Abstract
Introduction:
Literature posits discrimination can be a barrier to racial/ethnic minorities’ healthcare use. This study examined the relationship between perceived discrimination in the form of racial microaggressions and delayed prenatal care (PNC) in African American (AA) women. It also investigated whether this relationship was modified by women’s shade of skin color owing to societal attitudes and beliefs tied to colorism (also known as skin tone bias).
Methods:
Data were from a cohort of 1,410 black/AA women in Metropolitan Detroit, Michigan, enrolled in 2009–2011 (analyzed August 2017–July 2018). Perceived racial microaggressions were assessed using the 20-item Daily Life Experiences of Racism and Bother (DLE-B) scale. Logistic regression modeled the relationship between the DLE-B and delayed PNC, defined as third trimester or no PNC entry.
Results:
Nearly a quarter (24.8%) of women had delayed PNC. Logistic regression models showed a DLE-B score above the median was associated with delayed PNC (AOR=1.31, 95% CI=1.00, 1.71). This association was moderated by self-reported maternal skin tone (interaction p=0.03). A higher DLE-B score was associated with delayed PNC among AA women at either end of the color continuum (light brown: AOR=1.64, 95% CI=1.02, 2.65; dark brown: AOR=2.30, 95% CI=1.20, 4.41), but not in the middle (medium brown women).
Conclusions:
Skin tone–based mistreatment in tandem with racial discrimination in the form of racial microaggressions may influence AA women’s use of PNC. Findings have implications related to the engagement of women of color, particularly AA women, in healthcare systems and maternal and child health programs.
INTRODUCTION
Prenatal care (PNC) remains a critical anchor in the continuum of women’s healthcare given nearly three of every four women will have at least one birth in their lifetime.1 For many women, PNC represents their first encounter with the healthcare system since childhood.1 As such, PNC presents the opportunity for healthcare providers to offer health education1–3 and identify or monitor underlying chronic medical conditions and pregnancy complications.2,4 Unfortunately, African American (AA) women’s utilization of PNC, in general, tends to be lower than whites.5
Although AA women are nearly twice as likely to suffer from pregnancy complications and multiple comorbidities, they are less apt to use healthcare post-delivery than white women.1,2 Further, at 40 deaths/100,000 live births, the maternal mortality rate for AA women is two to three times greater than that for all other racial/ethnic groups.5,6 Poor PNC utilization may be a factor associated with poorer maternal health outcomes, including the aforementioned.7,8 It is pertinent to identify factors associated with PNC use for women of color, especially AAs, as such factors can be used to inform culturally relevant engagement strategies.
In the U.S. and other multiethnic societies, race is a construct that is socially assigned to individuals often based on physical attributes and represents a social classification system that has bearing on people of color’s daily life experiences, choices, and opportunities.9–11 Literature posits racism/racial discrimination, in and outside of the healthcare setting, may inhibit minorities’ use of needed healthcare, including PNC.8–10 Experiences of racism/racial discrimination are stressful and may illicit the adoption of psychological stress responses and coping strategies (e.g., anxiety or hypervigilance) that influence the way members of marginalized groups engage or disengage with institutional environments—like health care— where discrimination, prejudice, and antagonism are perceived to occur.12,13 Empirical evidence suggests differential treatment due to race/ethnicity within the bounds of the healthcare system is associated with the underutilization of health care by people of color across a broad spectrum of services.10 Yet, few studies have examined racism situated in everyday experiences as a driver of delayed health care or unmet need.9,10,12
Another aspect of the experience of race that impacts people of color, including AAs, is colorism or skin tone bias.14,15 Colorism is a phenotype-based continuum that assigns privilege and disadvantage based upon the color of one’s skin15,16; privilege is allocated to individuals with lighter complexions and more Eurocentric features whereas disadvantage is assigned to those with darker skin tone and more Afrocentric features.15,16 Colorism is an insidious outgrowth of cultural racism—defined as conscious or subliminal beliefs in the supremacy of one group over another group that are rooted into the cultural standards of societal institutions, ideology, and everyday actions.17 Colorism is more pervasive in multiracial/multiethnic societies—like the U.S.—with histories of slavery, colonization, or globalization.15,16 For this reason, skin tone is more than a physical trait reflective of value neutral bodily differences.15 Against the backdrop of colorism and racism, the color continuum of skin tone becomes a social construct that is hierarchical in nature and laden with racial bias, stereotypes, and social standing.18
Skin tone, as a proxy for colorism, has been associated with health outcomes19–21 and access to health-promoting resources like higher education, higher income, and presumably residential segregation with preferential treatment given to lighter skin tones.22–24 Women of darker hues might be more apprehensive to seek PNC because of potential mistreatment due to skin tone and previous experiences with racial discrimination. Thus, skin tone–based mistreatment in tandem with racial discrimination may exacerbate AA women’s willingness to seek PNC and other healthcare services for themselves.
To address the aforementioned knowledge gap, this study examines the relationship between perceived experiences of racial discrimination in the form of racial microaggressions and the receipt of PNC in AA women. Racial microaggressions—chronic or episodic daily race-related hassles that occur in the form of subtle, innocuous degradations and putdown—are often encountered by people of color with greater frequency than major experiences of racial discrimination.11 They often “create an atmosphere of expectation that something racist will happen.”25 This paper also examines the social significance of shades of skin color by investigating whether maternal skin tone moderates the relationship between experiences of racial discrimination and PNC.
METHODS
Study Population
This study used data from the Life-course Influences of Fetal Environments (LIFE) Study, a retrospective cohort study administered in June 2009–December 2011. Details regarding LIFE have been published elsewhere11,26,27; women were eligible to participate if they self-identified as AA/black, were aged 18–45 years, and gave birth to a singleton at a suburban hospital located in Metropolitan Detroit, MI. A total of 1,999 eligible women were approached by study staff; 71% (n=1,410) provided written consent and were interviewed 24–48 hours post-delivery by trained study staff prior to hospital discharge. Study participants were similar to U.S. black women who gave birth in 2010.26 Medical information was collected through medical record abstraction. LIFE was approved by Wayne State University and St. John Providence Health System IRBs.
Measures
Racial microaggressions that occurred during and 3 months prior to the index pregnancy (year prior to delivery) were operationalized using the 20-item Daily Life Experiences of Racial Discrimination and Bother (DLE-B) instrument.11 Examples of microaggressions include being ignored/overlooked; opinions being minimized, ignored, or devalued; being observed/followed in public areas; and mistaken for someone else of the same race. The DLE-B assesses the frequency that each microaggression is perceived to have transpired (1, never; 2, less than once a year; …; 5, few times a year; 6, once a week or more) and the extent that the reported racial microaggressions bothered the individual (1, never; 2, not at all; …; 5, a lot; 6, extremely).11,28 A summary score was developed by summing each item weighted by the participant’s response to how much the microaggression bothered them; the summary score ranged from 20 (low) to 720 (high). Prior publications,28,29 including one from LIFE,11 show the DLE-B to be valid and reliable. Per prior literature,30 the DLE-B was modeled as a dichotomous variable, to compare women who experienced discrimination with those who report little or no discrimination (score above versus at or below the median, respectively).
Delayed PNC was operationalized by categorizing women into two groups based on the month of their first recorded PNC visit: no PNC or first PNC visit in the third trimester versus first PNC visit prior to the third trimester (reference group). As a secondary outcome, a three-level categorical variable was created based on the trimester of pregnancy PNC began: (1) first trimester (reference group), (2) second trimester, and (3) third trimester or no PNC.
Skin tone was assessed using a self-reported measure from the Detroit Area Study and the National Survey of American Life.31,32 Women were asked to report their shade of skin color, compared to most black people, using a 5-point Likert-like scale (1, very dark brown; 2, dark brown; 3, medium brown; 4, light brown; 5, very light brown). Women were categorized into three groups: (1) dark, (2) medium, and (3) light; the distribution was similar to prior skin tone studies.32–34
Potential confounders, identified a priori from literature, were maternal age, highest grade level, marital status, health insurance (private versus public), current city of residence (Detroit versus Outer Metropolitan Detroit), employment status in pregnancy, receipt of Special Supplemental Nutrition Program for Women, Infants, and Children or food stamps (yes versus no). Parity was obtained from the medical record. Chronic medical conditions were not included as control variables because they may lie on the causal pathway between racism and health care10 and data on date of diagnosis or utilization of care related to the condition were not available.
Statistical Analysis
Statistical analyses were conducted in August 2017–July 2018 with Stata, version 14. Univariate and bivariate statistics were used to assess the distribution of sample characteristics by delayed PNC. Binary and multinomial logistic regression, to estimate ORs and 95% CIs, was used to examine the association between the DLE-B as a dichotomous variable and delayed PNC outcomes and to assess effect modification by maternal skin tone. Models were built using a stepwise approach. Model 1 assessed the main effects of the DLE-B median variable; Model 2 tested the main effects of the DLE-B median variable adjusted for potential confounders (including maternal skin tone). Potential confounders included in the multivariable regression model were those that changed the coefficient for the DLE-B median variable >5% when entered into the model alone or in combination with another covariate.35 Model 3 assessed interactive effects of the DLE-B median variable and the three categories of maternal skin tone on PNC while adjusting for covariates included in Model 2; significance of the interaction term was assessed using the Likelihood Ratio (LR) test with p<0.10. Effect modification by maternal skin tone was also assessed through stratified analyses.
Variables were assessed for missing values; 3.8% of women were missing outcome data and 7.5% of women were missing the DLE-B. Little (<1%) data were missing on covariates. As <10% of analytic variables were missing data, listwise deletion was employed. Because exposure to racial discrimination is more pervasive over the life course for U.S.-born (versus foreign-born) black women, the sample was restricted to U.S.-born women.36 Foreign-born women comprised <2% (n=26) of the cohort. The final analytic sample included 1,209 women (85.6% of the cohort).
In the exploration of the DLE-B and delayed PNC, sensitivity analyses were conducted to separate occurrences of discrimination from stress appraisal due to the reported discriminatory event by repeating the above analyses with each DLE-B subscale categorized at the median.
RESULTS
Maternal characteristics are displayed in Table 1. Women had a mean age of 27.2 (SD=6.2) years. Almost half (49.7%) resided in the City of Detroit at the time of enrollment; the remainder resided in Outer Metropolitan Detroit. Roughly half (47.5%) of women self-ascribed their skin tone as medium brown; women reporting light brown and dark brown skin comprised 31.8% and 20.8%, respectively. The mean DLE-B score was 96.1 (SD=79.9) and ranged from 20 to 637; a higher score indicated greater experiences of racial microaggressions. The mean DLE-B score varied by maternal skin tone with women on either end of the color continuum reporting greater experiences of discrimination as compared with women with medium brown skin tone (light brown: 99.3, SD=82.9; medium brown: 92.0, SD=75.8; dark brown: 100.6, SD=83.4). Nearly half (48.3%) of women had their first recorded PNC visit in the first trimester of pregnancy, 26.7% in the second trimester of pregnancy, and the remainder (24.8%) either had no PNC or their first visit occurred in the third trimester. Maternal characteristics stratified by maternal skin tone are in Appendix Table 1.
Table 1.
Distribution of Prenatal Care by Maternal Characteristics in the LIFE Study, Metropolitan Detroit, Michigan, 2009–2011
| Characteristic | Total sample N=l,209 |
First PNC visit <7 months |
No/late PNCa |
OR (95% CI) |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Prenatal care | ||||
| No/late PNCa | 300 (24.8) | – | – | – |
| PNC initiation <7 months | 909 (75.2) | – | – | – |
| Maternal age, years | ||||
| Mean, SD | 27.2, 6.2 | 27.5, 6.1 | 26.3, 6.3 | 0.97 (0.95, 0.99) |
| 18–19 | 102 (8.4) | 60 (6.6) | 42 (14.0) | 2.84 (1.66,4.87) |
| 20–29 | 698 (57.7) | 532 (58.5) | 166 (55.3) | 1.27 (0.84, 1.91) |
| 30–34 | 232 (19.2) | 175 (19.3) | 57 (19.0) | 1.32 (0.82,2.12) |
| ≥35 | 177 (14.6) | 142 (15.6) | 35 (11.7) | 1.00 (ref) |
| Current city of residence | ||||
| City of Detroit | 590 (48.8) | 426 (46.9) | 164 (54.7) | 1.37 (1.05, 1.78) |
| Outer Metro Detroit | 619 (51.2) | 483 (53.1) | 136 (45.3) | 1.00 (ref) |
| Employed | ||||
| Yes | 597 (49.4) | 460 (50.6) | 137 (45.7) | 1.00 (ref) |
| No | 612 (50.6) | 449 (49.4) | 163 (54.3) | 1.21 (0.94, 1.58) |
| Educational attainment | ||||
| Mean, SD (years) | 13.7, 1.9 | 13.6, 1.9 | 13.9, 1.9 | 0.98 (0.91, 1.04) |
| ≤High school/GED | 204 (16.9) | 156 (17.2) | 48 (16.0) | 1.13 (0.69, 1.86) |
| Some college | 846 (70.0) | 628 (69.1) | 218 (72.7) | 1.27 (0.85, 1.92) |
| ≥Associates degree | 159 (13.2) | 125 (13.8) | 34 (11.3) | 1.00 (ref) |
| Receipt of WIC/food stamps | ||||
| Yes | 638 (52.8) | 491 (54.0) | 147 (49.0) | 1.00 (ref) |
| No | 571 (47.2) | 418 (46.0) | 153 (51.0) | 1.22 (0.94, 1.59) |
| Marital status | ||||
| Single | 654 (54.1) | 501 (55.1) | 153 (51.0) | 0.85 (0.65, 1.10) |
| Married/living with partner | 555 (45.9) | 408 (44.9) | 147 (49.0) | 1.00 (ref) |
| Health insurance | ||||
| Private | 474 (39.2) | 368 (40.5) | 106 (35.3) | 1.00 (ref) |
| Public | 735 (60.8) | 541 (59.5) | 194 (64.7) | 1.24 (0.95, 1.63) |
| Parity (number of previous live births) | ||||
| None | 522 (43.2) | 390 (42.9) | 132 (44.0) | 1.16 (0.85, 1.59) |
| 1 | 367 (30.4) | 284 (31.2) | 83 (27.7) | 1.00 (ref) |
| ≥2 | 320 (26.5) | 235 (25.8) | 85 (28.3) | 1.24 (0.87, 1.73) |
| History of chronic medical conditions | ||||
| Yes | 363 (30.0) | 292 (32.1) | 71 (23.7) | 1.53 (1.13,2.06) |
| No | 846 (70.0) | 617 (67.9) | 229 (76.3) | 1.00 (ref) |
| Racial microaggressions (DLE-B)b | ||||
| <Median (score 39–70) | 601 (49.7) | 464 (51.1) | 137 (45.7) | 1.00 (ref) |
| ≥Median (score 71–637) | 608 (50.3) | 445 (49.0) | 163 (54.3) | 1.24 (0.95, 1.61) |
| Maternal skin tone | ||||
| Light brown | 384 (31.8) | 286 (31.5) | 98 (32.7) | 1.06 (0.78, 1.43) |
| Medium brown | 574 (47.5) | 434 (47.7) | 140 (46.7) | 1.00 (ref) |
| Dark brown | 251 (20.7) | 189 (20.8) | 62 (20.7) | 1.02 (0.72, 1.43) |
Includes 85 women with first recorded PNC visit >7 month of pregnancy.
Higher score represents greater experiences of racial discrimination.
LIFE, Life-course Influences of Fetal Environments; DLE-B, Daily Life Experiences of Racial Discrimination and Bother Scale; PNC, prenatal care; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
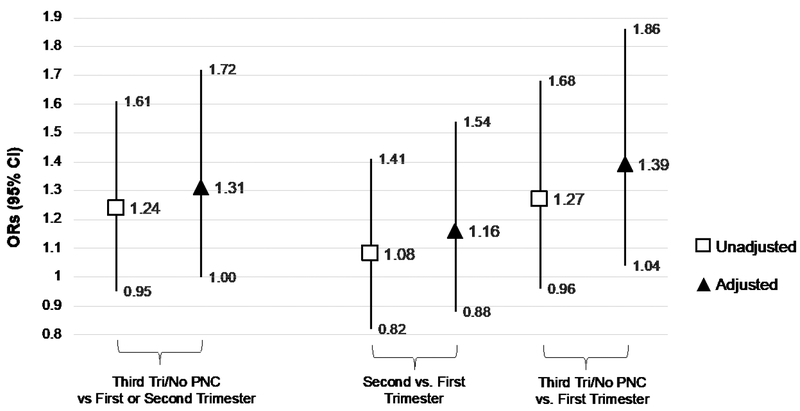
Results from the binary logistic regression showed AA women with a DLE-B score above the median were 24% more likely than AA women with a DLE-B score at or below the median to have delayed PNC (unadjusted OR=1.24, 95% CI=0.95, 1.61). After controlling for maternal skin tone, maternal age, city of residence, grade level, health insurance, parity, and receipt of Special Supplemental Nutrition Program for Women, Infants, and Children/food stamps, the association was slightly stronger (AOR=1.31, 95% CI=1.00, 1.72). Trimester of PNC initiation presented similar results (Figure 1).
Figure 1.
ORs for the association between racial microaggressions (DLE-B score >71) and delayed PNC among African American women in the LIFE Study, Metropolitan Detroit, Michigan, 2009–2011 (N=1,209).
Note: Delayed PNC is operationalized first as a binary variable with first or second trimester entry as the reference group and second as a three-level categorical variable with first trimester entry as the reference group. AORs were controlled for maternal age, city of residence, grade level, health insurance, parity, employment, and receipt of Special Supplemental Nutrition Program for Women, Infants, and Children or food stamps.
DLE-B, Daily Life Experiences and Bother Scale; PNC, prenatal care.
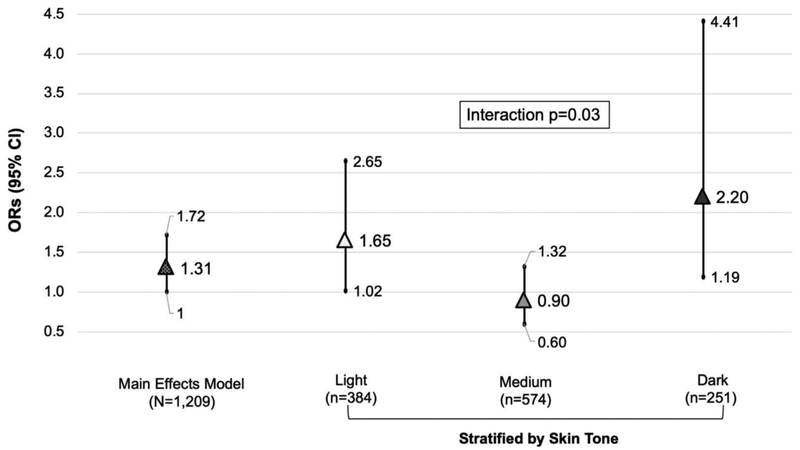
Next, analyses tested whether maternal skin tone modified the relationship between the DLE-B median and delayed PNC by including two skin tone X DLE-B interaction terms into the adjusted main effects model (Figure 2). The global test for the interaction terms was statistically significant (LR test: X2=6.83, df=2, p=0.03). Exploration of the interaction via stratification of the adjusted main effects model by maternal skin tone demonstrated that a DLE-B score above the median was associated with an increased odds of delayed PNC among light brown AA women (AOR=1.67, 95% CI=1.02, 2.71) and dark brown AA women (AOR=2.29, 95% CI=1.18, 4.43). No association was found among medium brown women. Again, similar patterns were observed for delayed PNC when operationalizing it as a three-level categorical variable with first trimester PNC entry as the reference group (Appendix Table 2). For light brown AA women, results were suggestive of a DLE-B score above the median being associated with the odds of PNC entry in the second trimester (AOR=1.50, 95% CI=0.90, 2.50). A DLE-B score above the median was associated with the odds of third trimester/no PNC entry (AOR=1.90, 95% CI=1.14, 3.17). Among dark brown AA women, a DLE-B score above the median was just associated with the odds of third trimester/no PNC entry (AOR=2.14, 95% CI=1.07, 4.32). No association was found among medium brown AA women. Additional analyses suggested the presence of a three-way interaction with parity (LR test: X2=4.83, df=2, p=0.09), but not maternal age (LR test: X2=2.16, df=2, p=0.27).
Figure 2.
AORs for the relationship between racial microaggressions (DLE-B score >71) and delayed PNC, overall and stratified by maternal skin tone, LIFE study, Metropolitan Detroit, Michigan, 2009–2011 (N=1,209).
Note: Delayed PNC is operationalized first as a binary variable with first or second trimester entry as the reference group. AORs were controlled for maternal age, city of residence, grade level, health insurance, parity, employment, and receipt of Special Supplemental Nutrition Program for Women, Infants, and Children or food stamps. Women who entered PNC <3 months served as the reference group.
DLE-B, Daily Life Experiences and Bother Scale; PNC, prenatal care.
Results from the sensitivity analyses with the DLE-Bothered and DLE-Occurrence subscales (Appendix Table 3) demonstrated associations similar to the overall DLE-B; however, the strength of association was stronger in the full sample for the DLE-Bothered subscale (AOR=1.39, 95% CI=1.06, 1.82) as compared with the DLE-Occurrence subscale (AOR=1.21, 95% CI=0.93, 1.68). Results stratified by skin tone showed both subscales were associated with delayed PNC in light and dark brown AA women, but not medium brown AA women.
DISCUSSION
Despite longstanding racial/ethnic disparities associated with PNC and researchers hypothesizing racial discrimination as a potential antecedent of the disparity,37–40 quantitative studies exploring racial discrimination as a barrier to receiving care are few (DeMarco et al.39 and Slaughter-Acey and colleages37 are exceptions). This study investigated whether exposure to racial discrimination was associated with AA women either not getting or delaying entry into PNC. Findings suggest that lived experiences in the form of racial microaggressions may influence AA women’s use of health care, particularly PNC.
Literature posits experiences of racial discrimination in general or within the healthcare setting may govern the way people of color perceive the healthcare system as well as how they access/utilize services.10,37,41 Indeed, a 2017 report on AA experiences of discrimination found that one fifth to one third of AAs report that they avoid seeking needed services (e.g., calling the police or medical care) to prevent potential discrimination.41 Roman et al.40 found that AA women perceived their experiences (provider attitudes, extended wait times, staff facial expressions) across the continuum of clinical and community-based care were influenced by their race and insurance status. It could be that AA women in LIFE who perceived greater experiences of racial microaggressions, in general or in the healthcare setting, develop a sense of hypervigilance and avoid or delay PNC as a way to circumvent potential discrimination.
Studies examining individual characteristics that influence (e.g., enhance, facilitate, buffer) the nature of the racism/racial discrimination–healthcare use relationship predominantly focus on age, ethnicity, gender, and income.42 Skin tone is one of the most notable physical attributes18; as a visible cue, it can illicit racial bias and discrimination by triggering culturally embedded racial stereotypes and prejudice.18 In the exploration of skin tone as an effect modifier, this study found maternal skin tone moderated the association between exposure to racial discrimination in the form of racial microaggression and PNC. Greater amounts of racial discrimination were correlated with delayed PNC for AA women on the ends of the color continuum (i.e., light and dark brown, but not medium brown).
At first glance, this finding seems counterintuitive given that colorism assigns privilege to individuals with lighter skin color. Colorism is insidiously complex; the way skin tone moderates the racial discrimination–PNC relationship may be a function of both outgroup colorism (perpetuated by whites) and ingroup colorism (perpetuated by blacks) as well as hyper-residential segregation of Metropolitan Detroit.43 A recent study based on nationally representative sample of AA women found that medium brown women perceived ingroup colorism with less frequency than light or dark brown women; medium brown women also reported fewer encounters of outgroup colorism than their dark brown but not light brown peers.32 Furthermore, Wilder,44 in focus groups with AA women, also found ingroup colorism operated in a three-tiered structure where colorism language and stereotypes attached to medium brown skin were more neutral.
This study has several strengths. First, the socioeconomically diverse sample was entirely composed of AA women, which allowed for the exploration of ingroup heterogeneity. To the authors’ knowledge, this study is the first epidemiologic study to quantitatively examine skin tone, as a social construct, and how its salience may drive women’s engagement with health care in the U.S., particularly PNC. This study used self-rated skin tone, rather than spectrometer-based or interviewer-rated skin tone; self-ascribed skin tone has been shown to be a better predictor of racialized social interactions.20,31,33 Moreover, self-ascribed skin tone captures the individual’s subjective perceptions of their social hierarchy in society.20,33 Still, findings may only be generalizable to non-Hispanic black/AA women born in the U.S. as foreign-born women were excluded. Future research should consider how colorism may vary across the ethnic groups within the Black Diaspora in America—that is, descendants of Africans brought to the U.S. as slaves, African immigrants, Afro-Latinas, and Caribbean Americans.18 Furthermore, as colorism is not specific to blacks,24 future research should consider how the antecedents and sequela of colorism affect other women of color in the U.S. and their engagement with health care.
Limitations
There are limitations to consider. As always, there is potential for measurement error in constructed variables. Timing of PNC visits was ascertained from the medical record, standard of practice for the 2003 revised U.S. birth certificate. It is possible that medical records may not have captured the first visit if the woman changed her prenatal provider. In relation to the exposure, the DLE-B did not take into consideration gendered experiences of racial microaggressions. Future research investigating racial discrimination as a barrier to healthcare for people of color should incorporate an intersectional framework45,46 as a growing body of literature suggests experiences of racial discrimination and other race-related stressors can be gender specific.34,47 Finally, this study is not able to infer causality. With that said, recruitment of women during the immediate postpartum period, versus prenatal recruitment, likely increased the generalizability of the results because prospective designs skew the probability of recruitment to women with lower-risk profiles.48
CONCLUSIONS
In summary, this study found maternal skin tone, a proxy for colorism, intersects with racial discrimination in the form of racial microaggressions to influence AA women’s use of PNC. Findings have implications related to the engagement of women of color, particularly AA women, in healthcare systems and maternal and child health programs.
Supplementary Material
ACKNOWLEDGMENTS
This work has been supported in part by Grant # 96-18-03 from the Russell Sage Foundation to Dr. Slaughter-Acey. The Life-course Influences of Fetal Environments (LIFE) Study was funded by NIH grant no. R01HD058510 to Dr. Misra. Dr. Parker is supported by a NIH/NIA-funding grant no. R01AG049692 – 02W1. Any opinions expressed are those of the author(s) alone and should not be construed as representing the opinions of the Russel Sage Foundation or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Handler A, Johnson K. A call to revisit the prenatal period as a focus for action within the 3reproductive and perinatal care continuum. Matern Child Health J. 2016;20(11):2217–2227. 10.1007/s10995-016-2187-6. [DOI] [PubMed] [Google Scholar]
- 2.Kitsantas P, Gaffney KF, Cheema J. Life stressors and barriers to timely prenatal care for women with high-risk pregnancies residing in rural and nonrural areas. Womens Health Issues. 2012;22(5):e455–e460. 10.1016/j.whi.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116(4):306–316. 10.1016/s0033-3549(04)50052-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Obstetrics and Gynecology. Preeclampsia and high blood pressure during pregnancy. FAQ034. www.acog.org/Patients/FAQs/Preeclampsiaand-High-Blood-Pressure-During-Pregnancy?IsMobileSet=false. Published 2014. Accessed July 23, 2018.
- 5.HHS, Health Resources and Services Administration, Maternal and Child Health Bureau. Child health USA; 2014 https://mchb.hrsa.gov/chusa14/. Published 2015. Accessed April 22, 2019. [Google Scholar]
- 6.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol. 2012;120(2):261–268. 10.1097/aog.0b013e31825cb87a. [DOI] [PubMed] [Google Scholar]
- 7.Yan J The effects of prenatal care utilization on maternal health and health behaviors. Health Econ. 2017;26(8):1001–1018. 10.1002/hec.3380. [DOI] [PubMed] [Google Scholar]
- 8.Gadson A, Akpovi E, Mehta PK. Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Semin Perinatol. 2017;41(5):308–317. 10.1053/j.semperi.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Bhopal RS. Racism in health and health care in Europe: reality or mirage? Eur J Public Health. 2007;17(3):238–241. 10.1093/eurpub/ckm039. [DOI] [PubMed] [Google Scholar]
- 10.Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: a systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900 10.1371/journal.pone.0189900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slaughter-Acey JC, Sealy-Jefferson S, Helmkamp L, et al. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26(1):7–13. 10.1016/j.annepidem.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burgess DJ, Ding Y, Hargreaves M, van Ryn M, Phelan S. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved. 2008;19(3):894–911. 10.1353/hpu.0.0063. [DOI] [PubMed] [Google Scholar]
- 13.Major B, O’Brien LT. The social psychology of stigma. Annu Rev Psychol. 2004;56:393–421. 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 14.Hunter M “If you’re light you’re alright” light skin color as social capital for women of color. Gend Soc. 2002;16(2):175–193. 10.1177/08912430222104895. [DOI] [Google Scholar]
- 15.Keith VM. A colorstruck world: Skin tone, achievement, and self-esteem among African American women In: Glenn EN, ed. Shades of Difference: Why skin color matters. Stanford, CA: Stanford University Press; 2009:25–39. [Google Scholar]
- 16.Thompson MS, Keith VM. The blacker the berry: gender, skin tone, self-esteem, and self-efficacy. Gend Soc. 2001;15(3):336–357. 10.1177/089124301015003002. [DOI] [Google Scholar]
- 17.Jones J Constructing race and deconstructing racism: a cultural psychology approach In: Bernai G, Trimble J, Burlew A, eds. Handbook of Racial & Ethnic Minority Psychology. Thousand Oaks, CA: SAGE Publications, Inc.; 2003. 10.4135/9781412976008.n14. [DOI] [Google Scholar]
- 18.Adams EA, Kurtz-Costes BE, Hoffman AJ. Skin tone bias among African Americans: antecedents and consequences across the life span. Dev Rev. 2016;40:93–116. 10.1016/j.dr.2016.03.002. [DOI] [Google Scholar]
- 19.Stewart QT, Cobb RJ, Keith VM. The color of death: race, observed skin tone, and all-cause mortality in the United States. Ethn Health. In press. Online May 8, 2018. 10.1080/13557858.2018.1469735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cobb RJ, Thomas CS, Pirtle WNL, Darity WA. Self-identified race, socially assigned skin tone, and adult physiological dysregulation: assessing multiple dimensions of “race” in health disparities research. SSM Popul Health. 2016;2:595–602. 10.1016/j.ssmph.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sweet E, McDade TW, Kiefe CI, Liu K. Relationships between skin color, income, and blood pressure among African Americans in the CARDIA study. Am J Public Health. 2007;97(12):2253–2259. 10.2105/ajph.2006.088799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunter M The persistent problem of colorism: skin tone, status, and inequality. Sociol Compass. 2007;1(1):237–254. 10.1111/j.1751-9020.2007.00006.x. [DOI] [Google Scholar]
- 23.Goldsmith AH, Hamilton D, Darity W. Shades of discrimination: skin tone and wages. Am Econ Rev. 2006;96(2):242–245. 10.1257/000282806777212152. [DOI] [Google Scholar]
- 24.Glenn EN. Shades of difference: why skin color matters. Stanford University Press; 2009. [Google Scholar]
- 25.Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry. 2000;70(1):42–57. 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- 26.Osypuk TL, Slaughter-Acey JC, Kehm RD, Misra DP. Life-course social mobility and reduced risk of adverse birth outcomes. Am J Prev Med. 2016;51(6):975–982. 10.1016/j.amepre.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sealy-Jefferson S, Giurgescu C, Helmkamp L, Misra DP, Osypuk TL. Perceived physical and social residential environment and preterm delivery in African-American women. Am J Epidemiol. 2015;182(6):485–493. 10.1097/01.ogx.0000480257.00385.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bond M, Kalaja A, Markkanen P, et al. Expanding our understanding of the psychosocial work environment: a compendium of measures of discrimination, harassment and work-family issues NIOSH Publication No. 2008–104. Cincinnati, OH: National Institute for Occupational Safety and Health; 2008. 10.26616/nioshpub2008104. [DOI] [Google Scholar]
- 29.Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. J Pers Soc Psychol. 2003;84(5):1079–1092. 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- 30.Rankin KM, David RJ, Collins JW Jr. African American women’s exposure to interpersonal racial discrimination in public settings and preterm birth: the effect of coping behaviors. Ethn Dis. 2011;21(3):370–376. [PubMed] [Google Scholar]
- 31.Brown KT. Skin tone bias and African-American well-being: a dual influence model approach [dissertation]. Ann Arbor, MI: University of Michigan; 1998. [Google Scholar]
- 32.Uzogara EE, Jackson JS. Perceived skin tone discrimination across contexts: African American women’s reports. Race Soc Probl. 2016;8(2):147–159. 10.1007/s12552-016-9172-y. [DOI] [Google Scholar]
- 33.Monk EP Jr. The cost of color: skin color, discrimination, and health among African-Americans. Am J Sociol. 2015;121(2):396–444. 10.1086/682162. [DOI] [PubMed] [Google Scholar]
- 34.Hargrove TW. Light privilege? Skin tone stratification in health among African Americans. Sociol Race Ethn. In press Online September 20, 2018. 10.1177/2332649218793670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 36.Dominguez TP, Strong EF, Krieger N, Gillman MW, Rich-Edwards JW. Differences in the self-reported racism experiences of U.S.-born and foreign-born black pregnant women. Soc Sci Med. 2009;69(2):258–265. 10.1016/j.socscimed.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slaughter-Acey JC, Caldwell CH, Misra DP. The influence of personal and group racism on entry into prenatal care among African American women. Womens Health Issues. 2013;23(6):e381–e387. 10.1016/j.whi.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salm Ward TC, Mazul M, Ngui EM, Bridgewater FD, Harley AE. ―You learn to go last‖: perceptions of prenatal care experiences among African-American women with limited incomes. Matern Child Health J. 2013;17(10):1753–1759. 10.1007/s10995-012-1194-5. [DOI] [PubMed] [Google Scholar]
- 39.De Marco M, Thorburn S, Zhao W. Perceived discrimination during prenatal care, labor, and delivery: an examination of data from the Oregon pregnancy risk assessment monitoring system, 1998–1999, 2000, and 2001. Am J Public Health. 2008;98(10):1818–1822. 10.2105/ajph.2007.123687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roman LA, Raffo JE, Dertz K, et al. Understanding perspectives of African American Medicaid-insured women on the process of perinatal care: an opportunity for systems improvement. Matern Child Health J. 2017;21(suppl 1):81–92. 10.1007/s10995-017-2372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harvard TH Chan School of Public Health, National Public Radio, Robert Wood Johnson Foundation. Discrimination in America: Experiences and views of African Americans. Published October 2017. [Google Scholar]
- 42.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–127. 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 43.Eisinger P Reimagining Detroit. City Community. 2003;2(2):85–99. 10.1111/1540-6040.00042. [DOI] [Google Scholar]
- 44.Wilder J Revisiting “color names and color notions” a contemporary examination of the language and attitudes of skin color among young black women. J Black Stud. 2010;41(1):184–206. 10.1177/0021934709337986. [DOI] [PubMed] [Google Scholar]
- 45.Bowleg L The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. 10.2105/ajph.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crenshaw K The intersection of race and gender In: Crenshaw K, Gotanda N, Peller G, eds. Critical race theory: The key writings that formed the movement. New York, NY: The New Press; 1995. [Google Scholar]
- 47.Jackson FM, Phillips MT, Hogue CJR, Curry-Owens TY. Examining the burdens of gendered racism: implications for pregnancy outcomes among college-educated African American women. Matern Child Health J. 2001;5(2):95–107. [DOI] [PubMed] [Google Scholar]
- 48.Kramer MS. Socioeconomic disparities in preterm birth. Paediatr Perinat Epidemiol. 2015;29(3):169–171. 10.1111/ppe.12186. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.