Fig. 1.
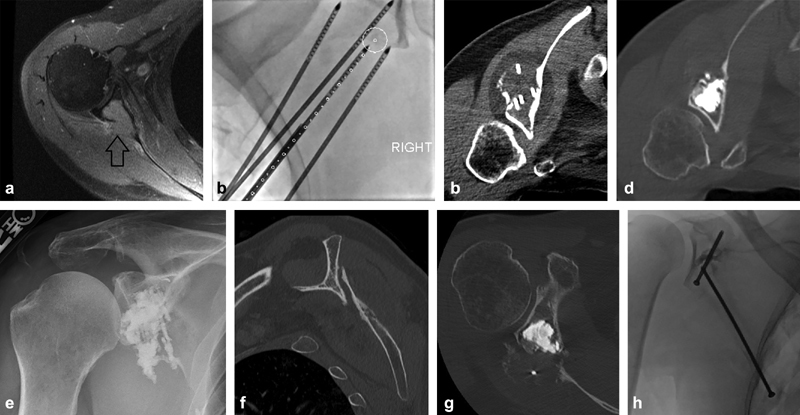
A 54-year-old man with a history of metastatic renal cell carcinoma presenting with right shoulder pain. Initial imaging demonstrated a right scapular lesion with posterior cortical destruction and invasion into the glenoid body but no definite fracture extension into the joint (arrow) ( a ). He received palliative radiation therapy, but was admitted to the hospital with persistent severe shoulder pain 1 month later. Open surgical repair was not offered as first-line therapy given the expected surgical morbidity and required interruption in ongoing systemic therapies in the setting of progressive disease. Goals of therapy included pain palliation, increased shoulder mobility, prevention of disease progression into the glenoid cortex and articular surface, and reinforcement of the glenoid to prevent stress fracture. Cryoablation was chosen for maximal visualization of the ablation zone and minimal damage to the adjacent joint. Four probes were placed using needle guidance software to optimize tumor coverage ( b ). Following cryoablation ( c ), a “hot” thaw was performed with active heating of the ablation probe tips for greater than 15 minutes to melt the ice and facilitate cement deposition. The glenoid cavity was then filled with polymethyl methacrylate under intermittent CT imaging to ensure no extravasation into the joint ( d ). Pain and function were significantly improved postoperatively ( e ). Unfortunately, he developed recurrent pain 2 months later and CT scan demonstrated a scapular body fracture with severe displacement and over-ride ( f ), despite the glenoid remaining well reinforced ( g ). Nonoperative management was chosen due to the expected morbidity associated with any operation and the patient's desire to avoid an extensive operation. For lesions isolated to the glenoid, osteoplasty alone is usually clinically sufficient to resist the compressive forces in this area with arm abduction; however, there was significant tumor destruction extending down into the midscapular body, and this fracture likely occurred due to a combination of overuse during the healing phase and multidirectional stress forces in the area of fracture. The addition of a scapular body screw ( h ), despite its inherent challenges, may have provided superior stabilization in this setting.
