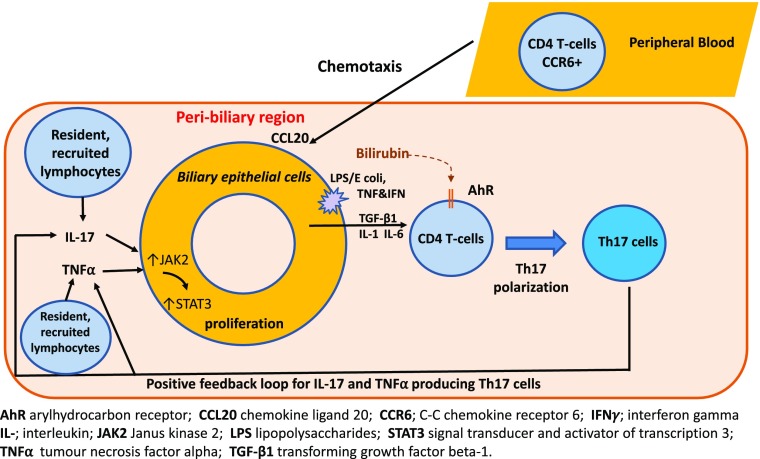
FIGURE 6.
An illustration of the bidirectional interaction between Th17 and BEC. Migrating bacteria from the gut express pathogen-associated molecular patterns (e.g., LPS) that trigger BEC activation via TLR4 signaling. The downstream cascade involves proinflammatory cytokines and chemokines, such as IL-1, IL-6, TGF-β1, and CCL20. IL-6 is both secreted by BEC and stimulates BEC proliferation via the JAK2/STAT3 signaling pathway in an autocrine manner. Importantly, although BEC undergo increased proliferation, this does not lead to increased apoptosis or necrosis. BEC-secreted CCL20 is responsible for chemotaxis and subsequent transmigration of lymphocytes that are CCR6+ (complementary receptor). The CD4+ lymphocytes undergo alterations in differentiation status, lineage stability, and function, depending on their respective subset. These cytokines act on BEC leading to BEC proliferation, which completes a self-sustaining positive feedback loop that propagates chronic peribiliary inflammation and biliary regeneration. This LPS-stimulated inflammatory cascade could be synergistically augmented by exposure to local bilirubin via the AhR present on lymphocytes.