In the basement of a state psychiatric hospital—a stereotypically dark, drab, and run-down building—a training session is being conducted to teach researchers how to engage with individuals who are experiencing symptoms that might presage psychosis. Bethany stares at the screen. The introduction spells out what she remembers to be true: young people at risk of developing schizophrenia sometimes hear things that other people do not. She thinks back to herself at 13 years of age, terrified and confused as she pressed her ear to her desk and listened to what sounded like people conversing inside. She thought she was going crazy then, and now she thinks that maybe she really was, but she never went to a psychiatrist for help and somehow ended up okay. In fact, she now sits on the other side of the couch, engaging young people with experiences like her own and trying to figure out how to make their path as easy as possible.
Bethany is not alone. Approximately 13% of people in the world’s general population hear voices (1). Considering that schizophrenia has a prevalence rate of only 1%, it is clear that individuals with a psychotic disorder are only a portion of those with hallucinations. Who are these healthy voice- hearers? Are the voices they hear like those heard in clinical populations? And is the underlying mechanism the same? Remarkably, despite the importance of these questions, they have only recently received attention in the scientific literature. Over the past several years, a team of researchers at Yale University (including ARP and PRC) set out to systematically explore this topic.
Their first challenge was to find people who hear voices but have never felt the desire to seek psychiatric care. Previous studies have used epidemiologic approaches, sending out questionnaires to large swaths of the population. The Yale University team decided to take the opposite approach and ask: Assuming people like this exist in the general population, where might they congregate? In what settings might hearing voices be considered positive or special rather than pathological? The answer came through contact with a clairaudient psychic medium.
Clairaudient psychic mediums believe that they receive auditory verbal messages from spirits (as opposed to clairvoyants, who receive visions), and that this experience is a gift meant to help others. In a peculiar way, this paralleled how the researchers viewed the psychics’ experiences—as a gift with the potential to help others (in their case, through a clearer understanding of what causes those experiences). With this shared alignment of goals, participants quickly began to recruit others like themselves to help with the project.
With a population of willing participants, the team began addressing one of the most basic questions: Are the messages heard by healthy voice-hearers qualitatively similar to the auditory verbal hallucinations experienced by patients with schizophrenia? They tested both groups using a structured interview that included both clinical questions and forensic instruments specifically designed to detect the malingering of voices. Intriguingly, both groups reported similar perceptual experiences, with respect to loudness, location in space, complexity of syntax, gender, and identity of the voices. Neither group endorsed experiences that were thought to be malingering. However, consistent with previous studies of nonclinical voice-hearers (2), the psychic group differed in the attribution they assigned to their voice-hearing (predominantly seen as a positive spiritual gift), their emotional response (less frightened), their engagement with their voices (more likely to seek them out), and their ability to control various aspects of their experiences (3).
These were fascinating data, suggesting that the voices were as “real” as those experienced by individuals with psychotic disorders. But that still did not indicate how and why the experiences might occur. To explore this question, the team adopted an approach that was rooted in an understanding of the mechanisms of perception (4). We often think of perception as being a relatively passive process—information about the world is detected by our sensory organs and relayed to higher centers. But a considerable body of literature suggests a more nuanced perspective: that perception entails an active process in which our mind generates a model of the environment that is informed not only by our sensory inputs but also by our previous experiences and expectations about the world. This dynamic balance is crucial for accurate perception. Having heightened expectations might allow us to perceive things that would otherwise go unnoticed (such as hearing a baby crying over the sound of an air conditioner). At the same time, if this balance is excessively shifted toward overweighting previous beliefs, we may perceive something to exist in the absence of a sensory stimulus-which is to say, we may hallucinate. As a common modern example, many individuals can relate to the phenomenon of “phantom phone syndrome” (5)-a nonclinical hallucination that may work in exactly this way. What if auditory verbal hallucinations might stem from a similar mechanism?
To test this hypothesis, the team brought together four groups of subjects: individuals who did or did not hear voices, with and without a previous diagnosis of a psychotic disorder. They then gave subjects a relatively straightforward hearing test, asking them to press a button every time they heard a faintly presented tone. The catch was that at the same time each tone was played, subjects were also presented with a light. After a series of trials (increasing in frequency across the duration of the experiment), subjects were sometimes presented with only the light. The key question was this: If individuals were trained to associate seeing a light with hearing a tone, might their strong beliefs about this pairing cause them to experience a conditioned hallucination and perceive a tone even when it was not there? Using computational models, it was then possible to ask: To what degree did participants’ previous beliefs influence their perception (i.e., were some groups more likely to experience conditioned hallucinations?), and how well were subjects able to update their beliefs about the experiment (as the likelihood of hearing a tone decreased)? Moreover, by collecting functional magnetic resonance imaging data during task performance, the team could begin to assess which neural circuits might underlie these processes.
Consistent with the premise of the experiment (i.e., that everyday perception entails a balance of previous beliefs and sensory stimulation), all subjects experienced some conditioned hallucinations. Of note, compared to the general population, people who hear voices were significantly more susceptible to this effect (regardless of whether they had a history of psychiatric illness). These data are consistent with the hypothesis that hallucinations may be caused by an overweighting of prior beliefs. The analysis also showed that individuals with a psychotic disorder (regardless of whether they heard voices) were less likely to update their beliefs about the relationships between the stimuli. Thus, the behavioral data suggested a double-dissociation between hallucinations and psychosis.
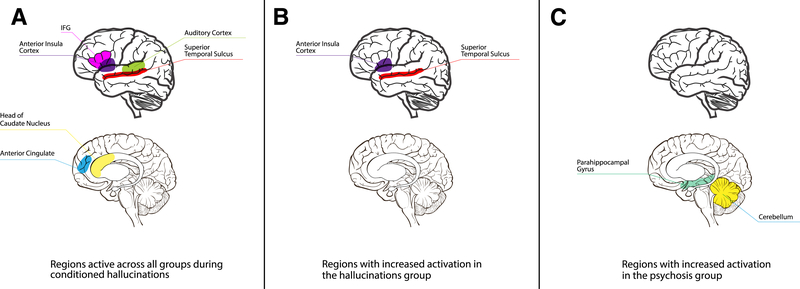
To better understand these results, the group then examined the functional magnetic resonance imaging data. Looking across all participants, the researchers were able to identify a brain circuit that was active during conditioned hallucinations. Interestingly, this circuit was similar to one previously identified to be active when people are hallucinating voices. This paradigm may therefore be a valid model for studying auditory hallucinations. The team also found unique areas of activity in participants who hear voices and unique areas of activity in those with a diagnosis of a psychotic disorder (Figure 1). These data suggest that it may be possible to dissect psychotic experiences into constituent symptoms and thereby open a deeper understanding of the connection between brain function and subjective experience.
Figure 1.
(A) Regions active across all groups during conditioned hallucinations: the auditory cortex, anterior insula cortex, inferior frontal gyrus (IFG), head of the caudate nucleus, anterior cingulate cortex, and posterior superior temporal sulcus. (B) Regions that differentiated participants with hallucinations from those without: the superior temporal sulcus and anterior insula. (C) Regions that differentiated those with a psychotic disorder from those without: the parahippocampal gyrus and cerebellum.
Returning to Bethany’s story, one central question remains: Are healthy voice-hearers individuals who once were at risk of developing a psychotic disorder but somehow avoided it? This is tricky to answer without longitudinal follow-up, but epidemiological data suggest that it may be possible. Of young people who present with potentially prodromal symptoms, including hallucinations, only approximately 10% to 25% will develop a frank psychotic disorder, approximately 55% to 65% will experience a complete resolution of symptoms, and approximately 10% to 30% will continue to manifest attenuated symptoms but not develop a psychotic disorder (6,7). The question of which individuals will go on to develop a major illness remains unknown. A range of demographic and clinical factors may predict risk of conversion to schizophrenia (8), but these measures offer limited insight into the pathophysiological changes that underlie this process. In this issue, Plavén-Sigray et al. (9) explore the possible role of inflammation, though considerable work remains to better understand this critical pathologic process.
While many questions remain unanswered, Bethany’s story offers hope. In our clinical settings, we often see only the sickest patients. Bethany reminds us that many individuals with psychosis-like symptoms may not only recover but thrive, even in the absence of psychiatric care. Over the years, Bethany turned her once terrifying voice-hearing into an asset that she has used to offer spiritual guidance to those seeking help. Moreover, her and her peers’ willingness to collaborate in research paves the way for new avenues of discovery that may ultimately lead to new treatments.
Acknowledgments and Disclosures
Clinical Commentaries are produced in collaboration with the National Neuroscience Curriculum Initiative (NNCI). David A. Ross, in his dual roles as co-chair of the NNCI and as Education Editor of Biological Psychiatry, manages the development of these commentaries but plays no role in the decision to publish each commentary. The NNCI is supported by the National Institutes of Health Grant Nos. R25 MH08646607S1 and R44 MH115546-01.
This work was supported by a Brain and Behavior Research Foundation Young Investigator Award, the Burroughs-Wellcome Fund Career Award for Medical Scientists, the Yale Department of Psychiatry, and the Yale School of Medicine (to AP), National Institute of Mental Health Grant Nos. K23 MH115252-01A1 (to ARP) and R01MH1128875 and R01MH067073-09 (to PRC), an International Mental Health Review Order/Janssen Rising Star Translational Research Award, Clinical and Translational Science Awards Grant No. UL1 TR000142 from the National Center for Research Resources and the National Center for Advancing Translational Science, components of the National Institutes of Health, the National Institutes of Health Roadmap for Medical Research, Clinical Neurosciences Division, U.S. Department of Veterans Affairs, and the National Center for Post-Traumatic Stress Disorders, Veterans Affairs Connecticut Healthcare System (to PRC). The contents of this work are solely the responsibility of the authors and do not necessarily represent the official view of National Institutes of Health or the Connecticut Mental Health Center/Division of Mental Health and Addiction Services.
Footnotes
The authors report no biomedical financial interests or potential conflicts of interest.
References
- 1.Beavan V, Read J, Cartwright C (2011): The prevalence of voice-hearers in the general population: A literature review. J Ment Health 20:281–292. [DOI] [PubMed] [Google Scholar]
- 2.Johns LC, Kompus K, Connell M, Humpston C, Lincoln TM, Longden E, et al. (2014): Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull 40(suppl 4):S255–S264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powers AR 3rd, Kelley MS, Corlett PR (2017): Varieties of voice-hearing: Psychics and the psychosis continuum. Schizophr Bull 43:84–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powers AR, Mathys C, Corlett PR (2017): Pavlovian conditioning-induced hallucinations result from overweighting of perceptual priors. Science 357:596–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothberg MB, Arora A, Hermann J, Kleppel R, St Marie P, Visintainer P (2010): Phantom vibration syndrome among medical staff: A cross sectional survey. BMJ 341:c6914. [DOI] [PubMed] [Google Scholar]
- 6.Woods SW, Walsh BC, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, et al. (2014): Current status specifiers for patients at clinical high risk for psychosis. Schizophr Res 158:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schlosser DA, Jacobson S, Chen Q, Sugar CA, Niendam TA, Li G, et al. (2012): Recovery from an at-risk state: Clinical and functional outcomes of putatively prodromal youth who do not develop psychosis. Schizophr Bull 38:1225–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cannon TD, Yu C, Addington J, Bearden CE, Cadenhead KS, Cornblatt BA, et al. (2016): An individualized risk calculator for research in prodromal psychosis. Am J Psychiatry 173:980–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plavén-Sigray P, Matheson GJ, Collste K, Ashok AH, Coughlin JM, Howes OD, et al. (2018): Positron emission tomography studies of the glial cell marker translocator protein in patients with psychosis: A meta-analysis using individual participant data. Biol Psychiatry 84:433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]