Abstract
Breast cancer survivors (BCS) often experience psychological and physiological symptoms after cancer treatment. Mindfulness-based stress reduction (MBSR), a complementary and alternative therapy, has reduced subjective measures of stress, anxiety, and fatigue among BCS. Little is known, however, about how MBSR affects objective markers of stress, specifically the stress hormone cortisol and the pro-inflammatory cytokine interleukin-6 (IL-6). In the present study, BCS (N = 322) were randomly assigned to a 6-week MBSR program for BC or usual-care control. Measurements of cortisol, IL-6, symptoms, and quality of life were obtained at orientation and 6 weeks. Cortisol and IL-6 were also measured prior to and after the MBSR(BC) class Weeks 1 and 6. The mean age of participants was 56.6 years and 69.4% were White non-Hispanic. Most had Stage I (33.8%) or II (35.7%) BC, and 35.7% had received chemotherapy and radiation. Cortisol levels were reduced immediately following MBSR(BC) class compared to before the class Weeks 1 and 6 (Wilcoxon-signed rank test; p < .01, d = .52–.56). IL-6 was significantly reduced from pre- to postclass at Week 6 (Wilcoxon-signed rank test; p < .01, d = .21). No differences were observed between the MBSR(BC) and control groups from baseline to Week 6 using linear mixed models. Significant relationships with small effect sizes were observed between IL-6 and both symptoms and quality of life in both groups. Results support the use of MBSR(BC) to reduce salivary cortisol and IL-6 levels in the short term in BCS.
Keywords: mindfulness-based stress reduction, breast cancer, stress hormone, cytokine
It was estimated that 252,710 new cases of invasive breast cancer (BC) would be diagnosed in 2017 (American Cancer Society, 2017). BC survivors (BCS) are confronted with physiological and psychological stressors, often related to their diagnosis and treatment, which may continue long after treatment ends (McGregor & Antoni, 2009). Persistent emotional distress can activate the secretion of stress hormones (Saboonchi, Petersson, Weenman-Larsen, Alexanderson, & Vaez, 2015). Evidence indicates that it is not the repeated exposure to stress that causes negative outcomes but rather the exposure to chemical mediators of stress (e.g., cortisol; McEwen, 1998). For example, cortisol can be protective in acute responses; however, chronic elevations of cortisol can cause damaging effects (McEwen, 2000). While the consequences of increased levels of cortisol are largely unknown among cancer survivors, cortisol has been associated with survival and symptoms in several landmark studies (Abercrombie, Giese-Davis, Sephton, Epel, & Turner-Cobb, 2004; Sephton, Sapolsky, Kraemer, & Spiegel, 2000; Turner-Cobb, Sephton, Koopman, Blake-Mortimer, & Spiegel, 2000). Disruption of cortisol function can affect cancer risk and progression (Spiegel, 2012). Particular to metastatic BC patients, flattened cortisol levels have been associated with decreased survival (Sephton et al., 2000).
Similar to cortisol, increased levels of cytokines, specifically interleukin-6 (IL-6), have been associated with acute and chronic stress levels (Rohleder, Aringer, & Boentert, 2012). IL-6 is a pro-inflammatory cytokine that stimulates inflammation by activating T cytotoxic cells, B-cell production of antibodies, complement and acute-phase proteins and by promoting phagocytosis and increasing vascular permeability and cellular adhesion (Rohleder, Aringer, & Boentert, 2012). Depression can produce elevated levels of IL-6, which may lead to metastasis (McEwen, 2007; Spiegel, 2012).
Some harmful effects of biological stress markers may be reversible through lifestyle changes, yet few behavioral interventions have been consistently implemented and examined to determine their impact on stress in daily lives, particularly among cancer survivors (McEwen, 2000, 2007). Research has shown, however, that mindfulness-based stress reduction (MBSR) programs reduced cortisol levels significantly in cancer patients (Carlson, Speca, Faris, & Patel, 2007) and cancer patient/caregiving dyads (Lengacher et al., 2012) as well as reduced IL-6 and pro-inflammatory gene expression in older adults experiencing loneliness (Creswell et al., 2012) and women with a history of trauma (Gallegos, Lytle, Moynihan, & Talbot, 2015). Although results indicate a relationship between MBSR and levels of cortisol and IL-6, it is unclear whether cortisol and IL-6 can serve as objective markers for stress reduction.
MBSR is a clinical stress-reducing program shown to reduce stress through self-regulation of arousal to stressful circumstances or symptoms. Training in mindfulness meditation increases individuals’ attention to their breath and body sensations, allowing for nonreactive awareness of internal and external stimuli (Baer, 2003; Bishop et al., 2004). Among BCS, researchers have found that MBSR decreases psychological symptoms such as depression, anxiety, stress, and fear of recurrence along physical symptoms of fatigue and pain while also improving sleep (Henderson et al., 2012; Hoffman et al., 2012; Lengacher et al., 2009; Lengacher et al., 2012; Lengacher et al., 2015; Lengacher et al., 2016; Wurtzen et al., 2013). Although there is evidence of the positive effects of MBSR on immune function and stress hormones, the potentially beneficial effects of MBSR programs on the stress hormone cortisol and cytokine IL-6 levels are still under investigation (Lengacher et al., 2012).
Cortisol and IL-6 results have varied in nonrandomized studies of MBSR. Carlson, Speca, Faris, and Patel (2007) found that improvements in quality of life were associated with decreases in afternoon cortisol levels following MBSR. In a pilot study by our team, breast, lung, colon, and prostate cancer patients and/or their caregivers had significant decreases in salivary cortisol from pre- to postsession at Weeks 1 and 3, but not at Week 6, of the MBSR program for caregivers (C). In addition, although not as consistent as the cortisol results, caregivers showed the largest reduction in IL-6 levels from pre- to post-MBSR(C) session in Week 1, and patients had lower IL-6 levels at Week 6 compared to Week 1 (Lengacher et al., 2012). In some studies of BCS, researchers have reported evidence of MBSR-related improvement in cortisol and/or IL-6 levels (Matchim, Armer, & Stewart, 2011; Matousek, Pruessner, & Dobkin, 2011; Witek-Janusek et al., 2008). There were no observed main effects of MBSR in a randomized trial among patients with various types of cancer, however investigators did observe a moderating effect on awakening cortisol levels (Branstrom, Kvillemo, & Akerstedt, 2013).
Although cortisol and IL-6 are considered to be physiological markers for stress, few BC studies have examined the relationships between these biomarkers and symptoms. Matousek, Pruessner, and Dobkin (2011) found no significant relationships between cortisol levels and perceived stress, depression or medical symptoms in women who had completed treatment for BC. Similarly, neither Branstrom, Kvillemo, and Akerstedt (2013) nor Carlson et al. (2007) found evidence of significant relationships between psychological variables and cortisol levels in cancer patients. Carlson et al. (2007), however, did report a relationship between cortisol level and quality of life. Current evidence, therefore, appears inconclusive for determining whether cortisol and IL-6 can be used as objective markers for stress in BC patients. Limited rigor evident in research trial design and small effect sizes may explain some of the mixed results.
The purpose of the present study, as part of a large randomized trial, was to evaluate the efficacy of MBSR for BC compared to a usual-care control treatment in reducing levels of a stress hormone measure (cortisol) and cytokine measure of immune function (IL-6). We hypothesized the following: (1) Within-group reductions in cortisol and IL-6 would occur from pre- to postclass delivery of the MBSR(BC) program, (2) greater reductions would occur at 6 weeks in cortisol and IL-6 levels among patients assigned to the MBSR(BC) program compared to usual care, and (3) the levels of the stress hormone cortisol and cytokine IL-6 would have positive associations with self-reported psychological and physical symptoms and negative associations with health-related quality of life.
Method
Participants
Participants were recruited from the Moffitt Cancer Center and the Morsani clinics at the University of South Florida, located in Tampa, FL. Eligibility requirements for participation included: (1) female sex; (2) age ≥ 21 years; (3) a diagnosis of Stage 0, I, II, or III BC; (4) treatment with a lumpectomy and/or mastectomy; (5) completion of adjuvant radiation and/or chemotherapy at least 2 weeks prior to enrollment and within 2 years from end of primary treatment; and (6) the ability to read and speak English at an eighth-grade level. Exclusion criteria included: (1) diagnosis of Stage IV cancer, (2) a severe current psychiatric diagnosis, and (3) a cancer recurrence.
Procedures
The Scientific Review Committee at the H. Lee Moffitt Cancer Center and Research Institute and the Institutional Review Board at the University of South Florida reviewed and approved the study protocol.
Study design and randomization
A two-armed randomized controlled trial design was implemented with BCS randomly assigned in a 1:1 ratio to (1) a 6-week formal (in-class) MBSR(BC) program, which began within 1 week of the baseline assessment visit or (2) usual care. Randomization was stratified by type of surgery (lumpectomy vs. mastectomy), adjuvant BC treatment (chemotherapy with or without radiation vs. radiation alone), and stage of BC (Stage 0/I vs. II/III). A stratified block randomization scheme was employed to equally distribute baseline characteristics between groups.
Recruitment and data-collection procedures
Written informed consent was obtained prior to randomization to either the MBSR(BC) or usual-care group at a baseline orientation visit. During the orientation visit, demographic information, clinical history, measures of psychological and physical symptoms, and quality of life were collected in both groups along with saliva specimens.
Intervention procedures: MBSR(BC)
The first author (C.L.) adapted the MBSR(BC) program from the MBSR program developed by Jon Kabat-Zinn (Kabat-Zinn, Lipworth, & Burney, 1985; Kabat-Zinn et al., 1992). She modified the original 8-week Kabat-Zinn MBSR program to a 6-week program to attend to the specific needs, symptoms, and concerns associated with BC survivorship (e.g., anxiety, depression, fear of recurrence, pain, and sleep disturbances). BCS learn skills that allow them to take an active role in symptom management and stress reduction through the self-regulatory process of meditation. The modified MBSR(BC) consists of (1) educational material related to relaxation, meditation, the mind–body connection, and a healthy lifestyle for BCS; (2) practice of meditation in group meetings and homework assignments; and (3) group processes related to barriers to the practice of meditation, application of mindfulness in daily situations, and supportive group interaction (Speca, Carlson, Goodey, & Angen, 2000).
During the 6 weekly 2-hr sessions, a psychologist trained in MBSR(BC) led participants (1) sitting meditation (an awareness of the body, thoughts, and emotions while focusing on attention on breathing), (2) body scan (observing any sensations from the head to the toes while focusing attention on breathing), (3) gentle Hatha yoga (a range of postures and stretching thought to increase awareness and balance), and (4) walking meditation (enhanced awareness while walking). Participants were asked to formally meditate for at least 15–45 min per day and to use informal practice (awareness of and attention to being mindful of everyday activities and events) for at least 15–45 min per day. Participants were provided with manuals containing CDs of the guided mindfulness exercises and daily diaries to record formal and informal practice times during the 6-week intervention period and after the intervention for another 6-week period.
Intervention fidelity
To maintain the reliability of the intervention, we developed a training manual. At each weekly session, a single research assistant recorded the timing of the intervention content and activities and completed a survey rating the quality for that session on an observational fidelity checklist. The principal investigator (PI) and research assistants evaluated the observational fidelity checklist as well as the patient diaries monthly for fidelity to the intervention.
Usual-care control
Usual care consisted of standard posttreatment clinic visits. Participants in the usual-care group were asked to refrain from practicing meditation, using yoga techniques, or participating in MBSR(BC) for the duration of the 12-week study. Members of the usual-care group were wait-listed to receive the MBSR(BC) intervention within 6 months after study enrollment.
Measures
Cortisol and IL-6 levels
At baseline and 6 weeks, saliva specimens were collected for both the MBSR(BC) and usual-care groups. All samples were collected in the morning at the same time of day. For the MBSR(BC) group, saliva was also collected 20 min prior to and 20 min after the MBSR(BC) intervention session during Weeks 1 and 6. Saliva was collected using the drool method, in which participants were asked to drool into 50-ml conical Falcon tubes over 5 min without coughing or clearing their throats. Samples were transferred to 15-ml conicals, then centrifuged at 3,000 rpm for 15 min; supernatants were pipetted into Fisherbrand™ siliconized/low-retention microcentrifuge tubes (Fisher Scientific) and stored at −80°C in the University of South Florida College of Nursing. For measurement of cortisol, saliva was assayed using a High-Sensitivity Salivary Cortisol Enzyme Immunoassay Kit from Salimetrics, Inc. Intra-assay coefficients of variation, inter-assay values, and assay sensitivity were calculated, and cortisol values were examined for outliers, with any raw data that fell outside the physiological range being excluded from the analyses. For measurement of IL-6, saliva was assayed using a high-sensitivity IL-6 ELISA kit (ABCom). As with cortisol, IL-6 values were examined for outliers, and raw data that fell outside the physiological range were excluded from analysis. Prior studies provide evidence supporting the use of salivary, as opposed to serum, IL-6. Salivary IL-6 has been found to relate more quickly to a stress response than serum or blood-based cytokines (Minetto et al., 2007; Minetto et al., 2005; Slavish, Graham-Engelnad, Smyth, & Engeland, 2015).
Psychological, Physical, and Quality of Life Measures
Fear of cancer recurrence
The Concerns About Recurrence Scale (CAR-S) was used to measure fear of cancer recurrence (Vickberg, 2003). The CAR-S comprises 30 items measured on a Likert-type scale. The instrument is divided into two sections, the first of which assesses the extent of worry related to recurrence, while the second assesses the nature of the concerns related to recurrence. The scale has good internal consistency reliability (0.87) for BCS (Vickberg, 2003).
Depression
To measure depression, the Center for Epidemiological Studies Depression (CES-D) Scale, a 20-item measure of depressive symptomatology (Radloff, 1977), was used. Participants rated how frequently they experienced each depressive symptom during the previous week on a four-point scale from 0 (rarely or none of the time) to 3 (most or all of the time). Higher scores are associated with more depressive symptoms. The CES-D instrument is widely used in cancer research with a reported α coefficient of >.85 among BC patients (D. Hann, Winter, & Jacobsen, 1999) and 0.92 in the general population (Radloff, 1977).
Anxiety
To measure state anxiety in study participants, the State-Trait Anxiety Inventory was used (Spielberger, Gorsuch, & Luschene, 1983). The State Anxiety subscale includes 20 items and measures state anxiety on a Likert-type scale ranging from 1 (not at all) to 4 (very much so). Higher scores are indicative of greater anxiety. The tool has high internal reliability (0.95; Spielberger et al., 1983).
Perceived stress
To measure perceived stress, the 14-item Perceived Stress Scale was used (Cohen, Kamarck, & Mermelstein, 1983). Items are rated on a Likert-type scale and assess how often in the past month respondents appraised life situations as “stressful.” Higher scores demonstrate a greater level of perceived stress. Internal consistency reliability has ranged from 0.84 to 0.86 (Cohen et al., 1983).
Sleep quality
The 19-item Pittsburgh Sleep Quality Index (PSQI; Carpenter & Andrykowski, 1998), which measures subjective sleep parameters and quantity of sleep based on the participant’s recall of sleep patterns and behaviors during the past month, was used to measure sleep quality. Specifically, the PSQI measures seven domains of sleep: quality, latency, duration, efficiency, disturbances, use of sleep medications, and daytime sleep function. Reported reliability of the PSQI ranges from 0.70 to 0.78 for sleep disturbance (Carpenter & Andrykowski, 1998).
Fatigue
The 14-item Fatigue Symptom Inventory assesses the perceived severity and frequency of fatigue as well as the degree to which it interferes with daily functioning (D. M. Hann et al., 1998). Respondents rate the severity of their fatigue on a scale from 0 (not all fatigued) to 10 (as fatigued as I could be). For perceived interference with daily activities, respondents rate the effect of fatigue on various activities on a scale from 0 (no inference) to 10 (extreme interference). For perceived frequency, respondents indicate the number of days in the past week (i.e., 0–7 days) during which they felt fatigued and the portion of the days for which they felt fatigued (0 [none of the day] to 10 [the entire day]). The 7-item interference scale has good internal consistency, with α coefficients above 0.90 (D. M. Hann et al., 1998).
Quality of life
The 36-Item Medical Outcomes Studies Short-Form General Health Survey was used to measure health-related quality of life, with items rated on a Likert-type scale (Ware, Snow, Kosinski, & Gandek, 1993). This 8-item self-report measure assesses physical functioning, physical role functioning, bodily pain, general health, vitality, social functioning, emotional role functioning, and mental health. Reliability estimates have been reported in several studies with several different patient populations. Estimated internal consistency reliability ranges from 0.62 to 0.94, although the majority of estimates exceeded 0.80. Factor analysis has indicated that two dimensions of the instrument, physical and mental health status, account for 82% of the reliable variance of the measure (Ware et al., 1993).
Demographic data and clinical history
The demographic data collected included age, ethnicity, educational achievement, marital status, income, and employment status. Medical history data included cancer type, date of cancer diagnosis, and treatments received for BC. We collected these data at baseline and then reviewed and updated them at 6 weeks.
Statistical Methods
Percentages were used to describe baseline demographic categorical variables, and χ2 tests were used to compare them. The one continuous demographic variable, age, was described using mean and standard deviation (SD) and compared between groups using Student’s t test.
To test the first hypothesis, the Wilcoxon-signed ranks test was used to evaluate whether there were immediate within-group differences in the levels of cortisol and cytokine IL-6 from pre- to post-MBSR(BC) sessions at Weeks 1 and 6.
For the second hypothesis, linear mixed models were used to assess whether BCS enrolled in the MBSR(BC) program experienced greater reductions from baseline to 6 weeks in levels of cortisol and IL-6 compared to the usual-care group. Cortisol and IL-6 levels from baseline were log-transformed to meet the normality assumption of linear mixed models. To determine the magnitude of the change, within-group effect sizes were calculated using Cohen’s d.
To test the hypothesis that cortisol and IL-6 levels would be positively related to symptoms and negatively related to quality of life, Spearman correlations were used. Correlations were examined at baseline and at 6 weeks after the MBSR(BC) program to assess consistency across time. Observing consistent correlations at these two time points enhances confidence in reproducibility.
Results
Participant Characteristics
Of the 322 BCS initially enrolled (167 MBSR[BC] and 155 usual care) in the study, 299 completed the baseline and 6-week assessments (152 MBSR[BC] and 147 usual care), yielding a 9% attrition rate. Refer to Lengacher et al. (2016) to view the CONSORT chart showing the number of participants screened, randomized, and retained. Table 1 depicts the demographic characteristics of the final sample (N = 322) by random assignment. The mean age for the sample was 56.6 years (±9.7 SD). The majority of participants were White non-Hispanic (69.4%) and married (64.4%), and a large minority comprised college graduates (43.6%). We observed no statistically significant differences on clinical characteristics between groups at baseline, with the majority diagnosed with either Stage I (33.8%) or Stage II (35.7%) BC. All BCS received either a lumpectomy (46.6%) or mastectomy (53.4%). A combination of chemotherapy and radiation was the most frequent treatment (35.7%), followed by radiation alone (29.2%) and chemotherapy alone (13%).
Table 1.
Demographic Characteristics of Participants.
| Characteristic | All (N = 322) | UC (n = 155) | MBSR(BC; n = 167) | p Value |
|---|---|---|---|---|
| Age in years (mean ± SD) | 56.6 ± 9.7 | 57.6 ± 9.2 | 56.5 ± 10.2 | .80 |
| Race/ethnicity (% [n]) | .88 | |||
| White non-Hispanic | 69.4 (222) | 71.9 (110) | 67.1 (112) | |
| Black non-Hispanic | 11.6 (37) | 10.5 (16) | 12.6 (21) | |
| Hispanic | 10.3 (33) | 9.1 (14) | 11.4 (19) | |
| Other single race/ethnicity | 3.7 (12) | 3.3 (5) | 4.2 (7) | |
| More than one race/ethnicity reported | 5.0 (16) | 5.2 (8) | 4.8 (8) | |
| Marital status (% [n]) | .65 | |||
| Married | 64.4 (206) | 66.7 (102) | 62.3 (104) | |
| Single | 9.4 (30) | 9.1 (14) | 9.6 (16) | |
| Widowed | 11.2 (36) | 11.8 (18) | 10.8 (18) | |
| Divorced | 15.0 (48) | 12.4 (19) | 17.4 (29) | |
| Highest level of education (% [n]) | .78a | |||
| High school or less | 17.8 (57) | 17.5 (27) | 18.0 (30) | |
| Some college or vocational | 38.6 (124) | 40.3 (62) | 37.1 (62) | |
| College graduate and above | 43.6 (140) | 42.2 (65) | 44.9 (75) | |
| Current employment status (% [n]) | .64 | |||
| Employed >32 hr/week | 26.3 (84) | 28.8 (44) | 23.9 (40) | |
| Employed <32 hr/week | 11.9 (38) | 13.7 (21) | 10.2 (17) | |
| Retired | 27.8 (89) | 26.1 (40) | 29.3 (49) | |
| Medical leave/disabled | 10.3 (33) | 9.8 (15) | 10.8 (18) | |
| Other | 23.7 (76) | 21.6 (33) | 25.8 (43) | |
| Annual income (% [n]) | .45a | |||
| <US$10,000 | 15.6 (49) | 15.2 (23) | 16.0 (26) | |
| US$10,000 to <US$20,000 | 16.2 (51) | 13.9 (21) | 18.4 (30) | |
| US$20,000 to <US$40,000 | 22.9 (72) | 24.5 (37) | 21.5 (35) | |
| US$40,000 to <US$80,000 | 24.2 (76) | 23.8 (36) | 24.5 (40) | |
| US$80,000 to <US$100,000 | 8.9 (28) | 9.3 (14) | 8.6 (14) | |
| >US$100,000 | 12.1 (38) | 13.3 (20) | 11.0 (18) |
Note. Groups were compared using χ2, except for age, which was compared using Student’s t test. MBSR(BC) = mindfulness-based stress reduction for breast cancer group; UC = usual-care group.
a p Value for linear trend.
Hypothesis 1: Immediate short-term effects of MBSR(BC) on salivary cortisol and IL-6 levels.
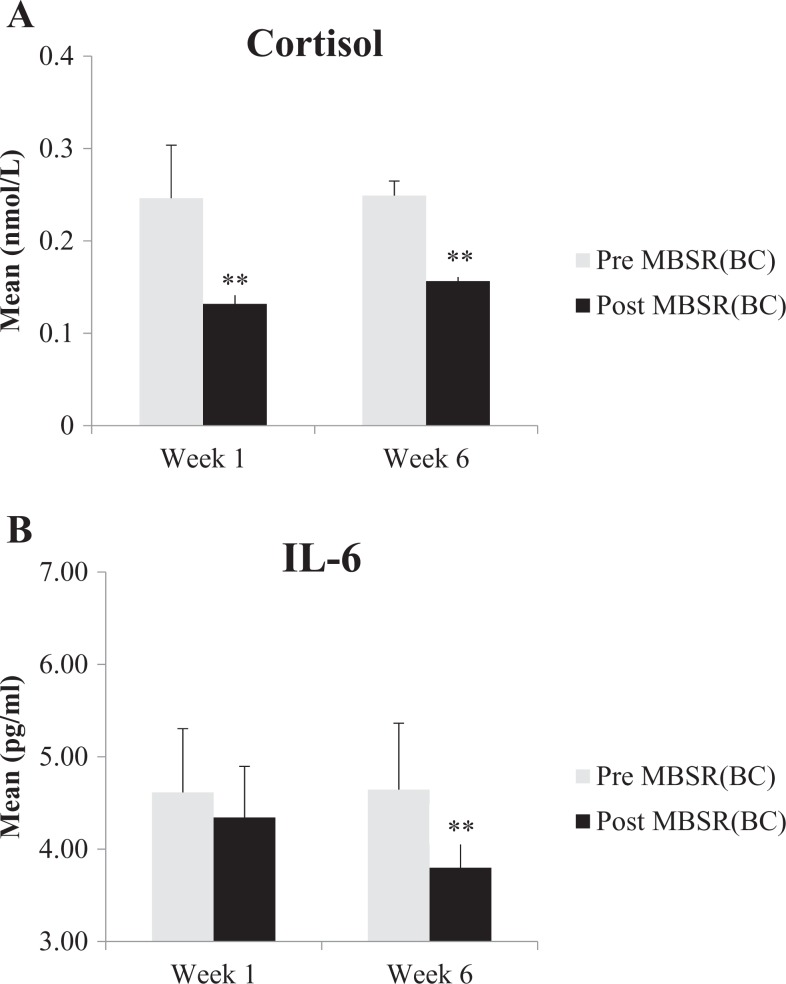
The immediate or short-term within-group effects of the MBSR(BC) program were accessed on salivary cortisol and IL-6 levels at Weeks 1 (n = 161) and 6 (n = 152) before and immediately following the MBSR(BC) intervention class. Statistically significant reductions were observed in cortisol levels from before to after the delivery of the MBSR(BC) program on both weeks. These differences had medium effect sizes at both the Weeks 1 (Cohen’s d = .52) and 6 (d = .56) time points (p < .01). There was a statistically significant reduction in IL-6 levels (p < .01) from before to after the delivery of the program at Week 6 only, and the within-group effect size was smaller than that for cortisol (d = 0.21). Figure 1a and b displays the within-group short-term effects of the program on these biomarkers. Our data supported our hypothesis.
Figure 1.
Mean (A) cortisol and (B) IL-6 levels before and after delivery of the MBSR(BC) program on Weeks 1 and 6. Mean values were compared between pre- and postsession using the Wilcoxon-signed ranks test. IL-6 = interleukin-6; MBSR(BC) = mindfulness-based stress reduction for breast cancer. **p < .01.
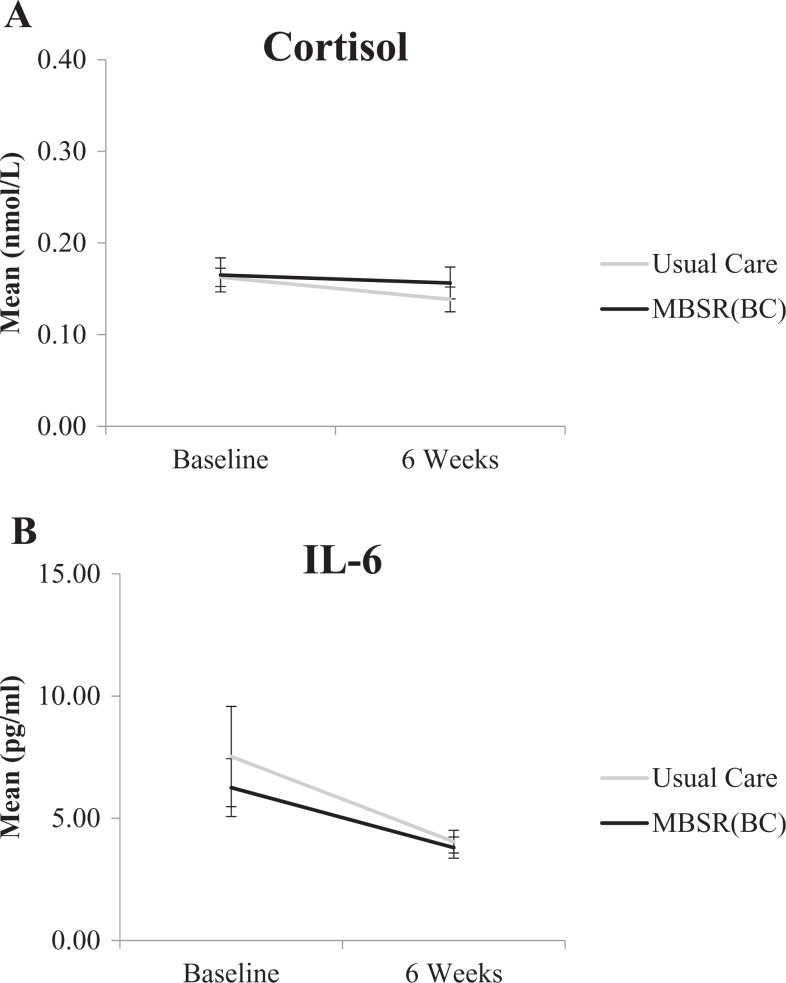
Hypothesis 2: Long-term effects of MBSR(BC) on salivary cortisol and IL-6 levels.
The between-group effects of MBSR(BC) compared to usual care on salivary cortisol and IL-6 levels using linear mixed models to compare changes in levels was assessed from baseline orientation to the postassessment 6-week time point. Results showed a nonsignificant difference in change in cortisol levels between the MBSR(BC) and usual-care groups over time (p = .48). Additionally, no significant differences between the MBSR(BC) and usual-care groups were observed for change over time in IL-6 levels (p = .76). Our findings did not support this hypothesis. Figure 2a and b displays the between-group effects of MBSR(BC) compared to usual care on salivary cortisol and IL-6.
Figure 2.
Figures 2a and 2b. Mean cortisol and IL-6 levels at Baseline and 6 weeks by experimental condition. The slope of each experimental condition was compared using linear mixed models.
Hypothesis 3: Associations between levels of cortisol and IL-6 and psychological and physical symptoms and quality of life.
At baseline among all patients, no statistically significant relationships between levels of cortisol and symptoms were observed (see Table 2). In contrast, we observed statistically significant positive relationships between levels of IL-6 and the following symptoms: (1) concerns about recurrence, overall (r = .13, p < .05), and recurrence problems (r = .14, p < .05); (2) fatigue severity (r = .13, p < .05); and (3) sleep disturbances (r = .13, p < .05) and global sleep (r = .14, p < .05). Significant negative associations were oberved between IL-6 levels and the Quality of Life subscales of general health (r = −.17, p < .01), physical health (r = −.17, p < .01), and pain (r = −.16, p < .01).
Table 2.
Correlations Between the Potential Stress Biomarkers Cortisol and Interleukin-6 (IL-6) and Symptoms and Quality of Life (QOL) at Baseline (All Participants) and 6 Weeks (MBSR Only).
| Cortisol (r) | IL-6 (r) | |||
|---|---|---|---|---|
| Symptom or QOL Variable | Baseline (n = 320) | 6 Weeks (n = 153) | Baseline (n = 262) | 6 Weeks (n = 123) |
| Center for Epidemiologic Studies Depression Scale | .01** | .11** | .07** | .20** |
| State-Trait Anxiety Inventory | .03** | .08** | .06** | .11 |
| Perceived Stress Scale | .01** | .17** | .08** | .19** |
| Concerns About Reoccurrence Scale | ||||
| All | −.08** | .08** | .13** | .09 |
| Problems | −.10** | .10** | .14** | .09 |
| Fatigue Symptom Inventory | ||||
| Severity | −.06** | .09** | .13** | .16* |
| Interference | −.07** | .13** | .11** | .17** |
| Brief Pain Inventory | ||||
| Severity | −.02** | .02** | .16** | .20** |
| Interference | −.04** | .02** | .16** | .20** |
| Pittsburgh Sleep Quality Index | ||||
| Duration | −.07** | .10** | .08** | .11 |
| Disturbances | −.07** | .05** | .13** | .22** |
| Latency | −.04** | .15** | .10** | .23** |
| Daytime sleep function | .02** | .00** | .05** | .10 |
| Efficiency | −.10** | .16** | .09** | .08 |
| Global | −.03** | .15** | .14** | .23** |
| Medical Outcomes Studies Short-Form (QOL) | ||||
| Physical functioning | −.01** | −.05** | −.10** | −.16* |
| Role limitations due to physical health | −.01** | .02** | .08** | .21** |
| Role limitations due to mental health | −.04** | .07** | .07** | .20** |
| Energy/fatigue | .10** | −.08** | −.11** | −.16* |
| Emotional well-being | .02** | −.13** | .00** | −.11 |
| Social functioning | .05** | −.07** | −.10** | −.19** |
| General health | .01** | −.10** | −.17** | −.18** |
| Physical health | .02** | −.08** | −.17** | −.15* |
| Mental health | .05** | −.05** | −.01** | −.00 |
| Pain | .04** | −.02** | −.16** | −.26** |
Note. MBSR = mindfulness-based stress reduction.
*p < .05. **p < .01.
After the 6-week MBSR(BC) program, additional significant positive relationships were observed in the intervention group between levels of cortisol and the following symptoms (see Table 2): (1) perceived stress (r = .17, p < .01); (2) fatigue interference (r = .13, p < .05); and (3) sleep latency (r = .15, p < .01), sleep efficiency (r = .16, p < .01), and global sleep (r = .15, p < .05). A significant negative association was found between cortisol and the Quality of Life subscale emotional well-being (r = −.13, p < .05). For IL-6 levels among the MBSR(BC) participants at 6 weeks, significant positive associations were observed with the following symptoms: (1) depression (r = .20, p < .01); (2) perceived stress (r = .19, p < .01); (3) fatigue severity (r = .16, p < .05) and fatigue interference (r = .17, p < .01); (4) pain severity (r = .20, p < .01) and pain interference (r = .20, p < .01); and (5) sleep disturbances (r = .22, p < .01), sleep latency (r = .23, p < .01), and global sleep (r = .23, p < .01). Significant negative associations were found between levels of IL-6 and the Quality of Life subscales of physical functioning (r = −.16, p < .01), energy/fatigue (r = −.16, p < .05), social functioning (r = −.19, p < .01), general health (r = −.18, p < .01), physical health (r = −.15, p < .05), and pain (r = −.26, p < .01). Significant positive correlations were identified between IL-6 levels and the Quality of Life subscales of role limitations due to physical health (r = .21, p < .01) and role limitations due to mental health (r = .20, p < .01).
Due to the multiple correlation coefficients calculated (increasing the possibility of Type I error), we examined the consistency in correlations across the two time points. No statistically significant correlations were repeated for cortisol, decreasing our confidence that these observations could be reproduced. The correlations that were statistically significant for IL-6 across both time points included those with fatigue severity, pain severity and interference, sleep disturbances, global sleep, general health, physical health, and pain. Thus, our evidence supports Hypothesis 3 for IL-6 but not for cortisol.
Discussion
To our knowledge, this study is the largest clinical trial to evaluate the effects of MBSR(BC) on the stress hormone cortisol and pro-inflammatory cytokine IL-6 among BCS to date. Our results support previous findings that physiological changes occur during MBSR(BC) sessions among BCS (Lengacher et al., 2012). Due to the stress-reducing effects of the MBSR(BC) intervention, we hypothesized that we would see immediate reductions in levels of cortisol and IL-6 from pre- to post-MBSR(BC) session and that these pre- to postintervention reductions would be sustained over the 6-week time period of the MBSR(BC) intervention. We also hypothesized that cortisol and IL-6 levels would be associated with self-reports of psychological and physical symptoms and quality of life.
Our findings partially supported our study hypotheses. When we examined the immediate effects of MBSR(BC) on cortisol and IL-6 levels within the MBSR(BC) group, we observed statistically significant reductions with medium effect sizes in cortisol levels pre- to post-MBSR(BC) session at Weeks 1 and 6. These results suggest that participation in the MBSR(BC) sessions immediately reduces salivary cortisol levels but does not indicate how long the reduction persists after the session. In addition, we observed a reduction in IL-6 levels from pre- to post-MBSR(BC) session at Week 6 with a small effect size, suggesting that MBSR(BC) may reduce salivary IL-6 salivary levels among BCS, at least temporarily.
Findings, however, did not support our second hypothesis, that BCS enrolled in the MBSR(BC) program would experience sustained reductions from baseline to 6 weeks in their cortisol and IL-6 levels when compared to the usual-care group. Although researchers have found salivary IL-6 to be a reliable marker of acute stress (Slavish et al., 2015), evidence shows that its levels peak almost immediately after a stress exposure, whereas plasma levels of IL-6 demonstrate a lag (Minetto et al., 2005). Our immediate results for pre- and postsession IL-6 measures for the intervention group at Weeks 1 and 6 show that the MBSR(BC) intervention reduced IL-6, thus reducing the stress effect. Due to the less invasive nature of the measurement of salivary IL-6 compared to plasma IL-6, researchers should continue to explore this method of cytokine collection in future research; however, more work needs to be done to assess the effectiveness of the use of salivary IL-6 as a measure of stress under varying conditions and across different collection periods (Slavish et al., 2015).
The results of previous studies that assessed cortisol as a marker for improvement in stress levels in cancer patients in response to MBSR are varied. Although Branstrom et al. (2013) found no overall effects of MBSR on cortisol levels, they did note a significant moderation effect in which intervention effects on awakening cortisol were contingent on baseline cortisol levels. Our results in the present study regarding short-term effects of MBSR are consistent with those of Matchim, Armer, and Stewart (2011), who reported a significant decrease in morning cortisol levels immediately after an MBSR intervention among BCS. Regarding longer term effects of the intervention on cortisol levels, our results differed from those of Witek-Janusek et al. (2008), who found that plasma cortisol levels decreased compared to the control group following an 8-week MBSR intervention, and of Carlson et al. (2007), who, also found no significant changes in cortisol levels over time, however did find that those with initially high cortisol levels showed a significant decrease compared to those with lower levels. By contrast, in a meta-analysis, O’Leary, O’Neill, and Dockray (2016) reported that randomized clinical trials have not yielded statistically significant evidence of long-term cortisol reductions in response to MBSR, which is consistent with our finding in the present study.
There is very limited evidence regarding the effects of MBSR on the stress biomarker IL-6 among cancer survivors. The few studies that examined this relationship have had mixed results, with some reporting significant changes in IL-6 levels over time (Gallegos et al., 2015; Lengacher et al., 2012; Witek-Janusek et al., 2008) and others, including the current study, reporting no long-term change (Creswell et al., 2012).
Evidence from the present study supported our third hypothesis, of relationships between the biomarkers and symptoms and quality of life, for IL-6 but not cortisol. The literature provides evidence that increased levels of both IL-6 and cortisol are associated with negative outcomes such as depression, anxiety, and sleep disorders (Lutgendorf et al., 2008; Rohleder et al., 2012). Although we did observe some isolated statistically significant relationships between symptoms and salivary cortisol, we are most confident in the reproducibility of the IL-6 correlations because they were consistent across time points. Specifically, we found positive, though weak, correlations between IL-6 and the physical symptoms fatigue, sleep, and pain along with worse physical and general health. By contrast, previous studies have found moderate positive correlations between IL-6 and anxiety and depression (Bossola et al., 2010) and moderate negative correlations between IL-6 and fatigue (Bossola, Di Stasio, Giungi, Rosa, & Tazza, 2015) in hemodialysis patients
The present study is not without limitations. Although internal validity of the study was strong due to the study design (randomized controlled trial), the addition of an active-attention group could have provided a more informative comparison for the MBSR(BC) intervention group. For future work, researchers should consider designing multi-arm randomized controlled trials with an active-attention control group alongside a usual-care control group to investigate the effects of time and attention on participant outcomes. The study sample was largely educated with some diversity but did not include non-English speaking participants. Even though we asked participants in the usual-care group to abstain from participating in meditation/mindfulness programs during the study period, we did not formally monitor compliance with this request. Lastly, the lack of extended follow-up is a limitation. MBSR(BC) is a nonpharmacological skill-based intervention that is learned and practiced over time. Long-term follow-up is needed in future research to determine the impact of continued mindfulness practice on biological markers of psychological and physiological symptoms resulting from BC treatment and recovery.
In summary, research has shown that MBSR is an effective intervention for reducing adverse psychological and physiological symptoms associated with cancer diagnosis or treatment among BCS (e.g., Henderson et al., 2012; Hoffman et al., 2012; Lengacher et al., 2009; Lengacher et al., 2016). The present study contributes to the biological evidence of the short-term effectiveness of MBSR(BC) on the objective markers of a stress hormone and an inflammatory cytokine. This body of research as a whole contributes to nursing research and practice by demonstrating that an alternative, nonpharmacological intervention can alleviate the stress response in the short term for BCS, providing more options for clinical interventions. Continued investigation is needed to determine the role of MBSR in affecting levels of the potentially deleterious stress hormones cortisol and IL-6.
Footnotes
Authors' Note: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. This study protocol was approved by the Institutional Review Board at the University of South Florida to ensure the ethical treatment of participants.
Author Contributions: Cecile A. Lengacher contributed to conception, design, acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Richard R. Reich contributed to conception, design, acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Carly L. Paterson contributed to analysis, drafted the manuscript critically, revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Melissa Shelton contributed to conception, analysis, and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Steve Shivers contributed to conception, analysis, and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Sophia Ramesar contributed to acquisition and analysis, drafted the manuscript, critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Michelle L. Pleasant contributed to interpretation, drafted the manuscript, critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Pinky Budhrani-Shani contributed to conception, acquisition, and analysis; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Maureen Groer contributed to acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Tiffany A. Romershausen contributed to interpretation, critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Janice Post-White, Versie Johnson-Mallard, and Bradley Kane, contributed to the conception, analysis, and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Lakeshia Cousin, Manolete S. Moscoso, and Jong Y. Park contributed to the interpretation, critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by National Cancer Institute Award No. 1R01CA131080-01A2. The work contained within this publication was supported in part by the Survey Methods Core Facility and the Biostatistics Core Facility at the H. Lee Moffitt Cancer Center & Research Institute.
ORCID iD: Janice Post-White  http://orcid.org/0000-0001-5472-5670
http://orcid.org/0000-0001-5472-5670
References
- Abercrombie H. C., Giese-Davis J., Sephton S. E., Epel E. S., Turner-Cobb J. M. (2004). Flattened cortisol rhythms in metastatic breast cancer patients. Psychoneuroendocrinology, 29, 1082–1092. doi:10.1016/j.psyneuen.2003.11.003 [DOI] [PubMed] [Google Scholar]
- American Cancer Society. (2017). Cancer facts & figures 2017. Atlanta, Georgia: Author; Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf [Google Scholar]
- Baer R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. doi:10.1093/clipsy/bpg015 [Google Scholar]
- Bishop S. R., Lau M., Shapiro S., Carlson L., Anderson N. D., Carmody J.…Devins G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology Science and Practice, 11, 230–241. doi:10.1093/clipsy/bph077 [Google Scholar]
- Bossola M., Ciccarelli C., Di Stasio E., Conte G. L., Vulpio C., Luciani G., Tazza L. (2010). Correlates of symptoms of depression and anxiety in chronic hemodialysis patients. General Hospital Psychiatry, 32, 125–131. doi:10.1016/j.genhosppsych.2009.10.009 [DOI] [PubMed] [Google Scholar]
- Bossola M., Di Stasio E., Giungi S., Rosa F., Tazza L. (2015). Fatigue is associated with serum interleukin-6 levels and symptoms of depression in patients on chronic hemodialysis. Journal of Pain and Symptom Management, 49, 578–585. doi:10.1016/j.jpainsymman.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Branstrom R., Kvillemo P., Akerstedt T. (2013). Effects of mindfulness training on levels of cortisol in cancer patients. Psychosomatics, 54, 158–164. doi:10.1016/j.psym.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Carlson L. E., Speca M., Faris P., Patel K. D. (2007). One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain, Behavior, and Immunity, 21, 1038–1049. doi:10.1016/j.bbi.2007.04.002 [DOI] [PubMed] [Google Scholar]
- Carpenter J. S., Andrykowski M. A. (1998). Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research, 45, 5–13. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Creswell J. D., Irwin M. R., Burklund L. J., Lieberman M. D., Arevalo J. M. G., Ma J., Cole S. W. (2012). Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain, Behavior, and Immunity, 26, 1095–1101. doi:10.1016/j.bbi.2012.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallegos A. M., Lytle M. C., Moynihan J. A., Talbot N. L. (2015). Mindfulness-based stress reduction to enhance psychological functioning and improve inflammatory biomarkers in trauma-exposed women: A pilot study. Psychological Trauma, 7, 525–532. doi:10.1037/tra0000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hann D., Winter K., Jacobsen P. (1999). Measurement of depressive symptoms in cancer patients. Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychosomatic Research, 46, 437–443. [DOI] [PubMed] [Google Scholar]
- Hann D. M., Jacobsen P. B., Azzarello L. M., Martin S. C., Curran S. L., Fields K. K.…Lyman G. (1998). Measurement of fatigue in cancer patients: Development and validation of the Fatigue Symptom Inventory. Quality of Life Research, 7, 301–310. [DOI] [PubMed] [Google Scholar]
- Henderson V., Clemow L., Massion A., Hurley T., Druker S., Hebert J. R. (2012). The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: A randomized trial. Breast Cancer Research and Treatment, 131, 99–109. doi:10.1007/s10549-011-1738-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman C., Ersser S., Hopkinson J., Nicholls P., Harrington J., Thomas P. (2012). An RCT evaluating of mindfulness-based stress reduction in mood, breast- and endocrine-related quality-of-life and wellbeing in Stages 0 to III breast cancer. Paper presented at the British Psychosocial 2012 Conference, Leeds, England Abstract retrieved from Psycho-Oncology, 21, 1. [Google Scholar]
- Kabat-Zinn J., Lipworth L., Burney R. (1985). The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8, 163–190. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J., Massion A. O., Kristeller J., Peterson L. G., Fletcher K. E., Pbert L.…Santorelli S. F. (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry, 149, 936–943. [DOI] [PubMed] [Google Scholar]
- Lengacher C. A., Johnson-Mallard V., Post-White J., Moscoso M. S., Jacobsen P. B., Klein T. W.…Kip K. E. (2009). Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology, 18, 1261–1272. doi:10.1002/pon.1529 [DOI] [PubMed] [Google Scholar]
- Lengacher C. A., Kip K. E., Barta M., Post-White J., Jacobsen P. B., Groer M.…Shelton M. M. (2012). A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. Journal of Holistic Nursing, 30, 170–185. doi:10.1177/0898010111435949 [DOI] [PubMed] [Google Scholar]
- Lengacher C. A., Reich R. R., Paterson C. L., Jim H. S., Ramesar S., Alinat C. B.…Kip K. E. (2015). The effects of mindfulness-based stress reduction on objective and subjective sleep parameters in women with breast cancer: A randomized controlled trial. Psycho-Oncology, 24, 424–432. doi:10.1002/pon.3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengacher C. A., Reich R. R., Paterson C. L., Ramesar S., Park J. Y., Alinat C. B.…Miladinovic B. (2016). Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: A randomized controlled trial. Journal of Clinical Oncology, 34, 2827–2834. doi:10.1200/JCO.2015.65.7874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutgendorf S. K., Weinrib A. Z., Penedo F., Russell D., DeGeest K., Costanzo E. S.…Lubaroff D. M. (2008). Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. Journal of Clinical Oncology, 26, 4820–4827. doi:10.1200/JCO.2007.14.1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matchim Y., Armer J. M., Stewart B. R. (2011). Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. Western Journal of Nursing Research, 33, 996–1016. doi:10.1177/0193945910385363 [DOI] [PubMed] [Google Scholar]
- Matousek R. H., Pruessner J. C., Dobkin P. L. (2011). Changes in the cortisol awakening response (CAR) following participation in mindfulness-based stress reduction in women who completed treatment for breast cancer. Complementary Therapies in Clinical Practice, 17, 65–70. doi:10.1016/j.ctcp.2010.10.005 [DOI] [PubMed] [Google Scholar]
- McEwen B. S. (1998). Protective and damaging effects of stress mediators. Journal of Medicine, 338, 171–179. doi:10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- McEwen B. S. (2000). The neurobiology of stress: From serendipity to clinical relevance. Brain Research, 886, 172–187. [DOI] [PubMed] [Google Scholar]
- McEwen B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87, 873–904. doi:10.1152/physrev.00041.2006 [DOI] [PubMed] [Google Scholar]
- McGregor B. A., Antoni M. H. (2009). Psychological intervention and health outcomes among women treated for breast cancer: A review of stress pathways and biological mediators. Brain, Behavior and Immunity, 23, 159–166. doi:10.1016/j.bbi.2008.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minetto M., Gazzoni M., Lanfranco F., Baldi M., Saba L., Pedrola R.…Rainoldi A. (2007). Influence of the sample collection method on salivary interleukin-6 levels in resting and post-exercise conditions. European Journal of Applied Physiology, 101, 249–256. [DOI] [PubMed] [Google Scholar]
- Minetto M., Rainoldi A., Gazzoni M., Terzolo M., Borrione P., Termine A.…Paccotti P. (2005). Differential responses of serum and salivary interleukin-6 to acute strenuous exercise. European Journal of Applied Physiology, 93, 679–686. doi:10.1007/s00421-004-1241-z [DOI] [PubMed] [Google Scholar]
- O’Leary K., O’Neill S., Dockray S. (2016). A systematic review of the effects of mindfulness interventions on cortisol. Journal of Health Psychology, 21, 2108–2121. [DOI] [PubMed] [Google Scholar]
- Radloff L. (1977). The CES-D scale: A self-report depression scale for researching the general population. Application of Psychological Measures, 1, 385–401. [Google Scholar]
- Rohleder N., Aringer M., Boentert M. (2012). Role of interleukin-6 in stress, sleep, and fatigue. Annals of the New York Academy of Sciences, 1261, 88–96. doi:10.1111/j.1749-6632.2012.06634 [DOI] [PubMed] [Google Scholar]
- Saboonchi F., Petersson L. M., Weenman-Larsen A., Alexanderson K., Vaez M. (2015). Trajectories of anxiety among women with breast cancer: A proxy for adjustment from acute to transitional survivorship. Journal of Psychological Oncology, 33, 603–619. doi:10.1080/07347332.2015.1082165 [DOI] [PubMed] [Google Scholar]
- Sephton S. E., Sapolsky R. M., Kraemer H. C., Spiegel D. (2000). Diurnal cortisol rhythm as a predictor of breast cancer survival. Journal of the National Cancer Institute, 92, 994–1000. [DOI] [PubMed] [Google Scholar]
- Slavish D. C., Graham-Engelnad J. E., Smyth J. M., Engeland C. G. (2015). Salivary markers of inflammation in response to acute stress. Brain, Behavior, and Immunity, 44, 253–269. doi:10.1016/j.bbi.2014.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speca M., Carlson L. E., Goodey E., Angen M. (2000). A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Journal of Psychosomatic Medicine, 62, 613–622. [DOI] [PubMed] [Google Scholar]
- Spiegel D. (2012). Mind matters in cancer survival. Psycho-Oncology, 21, 588–593. doi:10.1002/pon.3067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C., Gorsuch R., Luschene R. (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists. [Google Scholar]
- Turner-Cobb J. M., Sephton S. E., Koopman C., Blake-Mortimer J., Spiegel D. (2000). Social support and salivary cortisol in women with metastatic breast cancer. Psychosomatic Medicine, 62, 337–345. [DOI] [PubMed] [Google Scholar]
- Vickberg S. M. (2003). The Concerns About Recurrence Scale (CARS): A systematic measure of women’s fears about the possibility of breast cancer recurrence. Annuals of Behavioral Medicine, 25, 16–24. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Snow K. K., Kosinski M., Gandek B. (1993). SF-36 survey manual and interpretation guide. Boston, MA: New England Medical Center. [Google Scholar]
- Witek-Janusek L., Albuquerque K., Chroniak K. R., Chroniak C., Durazo-Arvizu R., Mathews H. L. (2008). Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain, Behavior, and Immunity, 22, 969–981. doi:10.1016/j.bbi.2008.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurtzen H., Dalton S. O., Andersen K. K., Elsass P., Flyger H. L., Sumbundu A., Johansen C. (2013). Who participates in a randomized trial of mindfulness-based stress reduction (MBSR) after breast cancer? A study of factors associated with enrollment among Danish breast cancer patients. Psycho-Oncology, 22, 1180–1185. doi:10.1002/pon.3094 [DOI] [PubMed] [Google Scholar]