I 2019, the twenty-two U.S. states have reported outbreaks. This means that a measles outbreak is not just a plane ride away but also could be just a bus ride or car trip away.
In the pre-vaccine era in the U.S., nearly all who were susceptible—up to 3–4 million individuals— developed measles each year, and in the early 1900s an average of 6,000 deaths occurred. In the 1950s and early 1960s, measles peaks, commonly noted during late winter and spring, were still associated with an increased risk for death (1 in 10,000 cases), especially in malnourished children.
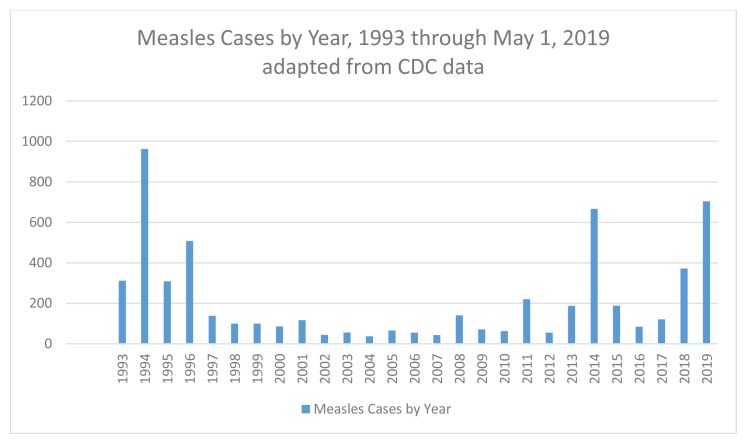
Routine measles vaccination of infants at one year of age was introduced in 1967; however, because outbreaks continued, the Centers for Disease Control & Prevention (CDC) Advisory Committee on Immunization Practices in 1989 recommended a second dose of measles, mumps, and rubella (MMR) vaccine before school entry. A significant drop in confirmed cases between 1993 and 2001 prompted a declaration that endemic measles had been eradicated in the U.S. in the year 2000.
In the next decade, spikes in the number of cases occurred sporadically, mostly linked to importation of disease in international travelers or to outbreaks in U.S. communities with large pockets of unimmunized. Outbreaks attracting particular media attention included the 2015 California Disneyland outbreak that resulted in multi-state spread as well as the 2017 Minnesota outbreak that occurred in Somalian Americans.
What makes the current statistics most concerning is that as of May 24, 2019, we now have 26 states (Arizona, California, Colorado, Connecticut, Florida, Georgia, Illinois, Indiana, Iowa, Kentucky, Maine, Maryland, Massachusetts, Michigan, Missouri, New Mexico, Nevada, New Hampshire, New Jersey, New York, Oklahoma, Oregon, Pennsylvania, Texas, Tennessee, and Washington) that have reported confirmed measles cases.1 There have been seven states with ongoing outbreaks in the first four months of 2019—resulting in the largest number of measles cases in the last 25 years (Figure 1).
Figure 1.
Measles Cases by Year
There are five likely reasons to explain why the 2019 outbreak is occurring and has been difficult to contain:
Disease is just a plane ride away given that multiple countries have substantial measles burden.
While national MMR adherence rates are at or near the herd immunity threshold of 93%, there are pockets of under-immunized or unimmunized.
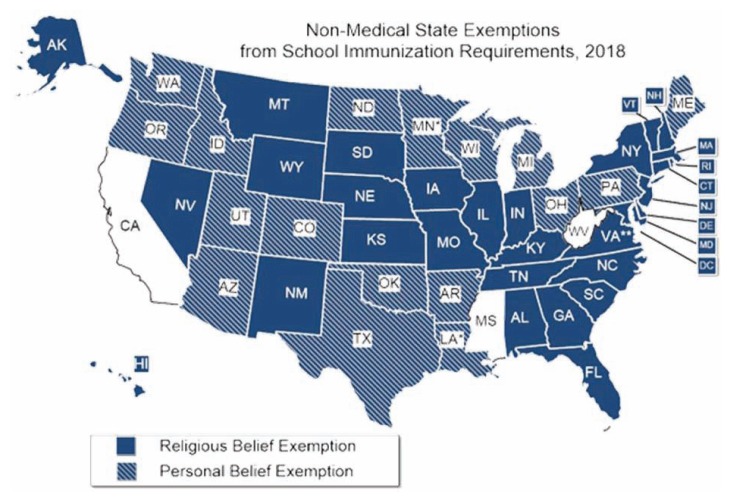
Personal vaccine exemptions are allowed in 18 states and “hotspot” metropolitan communities have been identified (Figure 2).
Measles is highly contagious and spreads easily to susceptible individuals.
Measles is difficult to recognize in the prodromal stage.
Figure 2.
States Allowing Non Medical Exemptions
Not Just a Plane Ride Away
To flourish, measles needs introduction into the “fertile ground” of persons not immune to measles. Lack of immunity can be by choice (vaccine declination due to personal, philosophical, or religious reasons) or due to true vaccine-contraindication (e.g. immune-compromised hosts or those too young to be eligible for vaccine). Measles virus exposure of a cluster of non-immune persons creates a bigger ripple effect than if there is only an occasional non-immune person. Think of an exposure within a non-immune cluster as multiple stones causing multiple overlapping secondary ripples when skipped across a pond. In contrast, an exposure in a mostly immune population with herd immunity (>93% of exposed are immunized) is like a single stone dropped in a pond causing one small concentric set of ripples.
Measles introductions have classically been via a person who is in the incubation period traveling to the U.S. by airplane from a country already having an outbreak. Years ago, outbreak countries were mostly in the developing world. Not all of the top 10 countries for measles cases during the last eighteen months per the World Health Organization have been in developing countries; top ten measles countries include Madagascar, Ukraine, India, Nigeria, Kazakhstan, Chad, Myanmar, Thailand, Philippines, and Republic of Congo.2
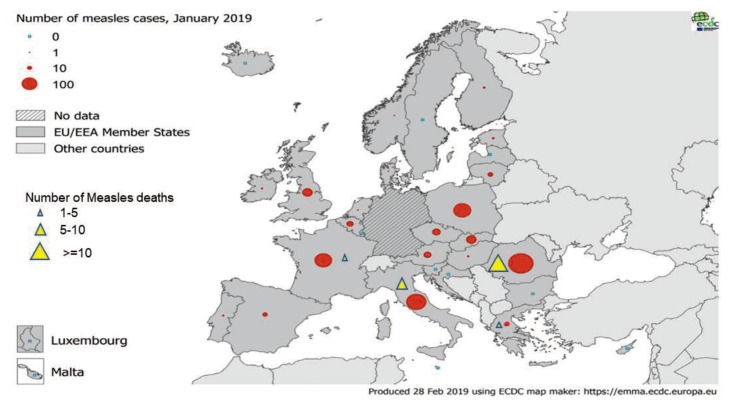
Europe has also been a not uncommon measles source over the past ten years, with France, Italy, Romania, Greece, Macedonia, and Serbia having the highest European rates; and the UK and Turkey are not far behind (Figure 3).
Figure 3.
Measles Cases and Deaths in Europe from January 2018 – January 2019.
https://ecdc.europa.eu/sites/portal/files/documents/measles-monthly-report-march-2019.pdf
MMR Adherence is Not Uniform
But now in 2019, the 22 U.S. states (Figure 1) having reported outbreaks confirm that most, if not all, states have measles-non-immune clusters. This means that a measles outbreak is not just a plane ride away but also could be just a bus ride or car trip away. CDC reports of vaccine adherence show that MMR coverage varies by state.3–5 Twenty-four states and the District of Columbia (DC) had 2017 MMR adherence rates below 93% at kindergarten age. 4 The lowest rates were in D.C. (~83%), Colorado, Kansas, Washington, Minnesota, Alaska, and Indiana.
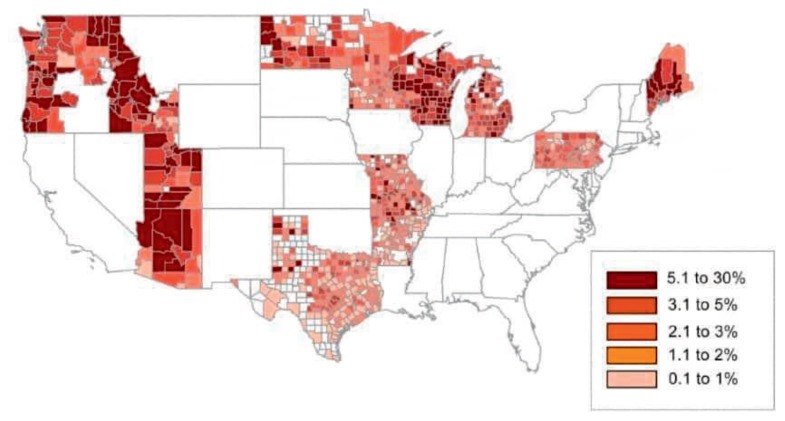
Another recent report of a model predicting measles outbreaks used the number of international flights from endemic countries together with apparent clusters of under-immunized persons within states and even among zip codes within cities6 to project Chicago, New York, Miami, Los Angeles, Washington state and mid-Texas as likely near-future measles epicenters (likely hotspots) (Figure 4).
Figure 4.
Review of selected states by county for rates of vaccine exemptions.
Nonmedical Exemptions Are Allowed in Most States
While all 50 states have measles vaccine mandates for school attendance, almost all allow for religious exemptions and eighteen states allow for philosophical or personal exemptions.7 The reported “hotspot” metropolitan locales where large numbers of kindergarteners have not received MMR vaccine have been linked to the increase in overall state nonmedical exemption (NME) rates. Cities with increased NMEs include Seattle and Spokane in Washington; Portland, Oregon; Phoenix, Arizona; Salt Lake City and Provo, Utah; Houston, Fort Worth, Plano, and Austin, Texas; Troy, Warren and Detroit, Michigan; Kansas City, Missouri; and Pittsburgh, Pennsylvania.6 Data also demonstrate that areas with the highest NME rates were in rural counties, e.g. in the state of Idaho. It’s critical to know that children with NME for MMR vaccine are 35 times as likely to develop measles as a child who has been immunized. Those children who develop measles and recover, still run the risk, estimated at 1:609 for those who are infected at age ≤12 months and 1:1367 <5 years, to develop a fatal, late stage complication of measles, namely, subacute sclerosing panencephalitis (SSPE) years later. Based on data from the CDC and California Encephalitis Project, such cases occurred in children with a median age of 12 years, but as young as 3 years and as old as 35 years.8
The median coverage for the two-dose schedule for MMR vaccine is 94.3% in the U.S.—but was below the herd immunity threshold of 93% in Alaska, Arkansas, Colorado, DC, Idaho, Indiana, Kansas, Kentucky, Minnesota, Ohio, Wisconsin, and Washington. Also remember that even in states with 93% coverage, clusters of non-immunized children can exist. 9
Measles is Highly Contagious
In addition to strengthening the emphasis on removing NME options, the national response to this outbreak depends on practitioners to promote MMR vaccine and expand access, and community campaigns to increase awareness. Awareness is critical for both the general public and medical providers because measles is one of the top three most contagious infections in the world, two to three times as contagious as mumps, rubella, smallpox, diphtheria, or polio. And unlike most other infections, it is spread airborne, meaning that spread doesn’t require direct contact with an infectious person or fomite. Merely inhaling air in the same area as an infected person will transmit measles to a non-immune person, hence the extreme measures needed for infection control and quarantine practices.
Measles Prodrome is Nonspecific
Another factor in potentially rapid and extensive spread is that there are typically 8–12 days of incubation, so a person can acquire measles from an exposure and travel long distances and across many areas before prodromal symptoms begin. Diagnosing the prodromal symptoms as measles is also difficult because the fever, headache, and myalgia mimic many other infections. This results in a contagious timeframe of 5–21 days after exposure (patients can be contagious even before symptom onset), although contagion usually recedes four days after onset of rash in immune competent patients.
The good news is that we have a proven tool for treating measles now, e.g. Vitamin A supplementation. And, nutrition is generally better than in the early 19th century when measles deaths were more common. With over 800 cases and counting in the U.S. at the time of writing this article (mid-May 2019), this will be the biggest outbreak since the 1990s.
Hopefully, we will not see a measles death in the U.S. this year – or ever. But if the U.S. national outbreak is not controlled, deaths may occur as have been reported in Europe (33 deaths in the past 12 months)10 (Figure 3). And by 2029, we could again start seeing the late and devastating complication of measles disease, subacute sclerosing panencephalitis (SSPE), a progressive and fatal dementia. We can only hope that the public health interventions added to individual clinicians doubling down on administering MMR per the recommended schedule (including catch up dosing) will curb this outbreak’s momentum and prevent such tragedies.
One aspect of outbreak control may come down to accelerating MMR schedules (immunizing infants 6–12 months old and giving second MMR doses before 4–6 years of age) if public health officials deem it necessary at hotspots or for children traveling to U.S. hotspots. Accelerated MMR dosing of 6–12-month olds produces an immune response but such doses are not “valid” for school attendance in most areas. So reimmunization at 12–15 months of age is usually needed. A repeat dose is also a potential issue for patients receiving a second MMR before 4 years of age (also not valid for most school districts), given recent experience with waning protection against mumps developing five years after the most recent MMR.11
Of note, longtime measles expert, James Cherry, MD, has long been a champion of a second MMR at 1–3 months after the 12–15 month MMR dose to catch up the 5% or so primary failures, and this is an option per current Advisory Committee on Immunization Practices (ACIP) schedules. Regardless, we need to keep track of children getting accelerated MMR dosing to ensure the repeat doses at a future date do not fall between the cracks.
Summary
As clinicians we need to make strong recommendations for maintaining on-time (if not accelerated) vaccine schedules. Most people listen to us when we are firm in our recommendations. And it is important now to ask the extra question to decide if an accelerated schedule is needed – “Any travel in the near future?” – but with a twist, i.e. it is not just foreign now, even a domestic travel can be to an outbreak area.
Footnotes
Mary Anne Jackson, MD, FAAP, FIDSA, FPIDS, is Interim Dean and Professor of Pediatrics; Christopher J. Harrison, MD, Director, Infectious Disease Research Laboratory, Director, Vaccine and Treatment Evaluation Unit, Professor of Pediatrics; both at the University of Missouri-Kansas City School of Medicine, Kansas City, Mo.
Contact: jacksonmar@umkc.edu
References
- 1.National Conferences of State Legislatures. http://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx.
- 2.Measles and Rubella Surveillance Data. https://www.cdc.gov/measles/cases-outbreaks.html Last updated May 24 2019.
- 3.WHO. Measles Cases and Outbreaks. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/Last updated May 13, 2019.
- 4.Mellerson JL, Maxwell CB, Knighton CL, Kriss JL, Seither R, Black CL. Vaccination Coverage for Selected Vaccines and Exemption Rates Among Children in Kindergarten — United States, 2017–18 School Year. MMWR Morb Mortal Wkly Rep. 2018;67:1115–1122. doi: 10.15585/mmwr.mm6740a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties. PLoS Med. 2018;15(6):e1002578. doi: 10.1371/journal.pmed.1002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill Holly A, Elam-Evans Laurie D, Yankey David, Singleton James A, Kang Yoonjae. Vaccination Coverage Among Children Aged 19–35 Months — United States, 2017. MMWR. 2018 Oct 12;67(40):1123–1128. doi: 10.15585/mmwr.mm6740a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mellerson Jenelle L, Maxwell Choppell B, Knighton Cynthia L, Kriss Jennifer L, Seither Ranee, Black Carla L. Vaccination Coverage for Selected Vaccines and Exemption Rates Among Children in Kindergarten — United States, 2017 18 School Year. Weekly. 2018 Oct 12;67(40):1115–1122. doi: 10.15585/mmwr.mm6740a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evaluating Vaccination Coverage Trends with the National Immunization Survey-Child (NIS-Child), 2013–2017, United States: Technical Appendix. https://www.cdc.gov/vaccines/imz-managers/coverage/childvaxview/pubs-presentations/NIS-vax-trends-2013-2017.html
- 9.Lewnard JA, Grad YH. Vaccine waning and mumps re-emergence in the United States. Sci Transl Med. 2018 Mar 21;10(433) doi: 10.1126/.scitranslmed.aao5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Measles Deaths in Europe. https://ecdc.europa.eu/sites/portal/files/documents/measles-monthly-report-march-2019.pdf.
- 11.Wendorf KA, Winter K, Zipprich J, et al. Subacute Sclerosing Panencephalitis: The Devastating Measles Complication That Might Be More Common Than Previously Estimated. Clin Infect Dis. 2017 Jul 15;65(2):226–232. doi: 10.1093/cid/cix302. [DOI] [PubMed] [Google Scholar]