graft used (allograft vs autograft), graft source (eg, palmaris longus, hamstring tendon), tunnel configuration (eg, modified Jobe, docking technique), and concomitant procedures. Concomitant procedures were classified into the following categories: ulnar nerve surgery, debridement of posteromedial impingement (ulnohumeral impingement), flexor-pronator tendon repair, loose body removal, cartilage surgery, treatment of olecranon fractures, and biological augmentation (eg, stem cell injection, platelet-rich plasma).
The following outcomes measures were assessed: RTP status, time to RTP, return to same level (RSL) status, and time to RSL. Players were evaluated over time to see whether they developed subsequent elbow or forearm injuries. For the analysis of subsequent injuries, any elbow or forearm injury that occurred after the player achieved RTP and resulted in at least 1 day out of play was included. The need for subsequent surgery to the elbow (including repeat revision UCL reconstruction and non-UCL reconstruction procedures) or forearm was also assessed. Although all players were included in the analysis of surgical trends, only players with a minimum follow-up of 2 years (ie, surgery between 2010 and 2014) were included in the RTP and outcomes analysis.
Statistical Analysis
General epidemiologic data are reported using standard descriptive statistics such as number, frequency, range, means with standard deviations, and medians. Comparisons were made between groups based on level of play at the time of surgery (MLB vs MiLB), type of graft (palmaris longus autograft vs hamstring autograft), and tunnel configuration (modified Jobe vs docking techniques). The differences in RTP, RSL, subsequent injury, and subsequent injury rates were compared between groups by use of a 2-tailed Fisher exact test. Pairwise comparisons between means were assessed using an unpaired Student t test, and these results are reported with their corresponding mean differences (MDs), 95% CIs, and P values. Linear regression was used to determine the significance of trends over time, and the corresponding R 2 and P values are provided. For all comparisons, P values less than .05 were considered to represent statistical significance.
Results
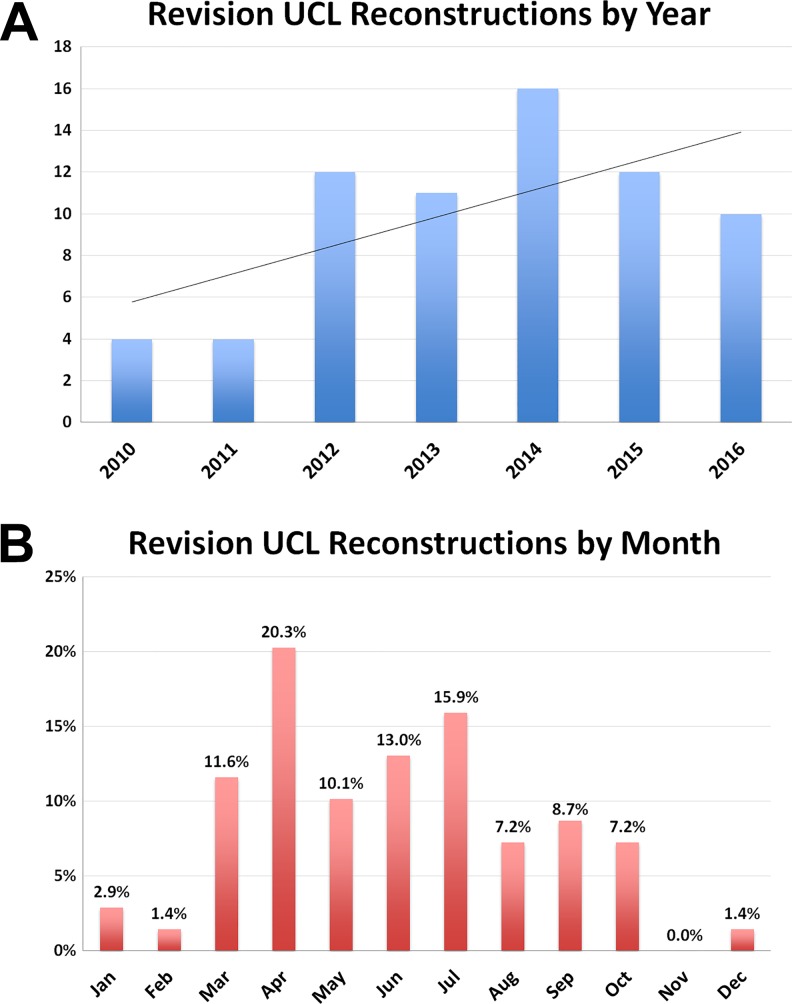
From 2010 to 2016, a total of 69 professional baseball pitchers underwent revision UCL reconstruction at an average of 1424 days (47 months) after their primary surgery. The mean age at the time of revision was 26.3 years (range, 19.5-40.4 years), and 37.7% (n = 26) were MLB pitchers whereas 62.3% (n = 43) were MiLB pitchers. Additional demographic data are listed in Table 1. The greatest number of procedures were performed in 2014 (n = 16), and the fewest were performed in 2010 and 2011 (n = 4 for each) (Figure 1A). Although a general trend was seen toward increasing numbers of revision surgeries over time, this did not reach statistical significance (R 2 = 0.441; P = .104). When case distribution was assessed by month, April (20.3%), July (15.9%), and June (13.0%) were the highest volume months (Figure 1B).
TABLE 1.
Demographics for All Professional Pitchers Undergoing Revision Ulnar Collateral Ligament Reconstruction From 2010 to 2016a
| n | Mean ± SD | Median (Min, Max) |
|
|---|---|---|---|
| Age, y | 69 | 26.3 ± 4.2 | 25.3 (19.5, 40.4) |
| Time from signing to surgery, d | 69 | 2147 ± 1613.0 (70 months) |
1803 (44, 7167) |
| Time from primary to revision, d | 69 | 1424 ± 1184.0 (47 months) |
971 (315, 5665) |
| Postsurgical career length, yb | 32 | 1.7 ± 1.3 | 3 (0, 5) |
| n | % | ||
| Handedness | |||
| Right | 52 | 75.4 | |
| Left | 17 | 24.6 | |
| Primary role | |||
| Starter | 42 | 60.9 | |
| Reliever | 27 | 39.1 | |
| Level at time of surgery | |||
| MLB | 26 | 37.7 | |
| MiLB | 43 | 62.3 | |
| Graft type | |||
| Autograft palmaris longus | 22 | 31.9 | |
| Autograft hamstring tendon | 34 | 49.3 | |
| Unknown or other | 13 | 18.8 | |
| Tunnel configuration | |||
| Docking | 17 | 24.6 | |
| Modified Jobe | 41 | 59.4 | |
| Unknown | 11 | 15.9 |
aMax, maximum; MiLB, Minor League Baseball; Min, minimum; MLB, Major League Baseball.
bOnly players who retired prior to the 2017 season were eligible for postsurgical career length calculations.
Figure 1.
(A) A trend was found toward increasing number of revision ulnar collateral ligament (UCL) surgeries performed over time (R 2 = 0.441; P = .104). (B) The monthly distribution of surgical cases demonstrates that most operations were performed from March to July.
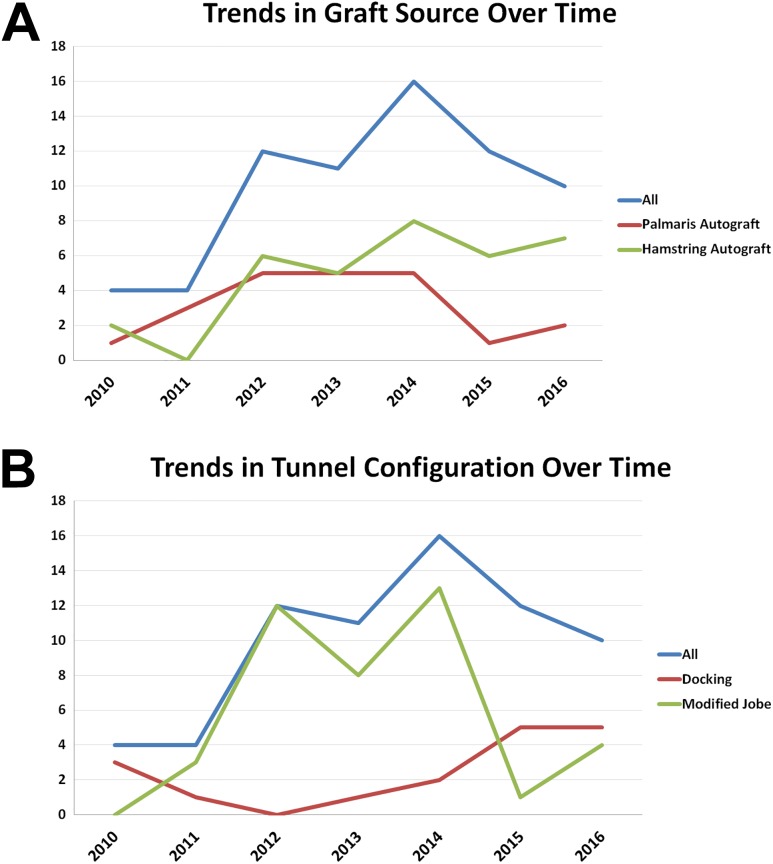
In terms of the surgical procedure, the most common graft sources used were hamstring tendon autograft (n = 34; 49.3%) and palmaris longus autograft (n = 22; 31.9%) (Table 1, Figure 2A). No significant differences were found in the types of grafts used over time (P = .185 for palmaris and P = .175 for hamstring). The majority of cases were performed with the modified Jobe technique (n = 41; 59.4%) or the docking technique (n = 17; 24.6%) (Table 1, Figure 2B), and the frequency of each technique was steady over time (P = .891 and .857, respectively). The 11 remaining cases were performed with an unspecified tunnel configuration. In total, 48 (69.6%) pitchers had at least 1 concomitant procedure at the time of revision UCL reconstruction; 28 (40.6%) had a single concomitant procedure, whereas 13 (18.8%) pitchers had 2 concomitant procedures, and 7 (10.1%) pitchers had 3 concomitant procedures. The most common concomitant procedures were ulnar nerve surgery (n = 36; 52.2%), debridement of posteromedial impingement (n = 15; 21.7%), biological augmentation (n = 15; 21.7%), flexor-pronator tendon repair (n = 7; 10.1%), and loose body removal (n = 2; 2.9%).
Figure 2.
Trends in (A) graft source and (B) tunnel configuration over time for revision ulnar collateral ligament surgery.
In terms of outcomes, 76.6% (n = 36/47) of eligible pitchers undergoing revision UCL reconstruction were able to RTP at any level, and 55.3% (n = 26/47) were able to RSL (Table 2). The mean time to RTP was 484 days (16 months; median, 446.5 days) compared with a mean time to RSL of 518 days (17 months; median, 489.5 days) (MD, 34 days; 95% CI, –36.1 to 104.1 days; P = .336). The frequencies of subsequent injuries and surgeries are listed in Table 2. A comparison of outcomes based on graft type (palmaris vs hamstring) is provided in Table 3. Ultimately, the mean time to RTP was 436 days (14.5 months) for the palmaris group versus 540 days (18 months) for the hamstring group (MD, 103.6 days; 95% CI, –24.3 to 231.5 days; P = .108). No significant differences were found in RTP rates, subsequent injuries, or subsequent surgeries based on graft type (Table 3). Similar results were noted for the comparison between tunnel configurations (Table 4). Mean time to RTP at any level was 423 days (14 months) for the docking technique versus 519 days (17 months) for the modified Jobe technique (MD, 96.6 days; 95% CI, –88.8 to 282.0; P = .296). Similar rates of subsequent injuries and surgeries were noted between the 2 revision techniques (Table 4).
TABLE 2.
Outcomes for the 47 Pitchers Undergoing Revision UCL Reconstruction From 2010 to 2014a
| n | Mean ± SD | Median (Min, Max) |
|
|---|---|---|---|
| Days to return to play | 36 | 484 ± 117.3 | 446.5 (146, 1115) |
| Days to return to play at same level | 26 | 518 ± 158.9 | 489.5 (221, 950) |
| n | % | ||
| Return to play at any level | |||
| Yes | 36 | 76.6 | |
| No | 11 | 23.4 | |
| Return to play at same level | |||
| Yes | 26 | 55.3 | |
| No | 21 | 44.7 | |
| Subsequent elbow injury | |||
| Yes | 14 | 29.8 | |
| No | 33 | 70.2 | |
| Subsequent forearm injury | |||
| Yes | 3 | 6.4 | |
| No | 44 | 93.6 | |
| Subsequent elbow surgery | |||
| Yes | 10 | 21.3 | |
| No | 37 | 78.7 | |
| Repeat revision UCL reconstruction | |||
| Yes | 3 | 6.4 | |
| No | 44 | 93.6 |
aFor all return to play and subsequent injury/surgery calculations, only players undergoing surgery between 2010 and 2014 were included. Max, maximum; Min, minimum; UCL, ulnar collateral ligament.
TABLE 3.
Comparisons of Outcomes Based on Type of Autograft Tendon Used (Autograft Palmaris Longus vs Autograft Hamstring Tendons)a
| n | Mean ± SD | Mean Difference (95% CI) |
P Value | |
|---|---|---|---|---|
| Days to return to play at any level | ||||
| Palmaris longus | 13 | 436 ± 91.5 | 103.6 (–24.3 to 231.5) |
.108 |
| Hamstring | 16 | 540 ± 208.5 | ||
| Days to return to play at same level | ||||
| Palmaris longus | 10 | 510 ± 144.7 | 68.9 (–74.8 to 212.6) |
.328 |
| Hamstring | 11 | 579 ± 167.5 | ||
| Yes, n | No, n | % Yes | P Value | |
| Return to play at any level | ||||
| Palmaris longus | 13 | 6 | 68.4 | .727 |
| Hamstring | 16 | 5 | 76.2 | |
| Return to play at same level | ||||
| Palmaris longus | 10 | 9 | 52.6 | .999 |
| Hamstring | 11 | 10 | 52.4 | |
| Subsequent elbow injury | ||||
| Palmaris longus | 3 | 16 | 15.8 | .163 |
| Hamstring | 8 | 13 | 38.1 | |
| Subsequent forearm injury | ||||
| Palmaris longus | 0 | 19 | 0.0 | .489 |
| Hamstring | 2 | 19 | 9.5 | |
| Subsequent elbow surgery | ||||
| Palmaris longus | 2 | 17 | 10.5 | .241 |
| Hamstring | 6 | 15 | 28.6 | |
| Subsequent UCL reconstruction | ||||
| Palmaris longus | 1 | 18 | 5.3 | .999 |
| Hamstring | 2 | 19 | 9.5 |
aUCL, ulnar collateral ligament.
TABLE 4.
Comparisons of Outcomes Based on Tunnel Configuration (Docking vs Modified Jobe Techniques)a
| n | Mean ± SD | Mean Difference (95% CI) |
P Value | |
|---|---|---|---|---|
| Days to return to play at any level | ||||
| Docking | 4 | 423 ± 54.5 | 96.6 (–88.8 to 282.0) |
.296 |
| Modified Jobe | 28 | 519 ± 178.1 | ||
| Days to return to play at same level | ||||
| Docking | 2 | 476 ± 37.5 | 77.6 (–159.2 to 314.4) |
.502 |
| Modified Jobe | 20 | 553 ± 156.8 | ||
| Yes, n | No, n | % Yes | P Value | |
| Return to play at any level | ||||
| Docking | 4 | 3 | 57.1 | .347 |
| Modified Jobe | 28 | 8 | 77.8 | |
| Return to play at same level | ||||
| Docking | 2 | 5 | 28.6 | .240 |
| Modified Jobe | 20 | 16 | 55.6 | |
| Subsequent elbow injury | ||||
| Docking | 2 | 5 | 28.6 | .999 |
| Modified Jobe | 10 | 26 | 27.8 | |
| Subsequent forearm injury | ||||
| Docking | 0 | 7 | 0.0 | .999 |
| Modified Jobe | 3 | 33 | 8.3 | |
| Subsequent elbow surgery | ||||
| Docking | 1 | 6 | 14.3 | .999 |
| Modified Jobe | 9 | 27 | 25.0 | |
| Subsequent UCL reconstruction | ||||
| Docking | 0 | 7 | 0.0 | .999 |
| Modified Jobe | 3 | 33 | 8.3 |
aUCL, ulnar collateral ligament.
Major league players had a significantly higher rate of RTP (73.1%) compared with minor league players (39.5%) (P = .01). However, no significant difference was found in RSL, time to RTP, or career length between MLB and MiLB players (P value range, .19-.54). Additionally, no significant difference was noted in RTP, RSL, time to RTP, or career length based on player handedness (P value range, .08-.78), role as a starter or relief pitcher (P value range, .62-.92), or player age at the time of surgery (P value range, .06-.94). Finally, the number of concomitant procedures did not significantly affect RTP (P = .19), RSL (P = .85), time to RTP (P = .24), or career length (P = .15).
Discussion
Because the results of revision procedures often differ from those of primary surgeries, epidemiologic and outcome data of revision UCL reconstruction may play a crucial role in patient care. This study demonstrated a trend toward increasing numbers of revision UCL reconstructions between 2010 and 2016 among professional baseball players. During this period, the most commonly used graft was an autograft hamstring tendon, and the majority of procedures were performed with the modified Jobe technique. More than three-fourths of players (76.6%) who underwent revision returned to play, but just over half (55.3%) returned to the same level of play following surgery. No statistically significant differences were found in the rates of subsequent injuries or subsequent surgeries between docking and modified Jobe techniques or between hamstring and palmaris longus autograft constructs.
The trend we found toward increasing numbers of revision UCL reconstructions being performed in professional baseball players is in agreement with other studies on the topic. Liu et al21 reported a revision rate of 13.2% (31/235) in professional baseball players who underwent UCL reconstruction between 1999 and 2016. This marked a considerable increase from the revision rates reported in earlier studies, which ranged from 1.0 to 1.9%1,27; however, those studies included other overhead athletes in addition to professional baseball players. Similarly, Wilson et al31 reported a revision rate of 15% (40/271) in a cohort of professional baseball players. In that work, the authors cited earlier age at the time of the index surgery, poor adherence to pitched-inning limits, and year-round throwing as potential causes for rising revision rates.31 Given the apparent complexities and inferior outcomes of revision surgery, this increase in revision rate may be cause for concern. Revision UCL reconstructions have been shown to result in lower RTP rates and higher complication rates compared with primary procedures in some studies.6,17,21,25
The majority of revisions in this study were completed through use of the modified Jobe technique, and when combined with those who underwent the docking technique, they accounted for nearly 85% of the cases. Currently, data reporting on the surgical techniques used at the time of revision UCL reconstructions are lacking in the literature. Specifically regarding primary surgery, a recent survey of MLB team orthopaedic surgeons found that 56.7% of respondents preferred the docking technique and 20% preferred the modified Jobe technique. Furthermore, 63.3% reported that the palmaris longus tendon was their preferred graft choice.11 These preferences for primary surgeries differ from the current investigation into revision UCL reconstruction, which demonstrated a predilection toward the modified Jobe technique and a hamstring autograft. This may reflect the fact that the palmaris was used for the primary procedure (and thus was no longer available for the revision surgery), or it could be that the surgeon believed that a large graft (ie, gracilis or semitendinosus) was indicated in the revision setting.
Although both techniques have been shown to provide acceptable outcomes,10,18 a systematic review by Watson et al29 studying primary surgeries demonstrated a significantly higher RTP rate and lower complication rate when the docking technique was used versus the Jobe or modified Jobe. Paletta et al28 reported in a cadaveric study that the docking technique may offer an initial biomechanical advantage over the Jobe construct; however, on the whole, biomechanical studies have failed to consistently demonstrate the superiority of any particular surgical technique.3,10,16,22,23,26 The current study did not show any statistically significant differences in subsequent injuries or subsequent surgeries between surgical techniques or graft constructs. The high rate found in the current study of subsequent elbow injury (29.8%) following revision UCL is consistent with other studies examining subsequent injury rates in professional baseball players undergoing primary UCL reconstruction.8,13 A recent study examining 195 primary UCL reconstructions in professional baseball players found a subsequent injury rate of 50.1% to 56.4%.8 The mean RTP time of 484 days (16 months) in the current study is shorter than RTP times previously reported in revision UCL reconstruction patients, which ranged from 18.9 to 20.76 months.17,21 This discrepancy may be attributable to the fact that these later studies included a relatively small number of patients. In the context of primary UCL reconstruction, Erickson et al9 reported no difference in outcome scores between surgical technique (docking vs double-docking) or graft types (palmaris autograft, hamstring autograft, and allograft). A robust comparative analysis of surgical technique specific to revision UCL reconstructions was not found in the literature. In the absence of any clear superiority, surgical technique selection ultimately depends on the surgeon’s expertise and preference.14
Several limitations in the present study merit discussion. As with all medical records, the validity of the data was reliant on the accurate documentation of player medical information, diagnoses, and outcomes into the HITS database. Although medical personnel and athletic trainers employed by professional baseball organizations are well trained, the potential for errors in data entry is always present. Additionally, preoperative treatments, the exact nature of the injury (site of ligament failure, severity of injury, etc), and postoperative rehabilitation programs were not consistently documented, thus limiting the comparisons that can be drawn about superiority of technique and graft construct. Finally, although this work represents the largest known study of revision UCL reconstructions in professional baseball players, it still may not have been sufficiently powered to detect differences among all of the variables studied. Despite these limitations, the study has a number of strengths. The inclusion of a homogeneous group of professional baseball pitchers allows for more precise comparisons and minimizes confounding variables that may be present if position players and other overhead athletes were included. The use of a comprehensive database (HITS) that was cross-referenced with operative reports allowed for a more complete and accurate representation of the epidemiologic patterns of these injuries. As such, this study provides a thorough epidemiologic report of RTP, RSL, subsequent injuries, and surgical details of revision UCL reconstruction in professional baseball players.
Conclusion
This report detailing revision UCL reconstruction among professional baseball pitchers showed a trend toward increasing numbers of revisions being performed, a finding consistent with other recent studies. The overall RTP percentage was higher than previously reported (76.6%); however, significantly fewer (55.3%) players returned to the same level of play. This work also demonstrated decreased RTP times (mean ± SD, 484 ± 117.3 days) compared with other investigations. The modified Jobe was the most commonly used surgical technique, and the 2 most commonly used graft constructs were hamstring autograft and palmaris longus autograft. Although this analysis did not reveal any statistically significant comparative differences between surgical techniques or graft constructs, future studies involving head-to-head comparisons of these surgical variables, specific to revision UCL reconstruction, may be helpful in improving player outcomes and career performance.
Acknowledgment
Permission to perform and submit this study was granted from Major League Baseball and the Major League Baseball Players Association.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: C.L.C. has received educational support from Arthrex and hospitality payments from Arthrex and Zimmer Biomet. C.S.A. has received royalties from Arthrex and Lead Player; consulting fees from Arthrex; research support from Arthrex, Major League Baseball, and Stryker; and hospitality payments from DePuy; and has stock/stock options in At Peak. M.C. has received research support from Arthrex, consulting fees from Arthrex, and educational support from Liberty Surgical. J.S.D. has received consulting fees from Arthrex, DePuy, Linvatec, Trice Medical, Wright Medical, and Merck Sharp & Dohme; speaking fees from Arthrex; research support from Arthrex; royalties from Linvatec, Thieme, Wolters Kluwer Health–Lippincott Williams & Wilkins; and hospitality payments from Horizon Pharma. D.W.A. has received educational support from Stryker and hospitality payments from Arthrex. T.B.G. has received educational support from Arthrex, Smith & Nephew, and Zimmer Biomet and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Mayo Clinic Institutional Review Board.
References
- 1. Cain EL, Jr, Andrews JR, Dugas JR. et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 2. Camp CL, Dines JS, Voleti PB, James EW, Altchek DW. Ulnar collateral ligament reconstruction of the elbow: the docking technique. Arthrosc Tech. 2016;5(3):e519–e523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ciccotti MG, Siegler S, Kuri JA, II, Thinnes JH, Murphy DJ. Comparison of the biomechanical profile of the intact ulnar collateral ligament with the modified Jobe and the docking reconstructed elbow: an in vitro study. Am J Sports Med. 2009;37(5):974–981. [DOI] [PubMed] [Google Scholar]
- 4. Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 seasons: 1998-2015. Am J Orthop (Belle Mead NJ). 2016;45(3):116–123. [PubMed] [Google Scholar]
- 5. Conte SA, Fleisig GS, Dines JS. et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 6. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36(6):1061–1065. [DOI] [PubMed] [Google Scholar]
- 7. Erickson BJ, Bach BR, Jr, Bush-Joseph CA, Verma NN, Romeo AA. Medial ulnar collateral ligament reconstruction of the elbow in Major League Baseball players: where do we stand? World J Orthop. 2016;7(6):355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Erickson BJ, Chalmers PN, D’Angelo J, Ma K, Dines JS, Romeo AA. Do outcomes or subsequent injuries differ after ulnar collateral ligament reconstruction with palmaris versus hamstring autograft? Am J Sports Med. 2019;47(6):1473–1479. [DOI] [PubMed] [Google Scholar]
- 9. Erickson BJ, Cvetanovich GL, Frank RM. et al. Do clinical results and return-to-sport rates after ulnar collateral ligament reconstruction differ based on graft choice and surgical technique? Orthop J Sports Med. 2016;4(11):2325967116670142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erickson BJ, Harris JD, Chalmers PN. et al. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health. 2015;7(6):511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erickson BJ, Harris JD, Fillingham YA. et al. Treatment of ulnar collateral ligament injuries and superior labral tears by Major League Baseball team physicians. Arthroscopy. 2016;32(7):1271–1276. [DOI] [PubMed] [Google Scholar]
- 12. Erickson BJ, Nwachukwu BU, Rosas S. et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. [DOI] [PubMed] [Google Scholar]
- 13. Griffith TB, Ahmad CS, Gorroochurn P. et al. Comparison of outcomes based on graft type and tunnel configuration for primary ulnar collateral ligament reconstruction in professional baseball pitchers. Am J Sports Med. 2019;47(5):1103–1110. [DOI] [PubMed] [Google Scholar]
- 14. Hibberd EE, Brown JR, Hoffer JT. Optimal management of ulnar collateral ligament injury in baseball pitchers. Open Access J Sports Med. 2015;6:343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction: a 10-year study in New York State. Am J Sports Med. 2016;44(3):729–734. [DOI] [PubMed] [Google Scholar]
- 16. Jackson TJ, Adamson GJ, Peterson A, Patton J, McGarry MH, Lee TQ. Ulnar collateral ligament reconstruction using bisuspensory fixation: a biomechanical comparison with the docking technique. Am J Sports Med. 2013;41(5):1158–1164. [DOI] [PubMed] [Google Scholar]
- 17. Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2013;22(5):642–646. [DOI] [PubMed] [Google Scholar]
- 18. Jones KJ, Osbahr DC, Schrumpf MA, Dines JS, Altchek DW. Ulnar collateral ligament reconstruction in throwing athletes: a review of current concepts. AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(8):e49. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan DJ, Glait SA, Ryan WE, Jr, Jazrawi LM. Modified Jobe approach with docking technique for ulnar collateral ligament reconstruction. Arthrosc Tech. 2016;5(6):e1321–e1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Keller RA, Mehran N, Marshall NE. et al. Major League pitching workload after primary ulnar collateral ligament reconstruction and risk for revision surgery. J Shoulder Elbow Surg. 2017;26(2):288–294. [DOI] [PubMed] [Google Scholar]
- 21. Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elbow Surg. 2016;25(1):90–97. [DOI] [PubMed] [Google Scholar]
- 22. Lynch JL, Maerz T, Kurdziel MD, Davidson AA, Baker KC, Anderson K. Biomechanical evaluation of the TightRope versus traditional docking ulnar collateral ligament reconstruction technique: kinematic and failure testing. Am J Sports Med. 2013;41(5):1165–1173. [DOI] [PubMed] [Google Scholar]
- 23. Lynch JL, Pifer MA, Maerz T. et al. The GraftLink ulnar collateral ligament reconstruction: biomechanical comparison with the docking technique in both kinematics and failure tests. Am J Sports Med. 2013;41(10):2278–2287. [DOI] [PubMed] [Google Scholar]
- 24. Makhni EC, Lee RW, Morrow ZS, Gualtieri AP, Gorroochurn P, Ahmad CS. Performance, return to competition, and reinjury after Tommy John Surgery in Major League Baseball pitchers: a review of 147 cases. Am J Sports Med. 2014;42(6):1323–1332. [DOI] [PubMed] [Google Scholar]
- 25. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43(5):1051–1056. [DOI] [PubMed] [Google Scholar]
- 26. Morgan RJ, Starman JS, Habet NA. et al. A biomechanical evaluation of ulnar collateral ligament reconstruction using a novel technique for ulnar-sided fixation. Am J Sports Med. 2010;38(7):1448–1455. [DOI] [PubMed] [Google Scholar]
- 27. Osbahr DC, Cain EL, Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 28. Paletta GA, Jr, Klepps SJ, Difelice GS. et al. Biomechanical evaluation of 2 techniques for ulnar collateral ligament reconstruction of the elbow. Am J Sports Med. 2006;34(10):1599–1603. [DOI] [PubMed] [Google Scholar]
- 29. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42(10):2510–2516. [DOI] [PubMed] [Google Scholar]
- 30. Whiteside D, Martini DN, Lepley AS, Zernicke RF, Goulet GC. Predictors of ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44(9):2202–2209. [DOI] [PubMed] [Google Scholar]
- 31. Wilson AT, Pidgeon TS, Morrell NT, DaSilva MF. Trends in revision elbow ulnar collateral ligament reconstruction in professional baseball pitchers. J Hand Surg Am. 2015;40(11):2249–2254. [DOI] [PubMed] [Google Scholar]