Abstract
Background:
Orthopaedic injuries of National Football League (NFL) players can have a deleterious effect on their health, with minimal to no high-level evidence on the management of these injuries.
Purpose:
To summarize all data published between January 1980 and March 2018 on orthopaedic injuries experienced by NFL candidates and professional players in the NFL.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A literature search of studies examining orthopaedic injuries in the NFL was performed through the PubMed, Embase, and CINAHL databases. The review included studies of orthopaedic injuries in college football recruits attending the NFL Combine as well as professional NFL players. Excluded were studies of nonorthopaedic injuries, such as concussions, traumatic brain injury, facial injuries, and vascular injuries, as well as case reports.
Results:
A total of 147 articles met the inclusion criteria and were divided into 11 topics based on anatomic site: general (16%), spine (13%), shoulder (13%), elbow (3%), hand and wrist (3%), trunk (0.7%), hip and pelvis (7%), thigh (3%), knee (24%), ankle (5%), and foot (12%). Of these studies, 74% were of level 4 evidence. Most studies obtained data from the NFL Combine database (26%), by searching the internet (24%), and via the NFL Injury Surveillance System (22%). Studies using internet search methods to identify injuries consistently found fewer participants than studies using the NFL Injury Surveillance System.
Conclusion:
This systematic review provides National Collegiate Athletic Association and NFL team physicians with a single source of the most current literature regarding orthopaedic injuries in NFL players. Most research was published on knee, spine, shoulder, and foot injuries and consisted of level 4 evidence. A substantial portion of the published literature was based on data obtained from internet searches and may not accurately represent the NFL population.
Keywords: orthopaedic, musculoskeletal, injury, football, Combine, National Football League
American football enjoys broad participation, and injuries commonly occur.1,4,101 Football is also associated with the most catastrophic injuries and fatalities among sports in the United States.1 The National Football League (NFL) and fantasy football are extremely popular, and information about player’s injuries can often be found in the public domain. This makes it possible to create databases from publicly available information and publish studies using these databases. Additionally, the anecdotal observations of NFL team physicians suggest that the injuries experienced by NFL players experience are unique in comparison with those of the general US population. One goal of medicine should be to base treatment on the highest levels of evidence. Injuries can have a deleterious effect on a football player’s health and career, and there is no high-level evidence to guide the management of injuries sustained by NFL players.88 The primary objective of this systematic review was to summarize all data published on orthopaedic injuries among college-level NFL recruits and professional players in the NFL. The secondary objective was to characterize the literature based on anatomic site, level of evidence, and source of data from which the study was based. Finally, when possible, we sought to compare the results among the different sources of data, including the NFL Injury Surveillance System (NFLISS), team and medical records, and internet-based sources.
Methods
PubMed, Embase, and CINAHL were searched from January 1, 1980, to March 31, 2018, to identify all studies of orthopaedic injuries in professional football players. Search terms were “National Football League” in combination with “combine” or “football.” We included studies of orthopaedic injuries in college football recruits attending the NFL Combine as well as those to professional NFL players. Excluded were case reports and studies of nonorthopaedic injuries, including concussions, traumatic brain injury, facial injuries, and vascular injuries. Two authors (W.H.K., W.M.L.) independently conducted the literature search and compared their findings. The articles were divided into 11 categories corresponding with the anatomic site of injury: general, spine, shoulder, elbow, hand and wrist, trunk, hip and pelvis, thigh, knee, ankle, and foot. Level of evidence, source of data, and type of injury were extracted from each article. Finally, when possible, we compared studies on overlapping topics that used various data sources, including the NFLISS, team or surgeon medical records, and the internet.
Results
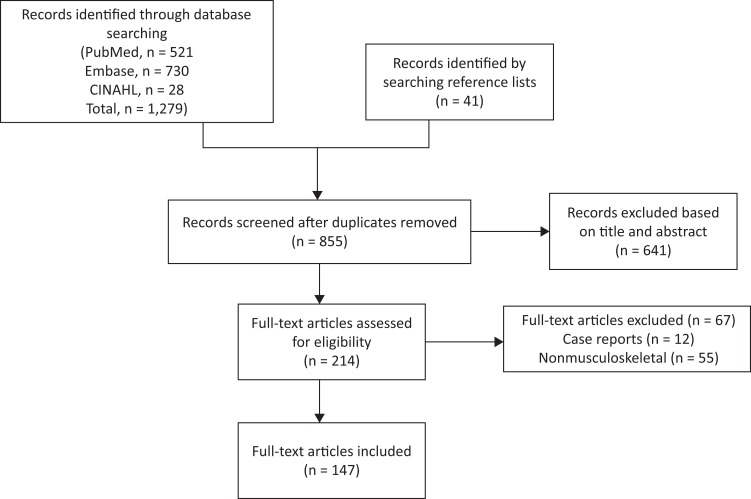
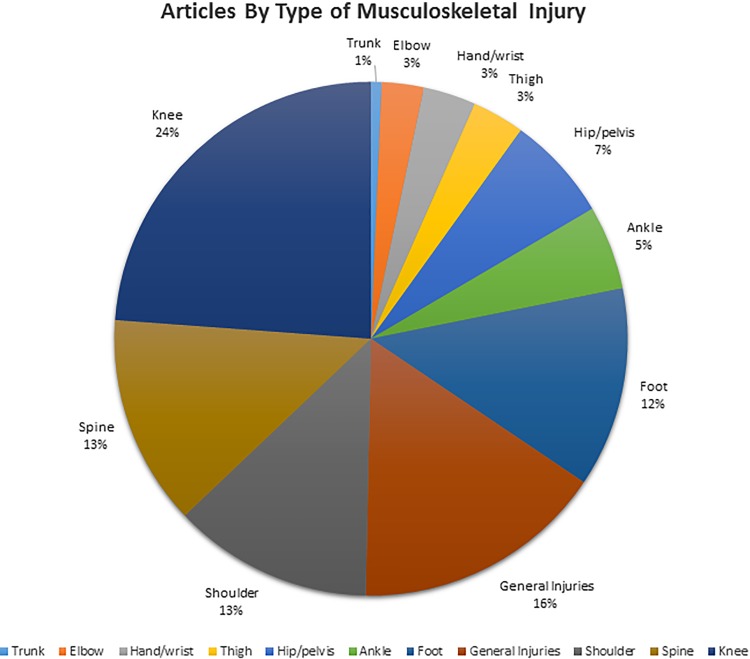
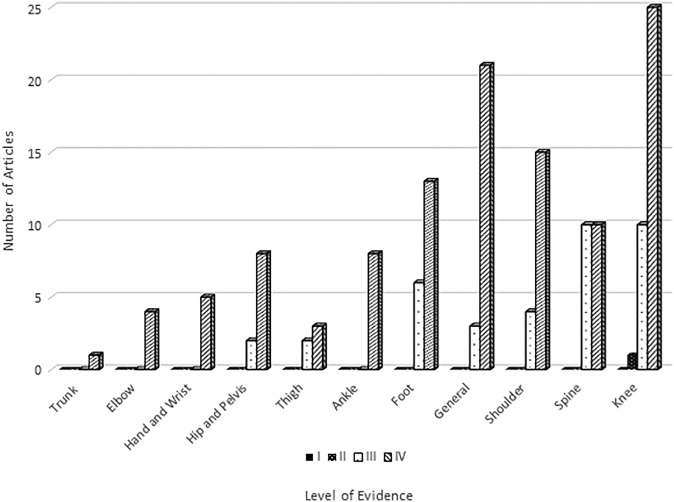
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the search strategy is presented in Figure 1. We identified 855 articles through our literature search, of which 147 articles published between 1980 and 2018 met the inclusion criteria. Figure 2 illustrates the number of included articles by type of orthopaedic injury. Most articles examined knee (24%), spine (13%), shoulder (13%), and foot (12%) injuries. Of the studies reviewed, 74% were of level 4 evidence (Figure 3). No level 1 studies met the inclusion criteria. As shown in Table 1, most studies obtained data from the NFL Combine database (26%), the internet (24%), and the NFLISS (22%). The results of the included articles are summarized and grouped according to anatomic location.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart.
Figure 2.
Percentage of articles by type of orthopaedic injury. Injury categories are not mutually exclusive.
Figure 3.
Number of articles by level of evidence and type of orthopaedic injury. No level 1 or 2 articles were found.
TABLE 1.
Number of Articles by Source of Data and Type of Injurya
| Source of Data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Type of Injury | NFL Combine Database | NFL Injury Surveillance System | Internet-Based Search of Publicly Available Data | Data From a Single Team | Medical Records of Players | Survey of Team Physicians or Athletic Trainers or Players | Med Sports Systems Limited Database | Data Collected by Athletic Trainers |
| Trunk | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| Elbow | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hand/Wrist | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 |
| Hip/Pelvis | 3 | 3 | 2 | 0 | 2 | 0 | 0 | 0 |
| Thigh | 1 | 2 | 0 | 2 | 0 | 0 | 0 | 0 |
| Ankle | 1 | 2 | 0 | 3 | 1 | 2 | 0 | 0 |
| Foot | 6 | 0 | 10 | 4 | 1 | 2 | 0 | 0 |
| General Injuries | 5 | 4 | 3 | 5 | 2 | 4 | 0 | 2 |
| Shoulder | 6 | 5 | 3 | 2 | 5 | 1 | 0 | 0 |
| Spine | 7 | 3 | 6 | 2 | 1 | 1 | 1 | 0 |
| Knee | 9 | 8 | 11 | 5 | 1 | 6 | 0 | 0 |
| Total | 38 | 33 | 36 | 24 | 14 | 18 | 1 | 2 |
aData are not mutually exclusive. NFL, National Football League.
General Information
Several studies investigated the football field and environmental conditions and their effect on injury. The studies consistently found higher rates of lower extremity injury on artificial surfaces in comparison with natural turf,46,107,108 although 1 study from 1989 to 1998 found lower rates of anterior cruciate ligament (ACL) tears on AstroTurf in cold weather.102 Lawrence et al71 found that game-day temperature below 50° was a risk factor for concussions and ankle injuries.
Medical grading systems can predict future availability and performance in NFL Scouting Combine players and should incorporate the player’s position and history of injury, with shoulder instability, meniscal injury, ACL tear, and other lower extremity injuries having well-documented decreased performance and availability effects.4,10,11,15,79,111
The most common site of injury was the knee, followed by hamstring strains and contusions.35,72 Injuries were more common in the first 2 weeks of training camp and during games35 and occurred most commonly in defensive players, particularly defensive backs, although other positions had unique injury patterns. These included acromioclavicular (AC) joint separations in quarterbacks, forearm fractures in defensive backs, and lower extremity strains in kickers.17,49,61,72 Corticosteroid injections for muscle strains as well as certain ligament sprains, such as the AC joint or ankle syndesmosis, have been shown to be safe as well as effective in allowing earlier return to play (RTP).29,30,75,85 Finally, several studies documented increased arthritis and whole-person impairment in former NFL players, with the cervical and lumbar spine being highly affected.27,42,97
Spinal Injuries
Spine injuries accounted for 7% of NFL injuries, were about 10 times more common in games than in practices, were most common in the cervical spine, and most commonly occurred in offensive linemen or defensive players who were blocking or tackling.43,82
Cervical Spine
The space available for the spinal cord on cervical magnetic resonance imaging (MRI) was decreased in heavy-contact NFL positions and was associated with chronic stingers when the space available for the spinal cord was <5 mm.109,110 Cervical pathology negatively affected the number of games played in the NFL but did not affect player performance.50,122 Players with cervical disc herniation may safely RTP, but RTP decreased to approximately 70% in those requiring anterior cervical discectomy and fusion (ACDF).80,93 Adjacent segment degeneration occurred in 10% of players undergoing ACDF, while those treated with foraminotomy had an RTP rate of 92% and returned earlier than those with ACDF but had a 50% reoperation rate.80
Lumbar Spine
Hyperconcavity of the lumbar spine was commonly found on radiographs but had no evident consequences.106 The lumbar spine was the most common site of disc herniation, especially L5/S1, and lumbar herniations were most common in offensive linemen.44 Lumber conditions, including disc herniation or spondylolisthesis, commonly led to team physicians’ downgrading draft prospects; but there were conflicting data regarding player longevity and no evident effect on performance in those players drafted into the NFL.78,121,123,127 Treatment of lumbar disc herniations with epidural injections allowed RTP in 90% of NFL players with few practices or games missed, but it was less successful in the setting of weakness on examination or disc sequestration on MRI.68 When surgery was indicated for lumbar disc herniation, NFL data and internet-based studies showed that RTP was approximately 75% to 80% but with 15% of players requiring revision decompression.51,52,118,141 Performance was preserved in those returning to play. Lumbar transverse process fractures occurred, rarely involved viscera, and typically took 3 to 4 weeks before RTP.138
Trunk Injuries
Chondral rib fractures were common and typically diagnosed by computed tomography and/or MRI. Sixty percent of team physicians used an anesthetic block for pain management acutely, and 40% used a block to allow for RTP.
Shoulder Injuries
A history of shoulder injury, particularly AC separation and instability, was found in 50% of NFL prospects, and the most common shoulder surgery was for anterior instability.39,58 Compared with players without shoulder injuries, those with a history of shoulder injury were more likely to go undrafted, and they played and started in fewer games.39
AC Joint
Most AC injuries occurred in games rather than practices, were low grade, and rarely required surgery, with quarterbacks missing more time than other players (17 vs 10 days).61,77
Rotator Cuff
Preexisting rotator cuff tears were rare in NFL prospects but, when present, they decreased the athletes' likelihood of being drafted and were associated with lower availability and performance in those who were drafted.41 Rotator cuff injuries included contusions and tears, and contusions led to minimal time lost and were treated with rehabilitation and occasionally with injection.25 Of players with rotator cuff injuries, 11% ultimately required surgery. Rotator cuff tears occurred most commonly in offensive linemen and linebackers, with 90% being treated with surgery and 90% of those surgically treated returning to play at a mean of 5 months.38 Residual shoulder pain after rotator cuff repair was common.
Fractures
Clavicle fractures were successfully treated nonoperatively and operatively, with both methods allowing RTP in 95% of players; however, surgical treatment led to earlier healing and RTP.55,94 Some athletes had decreased availability and/or performance after a clavicle fracture, including offensive skill players (quarterbacks, wide receivers [WRs], and running backs [RBs]).55,56
Shoulder Instability
Shoulder instability decreased the likelihood of NFL Combine prospects being drafted as well as reduced career longevity.14 Nonoperative treatment of instability had recurrence rates from 40% to 55% but allowed players to RTP in 1 week for subluxation and 3 weeks for dislocation, while players undergoing surgery had 80% to 90% RTP rates but took nearly 9 months before RTP, with a recurrence rate that ranged from 13% to 26%.74,100,145 Latarjet surgery history was rare in NFL Combine players but, when present, decreased the likelihood of being drafted and was commonly associated with hardware complications and glenohumeral osteoarthritis, with 1 of 2 studies showing a negative effect of Latarjet surgery on NFL participation.66,73
Other
SLAP (superior labral anterior-posterior) tears were rare in NFL Combine participants (3%) but, when present, decreased future player availability. When NFL Combine participants underwent labral repair, 32% had recurrent tearing and/or degenerative joint disease on MRI, but this did not affect availability in their first NFL season.65 In NFL players, SLAP tears were most common in offensive linemen and were typically treated nonoperatively (60%).23 Nonoperative treatment led to RTP after a mean of 21 days versus 4 to 5 months with surgery. Pectoralis major injuries were rare in NFL players (1 injury per season for the entire league) and occurred most often in games (90%) and during tackling (50%) rather than with weight lifting, with RTP after surgery taking 4 months on average.136
Elbow and Forearm Injuries
Most NFL elbow injuries were sprains (77%) or dislocations (18%) and included hyperextension (56%) or medial collateral ligament (MCL) injuries (20%).63 They most commonly occurred in offensive and defensive linemen.21 Elbow MCL sprains were usually treated nonoperatively, and players missed up to 1 game. Triceps tears often occurred in linemen, with one-third having prodromal symptoms and 25% having a prior steroid injection. Nearly half of partial triceps tears eventually required surgery, and athletes commonly returned to play following repair of partial and complete tears, although they may miss the remainder of the season and possibly the season after surgery.37,81 Forearm injuries were most commonly fractures and involved defensive backs.21
Hand and Wrist Injuries
Mall et al83 reported that the overall incidence of hand injuries in NFL players over 10 years (1996-2005) was 10.6 per 1000 athletic exposures, with 50% of injuries involving the fingers, 30% hand, and 20% first ray. Also according to Mall et al,83 metacarpal fractures (17%) and peripheral interphalangeal dislocations (17%), especially of the ulnar 2 digits, were the most common types of injuries, with the most common activity being tackling and the most common positions being linemen (hand) and WRs and defensive secondary (fingers). Thumb ligament injuries have been a topic of study, and researchers have found that ulnar collateral ligament injuries are often treated surgically, with RTP in 4 to 5 weeks and no decline in performance; 25% of ulnar collateral ligament injuries also involve the radial collateral ligament and should be treated surgically (which can safely be delayed until the end of the season).133,143
Lunate or perilunate dislocations were described in 10 NFL players, with hyperextension being the most frequent mechanism of injury.112 Closed or open reduction with percutaneous pinning allowed for successful RTP after a minimum of 4 weeks.
Hip and Pelvis Injuries
Feeley et al36 found that 3% of all NFL injuries involved the hip and were primarily muscle strains (36.3%). Defensive backs and WRs had the most hip injuries, and offensive linemen missed the most time (mean, 18.3 days). Blocking was the most common mechanism of hip injury, and contusions were due to contact while strains were usually noncontact injuries. Proximal rectus femoris avulsion was successfully treated nonoperatively, but time to RTP varied from 3 to 10 weeks.40 Adductor longus ruptures were usually treated nonoperatively, with RTP at a mean of 6 weeks, but surgery was indicated in approximately 25% of cases and RTP took 12 weeks.120
In NFL Combine attendees, a history of core muscle surgery did not significantly affect an athlete’s draft status or future NFL performance.64 In NFL players, an internet-based study found that 95% of players undergoing surgery for a core muscle injury were able to RTP, with no decrease in statistical performance but a slightly shorter career (approximately 6 months shorter on average) and 2 fewer games played per season in comparison with controls.53
Imaging studies of NFL Combine attendees and retired NFL players noted a high incidence of impingement findings, including labral tears (89%), chondral lesions (98%), and ligamentum teres tears (81%) in athletes with symptoms.28,95 An increased alpha angle seemed to be the best imaging study predictor of pain.70 Persistent symptoms of adductor and rectus strain that did not resolve despite therapy were described as the “sports hip triad” and should raise suspicion of a labral tear.36 Finally, when hip surgery was indicated, impingement surgery and labral repair both showed an RTP rate of approximately 85% to 90%,100,108 although the odds of RTP were about 6 times less in lineman compared to other positions.92,98
Thigh Injuries
A case-control study found that isokinetic parameters measured at the NFL Combine were not associated with hamstring injuries that occurred within the player’s first season.147 Hamstring injuries primarily occurred 4 times as often during the preseason as in the regular season, happened primarily during practices (53%), were noncontact (82%), and resulted in a mean 13 days lost among NFL players.32 Forty-one percent of hamstring injuries were minor (<7 days lost), 41% moderate (1-3 weeks lost), and 18% major (>21 days lost), and most hamstring injuries occurred in defensive backs (23%), WRs (21%), and special teams players (13%). Corticosteroid injection for hamstring strain can safely speed RTP without leading to recurrence, while platelet-rich plasma has not been effective.75,114 Finally, repair of proximal hamstring avulsions can restore strength, but only 5 of 10 NFL players who underwent early repair were able to play in more than 1 NFL game after surgery.86
Knee Injuries
General
Among NFL Combine attendees, approximately 50% had a history of knee injury, most commonly MCL (40.8%), meniscal (26.3%), or ACL (19%).8 Linemen and tight ends had the highest incidence of knee injury (57%-68%), and knee surgery was most common in RBs and linebackers (35%).
Anterior Cruciate Ligament
Two percent of all injuries reported to the NFLISS between 1994 and 1998 involved the ACL.9 Most noncontact ACL tears from 1989 to 1993 occurred during games (47.5%), on natural grass (65.6%), and on a dry surface (93.4%).125 A video analysis found that the majority of ACL tears (72%) in NFL athletes involved a noncontact mechanism, with the lower extremity exhibiting significant valgus of the knee, particularly during lateral movement.57 The incidence of ACL injuries was the highest for speed players (6.3%-10%), including WRs, tight ends, linebackers, fullbacks, and halfbacks, and players experiencing reinjury were more likely to injure the same knee versus the contralateral knee (12.3% vs 7.3%, P < .05).26
A study of NFL Combine participants found that a 30° reduction of hip internal rotation was associated with increased odds of ACL tears in the ipsilateral (odds ratio, 4.06) and contralateral (odds ratio, 5.29) sides.5 In a separate imaging study of combine athletes, ACL reconstructions with more posterior tibial tunnels and grafts with less sagittal obliquity had increased translation on Lachman examination.84 Finally, Keller et al60 studied players at the 2010 through 2014 NFL Combines and found no differences in measures of speed, jumping, agility, and quickness in players with a history of ACL reconstruction versus controls; in addition, they found that isolated ACL reconstruction in combine participants did not shorten their future NFL career.13
Survey studies of NFL team physicians regarding management of ACL injuries found that 80% to 90% preferred patellar tendon autograft via a single-bundle technique, most recommended at least 6 months until RTP, and most did not routinely recommend a brace.9,33,88
RTP after ACL reconstruction ranged from 60% to 90%, varied by position, and was highest in quarterbacks, but longevity was found to be diminished.24,31,34,113,128,146 RTP was lower in less experienced and/or less highly skilled players, had a significant negative financial impact on future earnings, and was also associated with diminished performance following RTP in all positions except quarterbacks.20,31,34,126,128
Okoroha et al99 found that if the ACL graft failed, 79% of 24 NFL players who underwent revision ACL reconstruction returned to play at a mean of 12.6 months, with experience and skill associated with successful RTP and no effect on career longevity.
Collateral Ligaments
Two studies documented successful nonoperative treatment of isolated collateral ligament injuries up to grade 3, reporting faster RTP with lower-grade injuries and injuries managed nonoperatively.19,129 MRI was helpful in predicting time lost following injury.129
Articular Cartilage
Full-thickness cartilage lesions were common in NFL prospects, being found in 40% to 60% of players at the NFL Combine who underwent knee MRI.47,96 Most isolated cartilage lesions were in the patellofemoral compartment, and full-thickness cartilage lesions were more common in a compartment of the knee that underwent prior arthroscopic partial meniscectomy (APM), particularly laterally. In NFL Combine players with knee osteoarthritis based on plain radiographs or MRI, 27% had a history of APM, 24% ACL reconstruction, and 11% meniscal repair.132 History of knee surgery and body mass index ≥30 kg/m2 were associated with knee osteoarthritis. When players experienced articular cartilage injuries in the NFL, roughly 50% occurred during games, 50% involved linemen, 50% involved the medial femoral condyle, and 50% required eventual surgery.16 RTP was longer for operative versus nonoperative management (124 vs 36 days). Finally, according to a survey of team physicians regarding the management of chondral lesions, microfracture was favored the most (43%), followed by debridement (31%) and nonoperative treatment (13%).16
Several studies focused on treatment of articular cartilage injuries in NFL players, with chondroplasty with or without microfracture rates of 70% to 75% and with predictors of return rates being absence of microfracture and more presurgical games per season played.119,124,134 Finally, Tabacco et al135 studied 31 NFL players with knee osteoarthritis treated with autologous stem cell therapy and found that all players were satisfied with their treatment and that RTP occurred at a mean of 2.4 months.
Meniscus
Lateral meniscectomy resulted in 60% RTP in NFL players by 8 to 9 months after surgery, with more skilled and experienced players successfully returning and speed players less likely to return.2 Isolated APM resulted in fewer games played and a shortened career.13
Concomitant Injuries
One study of multiligament knee injuries identified through the NFLISS database (2000-2016) found RTP rates of 70% after combined ACL-MCL injuries, 55% RTP after ACL and posterior cruciate ligament and/or lateral collateral ligament injuries, and 50% RTP after frank knee dislocations.3
Other
Tejwani et al137 identified 24 players from a single NFL team (1993-2006) with Morel-Lavallee lesions, of which only 2 players missed 1 game each and all players were treated successfully with compression/cryotherapy/physical therapy (52%) or aspiration (48%). However, 20% of players required repeated aspirations, and 10% needed doxycycline sclerodesis when 3 aspirations failed to resolve the fluid collections. Quadriceps injuries most commonly occurred in defensive linemen and had only a 50% RTP rate, with return more successful in more talented players.7 In contrast, patellar tendon ruptures had an approximately 80% RTP rate, with return again favoring more talented players.6 Finally, a radiographic study of patellofemoral congruence in 132 athletes at the 2011 NFL Combine found incongruence in 10%, with an association of higher body mass index with patellofemoral incongruence but no association with quadriceps-to-hamstring strength ratios.18
Ankle Injuries
A history of ankle (and foot) injuries, particularly lateral sprains, was very common in NFL Combine participants (>70%), particularly in special teams players, WRs, and offensive linemen.59 Syndesmotic injuries were a topic of several studies in the NFL; they often occurred in special teams players and offensive linemen, with the mean number of days missed being just over 2 weeks when all grades were combined.59,103 Steroid injection of stable syndesmosis sprains led to early RTP by approximately 10 days, while higher-grade injuries with positive squeeze test were associated with longer RTP times.85,130 In a survey of NFL trainers in 1997, most used ice, electrical muscle stimulation, a cast and/or brace, and nonsteroidal anti-inflammatory drugs during the acute phase of the injury; proprioceptive training, ultrasound, and taping were the most common follow-up modalities. Recovery time was thought to be reduced by immobilization, corticosteroid injection, ice, and exercise.29
Isolated fibular fractures were found to require surgery in 50% of cases and allowed for faster RTP when isolated, but when treated with surgery, even isolated fractures required a mean of 10 weeks to RTP.144 In NFL athletes requiring ankle fracture fixation, superficial deltoid complex avulsion was a distinct injury that should be recognized, and these players might benefit from primary open repair.48
Finally, calf injuries have been studied in NFL players, and 75% were isolated to the gastrocnemius, 15% to the soleus, and 10% to both muscles.142 The mean time to RTP for calf injuries was 17 days, and 3 players required surgery. Larger fascial defects and the presence of fluid collection on MRI were associated with longer RTP.
Foot Injuries
Lisfranc Injuries
Kent et al62 reviewed 16 videos of tarsometatarsal injuries and found that these injuries typically occurred when a player was engaged with another player and when a combination of axial loading of a plantarflexed foot, external rotation, and pronation or supination occurred. Lisfranc sprains in NFL Combine participants were shown to negatively affect draft position and player availability, particularly when >2-mm residual displacement is present, while internet data of Lisfranc sprains in NFL players showed >90% RTP at a median of 11 months with no effect on performance or career length.90,91 Type 1 and 2 injuries were treated nonoperatively, with RTP within 1 week for grade 1 and at 5 weeks for grade 2, while grade 3 injuries required surgery but allowed eventual RTP.104
Achilles Tendon Ruptures
Several studies investigated Achilles tendon ruptures in NFL athletes, including data from the NFLISS, the internet, and individual surgeon studies. There were similar results based on all these data sets, with RTP occurring in 66% to 72% of players and various performance metrics being decreased for 2 to 3 years following repair.45,54,67,89,105,139
Fractures
Multiple studies investigated fifth metatarsal fractures in NFL Combine participants and NFL players. The incidence of this injury was approximately 2% in NFL Combine participants and was higher in athletes with long, straight, narrow fifth metatarsals and an adducted forefoot; 7% to 12% had nonunions after surgery versus 20% without surgery.22,69,76,116,140 There was a nonsignificant association with player availability in 1 study22 and no association in another,140 as well as a negative effect on performance.131 Successful completion of at least 1 college season after surgery for fifth metatarsal fracture decreased the likelihood of reinjury.117 Operative treatment was successful at maximizing RTP when it employed (1) a protocol of fixation with a Jones-specific intramedullary screw and iliac crest bone marrow aspirate with demineralized bone matrix injected at the fracture site, (2) noninvasive bone stimulators, (3) use of customized orthoses, and (4) an aggressive patient-specific rehabilitation protocol; however, 12% developed nonunion and required revision surgery when returning during the same season (at a mean of 9 weeks).69
Other
One study found that age, playing on artificial surface, and decreased ankle dorsiflexion were risk factors for turf toe in NFL players,115 while another study found that players with a history of turf toe had decreased first metatarsophalangeal dorsiflexion and higher peak hallucal pressures but no difference in peak first metatarsophalangeal pressures.12
Comparison of Overlapping Findings From the NFLISS vs Medical Records vs Internet-Based Studies
Cervical Disc Herniation
Hsu50 sought to describe outcomes of cervical disc herniation in NFL athletes and, using the internet, was able to identify 99 players with cervical disc herniations over 30 seasons (1979-2008), or 3.3 cases per year. In contrast, Gray et al44 used NFLISS data and found 61 cervical herniations over 12 seasons (2000-2012), or 5.1 cases per year. No studies of cervical disc herniation utilized team medical record data. Although many remote cases were likely missed by Hsu using an internet search and despite the fact that the number of teams in the NFL has increased since 1979, the disparity between the 2 sources of data suggests that the medical information on NFL players available via the internet is likely incomplete.
Lumbar Disc Herniation
Two studies contained overlapping data regarding lumbar disc herniation.44,141 Weistroffer and Hsu141 used internet search methods to identify lumbar disc herniations in NFL linemen and found 66 cases from 1982 to 2009 (approximately 2.4 cases per year). In contrast, Gray et al44 used NFLISS data to identify lumbar disc herniations and found 83 cases in linemen from 2000 to 2012 (6.9 cases per year).44 This suggests that a large number of cases are missed with information from the public domain and introduces bias into the internet-based study. No studies of lumbar disc herniation utilized team medical record data.
Achilles Tendon Repair
Five studies collected internet-based data and found 31 to 172 ruptures in NFL players; however, there was much variation in the period for data extraction (2-58 years).45,54,67,105,139 Two of these studies reported RTP rate, which ranged from 66% to 72% and was similar to a study by McCullough et al,89 who found that 78% returned to play after mini-open repair according to medical record data from a single surgeon’s practice.54,105 No studies on Achilles tendon ruptures utilized data from the NFLISS.
ACL Injuries
Multiple studies used the internet or NFLISS to identify ACL tears in certain NFL populations, affording an opportunity to determine the ability of an internet search to capture a given player population.9,20,24,26,31,57 Three studies provided data regarding the number of RBs and WRs experiencing ACL tears over a defined period.9,20,26 Using the NFLISS, Bradley et al9 searched the years 1994 to 1998 (5 seasons) and found 39 ACL tears among RBs and WRs, while Dodson et al26 found 57 ACL tears in RBs and WRs from 2010 to 2013 (4 seasons). In contrast, Cary et al20 found 33 ACL tears in these positions using the internet for the 5 seasons from 1998 to 2002.
In another set of studies focusing on a different position, Cinque et al24 used the internet to identify ACL tears in linemen and, over the 6 seasons from 2010 to 2015, found 38 ACL tears. In comparison, Bradley et al9 found 57 ACL tears in these positions in their study using the NFLISS over 5 seasons, and Dodson et al26 found 56 tears over 4 seasons, also using the NFLISS. Finally, in 2 studies using the internet to identify all NFL ACL tears over the same period, Eisenstein et al31 found 92 cases in the 2013 and 2014 seasons, while Johnston et al57 found 108 ACL tears during those same 2 seasons.
Taken together, these findings imply that (1) an internet search is likely to miss eligible participants; (2) higher-profile players, such as RBs and WRs, may be more easily identified via an internet search; (3) internet searches to identify ACL tears at lower-profile positions, such as linemen, may miss a significant number of cases with a risk of spurious findings; and (4) differences in internet search methods may lead to many eligible cases being missed. No studies on ACL injuries extracted data from medical records.
Discussion
This systematic review provides a comprehensive summary of the orthopaedic literature involving NFL players. Most studies examined knee, spine, and shoulder injuries in NFL players, and the majority of articles were level 4 evidence. The most common sources of data were the NFL Combine database, internet, and NFLISS.
Orthopaedic injuries in NFL players occurred more often during games than practices and led to decreased performance.4,35 Injuries to the trunk were rare, with only 1 chondral rib fracture reported per year.87 Spine injuries accounted for 7% of all injuries in NFL players.82 Preexisting cervical spine conditions resulted in fewer games played but were not associated with diminished performance.122 Cervical pathology failing nonoperative management was often treated with ACDF or foraminotomy, depending on the pathoanatomy and symptom complex. About 70% of players returned to play after ACDF; however, later adjacent segment degeneration occurred in 10% of players.93 The RTP rate after foraminotomy (92%) was higher than that after ACDF, although 50% of players required another operation.80 Players with a history of lumbar spine conditions were less likely to be drafted, but when they were drafted, their career longevity and performance were not affected.123
Shoulder injuries were fairly common in football players, with about 50% of recruits at the NFL Combine reporting a history of shoulder injury. Shoulder injuries occurred most often during passing plays and as a result of direct trauma.58 AC separation and anterior instability were the most common types of shoulder injuries, and the rate of RTP was as high as 90% after shoulder surgery (rotator cuff repair and surgery for clavicle fractures and shoulder instability).38,55,61,145 Most hand injuries were fractures and dislocations; elbow and wrist injuries were primarily ligamentous; and forearm injuries were fractures.21,83
Hip injuries accounted for only 3% of all injuries in NFL players and were mainly muscle strains.36 Most NFL players returned to play within 1 to 2 weeks of treatment for thigh injuries, but only 50% returned following complete proximal hamstring avulsion and quadriceps injuries.7,32,75,86 About 50% of players at the NFL Combine reported a history of knee injury, primarily MCL, meniscal, and ACL injuries.8 Team physicians preferred patellar tendon autograft for ACL reconstruction.9,33,88 About 60% of players returned to play after ACL reconstruction, and performance seemed to diminish after surgery.60,128 About 40% to 60% of players at the NFL Combine had full-thickness cartilage lesions on MRI, and 46% of NFL players with articular cartilage injuries required surgery and took longer to RTP than those treated nonoperatively.16,96
About 70% of players at the NFL Combine had a history of ankle injuries, with lateral and syndesmotic sprains, metatarsophalangeal dislocations, and fibular fractures being the most common.59 Sixty eight percent of players returned to play following Achilles tendon rupture.105 Type 1 (undisplaced) and type 2 (2 mm or less of widening vs the opposite side on weightbearing bilateral radiographs) Lisfranc injuries were treated nonoperatively, with RTP within 1 week for grade 1 and at 5 weeks for grade 2, while grade 3 (≥3 mm of widening) required surgery (open reduction internal fixation without fusion, with optional removal of hardware at approximately 4-6 months) but allowed for eventual RTP.104 Care must also be taken to recognize proximal Lisfranc variants with any degree of widening between the medial and middle cuneiform, and these were commonly treated with internal fixation.
One strength of this study is that it is the first systematic review, to our knowledge, that has examined the range of orthopaedic injuries in NFL players. This systematic review provides National Collegiate Athletic Association (NCAA) and NFL team physicians with the most up-to-date information regarding the frequency and outcomes of orthopaedic injuries in professional football players. There are several limitations of this systematic review. Very few studies have been published for certain types of orthopaedic injuries in NFL players, such as trunk injuries. This may be due to the rarity of these types of injuries. The majority of studies provided lower-quality evidence (level 3 or 4); however, this seems appropriate, as all of the included studies examined descriptive data pertaining to injuries in NFL players. Multiple studies in this review collected their data by performing an internet-based search of publicly available data (eg, injury reports, player profiles, press releases). Data collected in this fashion were not standardized and may produce unreliable estimates. Also, publically available data are very limited and do not provide access to detailed medical records and demographics of the players. We found that 17% of studies collected data from a single team only; therefore, the results of these studies may not be generalizable to all NFL players. We also found that 10% of studies conducted a survey of team physicians and/or athletic trainers. Survey data are subject to recall bias (ie, information is misremembered) and nonresponse (ie, all questions are not completed or all respondents do not complete the survey).
In conclusion, this systematic review provides the NCAA and NFL team physicians with a single source of the most current literature regarding orthopedic injuries in NFL players.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson, Jr, Foundation. L.J.B. has received funding for education from Arthrex, royalties from Zimmer Biomet, and hospitality payments from Prodigy Surgical Distribution.
References
- 1. Armsey TD, Hosey RG. Medical aspects of sports: epidemiology of injuries, preparticipation physical examination, and drugs in sports. Clin Sports Med. 2004;23(2):255–279. [DOI] [PubMed] [Google Scholar]
- 2. Aune KT, Andrews JR, Dugas JR, Cain EL., Jr Return to play after partial lateral meniscectomy in National Football League athletes. Am J Sports Med. 2014;42(8):1865–1872. [DOI] [PubMed] [Google Scholar]
- 3. Bakshi N, Khan M, Finney FT, Stotts J, Sikka RS, Bedi A. Return to play after multi-ligament knee injuries in National Football League (NFL) athletes. Paper presented at: AOSSM 2017; June 20-23, 2017; Toronto, Canada. [Google Scholar]
- 4. Beaulieu-Jones BR, Rossy WH, Sanchez G. et al. Epidemiology of injuries identified at the NFL Scouting Combine and their impact on performance in the National Football League: evaluation of 2203 athletes from 2009 to 2015. Orthop J Sports Med. 2017;5(7):2325967117708744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bedi A, Warren RF, Wojtys EM. et al. Restriction in hip internal rotation is associated with an increased risk of ACL injury. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):2024–2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boublik M, Schlegel T, Koonce R, Genuario J, Lind C, Hamming D. Patellar tendon ruptures in National Football League players. Am J Sports Med. 2011;39(11):2436–2440. [DOI] [PubMed] [Google Scholar]
- 7. Boublik M, Schlegel TF, Koonce RC, Genuario JW, Kinkartz JD. Quadriceps tendon injuries in National Football League players. Am J Sports Med. 2013;41(8):1841–1846. [DOI] [PubMed] [Google Scholar]
- 8. Bradley J, Honkamp NJ, Jost P, West R, Norwig J, Kaplan LD. Incidence and variance of knee injuries in elite college football players. Am J Orthop (Belle Mead NJ). 2008;37(6):310–314. [PubMed] [Google Scholar]
- 9. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18(5):502–509. [DOI] [PubMed] [Google Scholar]
- 10. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine—trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22–27. [DOI] [PubMed] [Google Scholar]
- 11. Brophy RH, Chehab EL, Barnes RP, Lyman S, Rodeo SA, Warren RF. Predictive value of orthopedic evaluation and injury history at the NFL Combine. Med Sci Sports Exerc. 2008;40(8):1368–1372. [DOI] [PubMed] [Google Scholar]
- 12. Brophy RH, Gamradt SC, Ellis SJ. et al. Effect of turf toe on foot contact pressures in professional American football players. Foot Ankle Int. 2009;30(5):405–409. [DOI] [PubMed] [Google Scholar]
- 13. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: a case control study. Am J Sports Med. 2009;37(11):2102–2107. [DOI] [PubMed] [Google Scholar]
- 14. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of shoulder stabilization on career length in National Football League athletes. Am J Sports Med. 2011;39(4):704–709. [DOI] [PubMed] [Google Scholar]
- 15. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768–775. [DOI] [PubMed] [Google Scholar]
- 16. Brophy RH, Rodeo SA, Barnes RP, Powell JW, Warren RF. Knee articular cartilage injuries in the National Football League: epidemiology and treatment approach by team physicians. J Knee Surg. 2009;22(4):331–338. [DOI] [PubMed] [Google Scholar]
- 17. Brophy RH, Wright RW, Powell JW, Matava MJ. Injuries to kickers in American football: the National Football League experience. Am J Sports Med. 2010;38(6):1166–1173. [DOI] [PubMed] [Google Scholar]
- 18. Brown CA, Carragee C, Sox-Harris A, Merchant AC, McAdams TR. Prevalence of abnormal patellofemoral congruence in elite American football players and association with quadriceps isokinetic testing. J Knee Surg. 2014;27(1):47–52. [DOI] [PubMed] [Google Scholar]
- 19. Bushnell BD, Bitting SS, Crain JM, Boublik M, Schlegel TF. Treatment of magnetic resonance imaging—documented isolated grade III lateral collateral ligament injuries in National Football League athletes. Am J Sports Med. 2010;38(1):86–91. [DOI] [PubMed] [Google Scholar]
- 20. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911–1917. [DOI] [PubMed] [Google Scholar]
- 21. Carlisle JC, Goldfarb CA, Mall N, Powell JW, Matava MJ. Upper extremity injuries in the National Football League, part II: elbow, forearm, and wrist injuries. Am J Sports Med. 2008;36(10):1945–1952. [DOI] [PubMed] [Google Scholar]
- 22. Carreira DS, Sandilands SM. Radiographic factors and effect of fifth metatarsal Jones and diaphyseal stress fractures on participation in the NFL. Foot Ankle Int. 2013;34(4):518–522. [DOI] [PubMed] [Google Scholar]
- 23. Chambers CC, Lynch TS, Gibbs DB. et al. Superior labrum anterior-posterior tears in the National Football League. Am J Sports Med. 2017;45(1):167–172. [DOI] [PubMed] [Google Scholar]
- 24. Cinque ME, Hannon CP, Bohl DD. et al. Return to sport and performance after anterior cruciate ligament reconstruction in National Football League linemen. Orthop J Sports Med. 2017;5(6):2325967117711681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cohen SB, Towers JD, Bradley JP. Rotator cuff contusions of the shoulder in professional football players: epidemiology and magnetic resonance imaging findings. Am J Sports Med. 2007;35(3):442–447. [DOI] [PubMed] [Google Scholar]
- 26. Dodson CC, Secrist ES, Bhat SB, Woods DP, Deluca PF. Anterior cruciate ligament injuries in National Football League athletes from 2010 to 2013: a descriptive epidemiology study. Orthop J Sports Med. 2016;4(3):2325967116631949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Domb BG, Carter C, Finch NA, Hammarstedt JE, Dunne KF, Stake CE. Whole-person impairment in younger retired NFL players: the orthopaedic toll of a professional football career. Orthop J Sports Med. 2014;2(5):2325967114534824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Domb BG, Jackson TJ, Carter CC, Jester JR, Finch NA, Stake CE. Magnetic resonance imaging findings in the symptomatic hips of younger retired National Football League players. Am J Sports Med. 2014;42(7):1704–1709. [DOI] [PubMed] [Google Scholar]
- 29. Doughtie M. Syndesmotic ankle sprains in football: a survey of National Football League athletic trainers. J Athl Train. 1999;34(1):15–18. [PMC free article] [PubMed] [Google Scholar]
- 30. Drakos M, Birmingham P, Delos D. et al. Corticosteroid and anesthetic injections for muscle strains and ligament sprains in the NFL. HSS J. 2014;10(2):136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Eisenstein ED, Rawicki NL, Rensing NJ, Kusnezov NA, Lanzi JT. Variables affecting return to play after anterior cruciate ligament injury in the National Football League. Orthop J Sports Med. 2016;4(10):2325967116670117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843–850. [DOI] [PubMed] [Google Scholar]
- 33. Erickson BJ, Harris JD, Fillingham YA. et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30(6):731–738. [DOI] [PubMed] [Google Scholar]
- 34. Erickson BJ, Harris JD, Heninger JR. et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728–e734. [DOI] [PubMed] [Google Scholar]
- 35. Feeley BT, Kennelly S, Barnes RP. et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597–1603. [DOI] [PubMed] [Google Scholar]
- 36. Feeley BT, Powell JW, Muller MS, Barnes RP, Warren RF, Kelly BT. Hip injuries and labral tears in the National Football League. Am J Sports Med. 2008;36(11):2187–2195. [DOI] [PubMed] [Google Scholar]
- 37. Finstein JL, Cohen SB, Dodson CC. et al. Triceps tendon ruptures requiring surgical repair in National Football League players. Orthop J Sports Med. 2015;3(8):2325967115601021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Foulk DA, Darmelio MP, Rettig AC, Misamore G. Full-thickness rotator-cuff tears in professional football players. Am J Orthop (Belle Mead NJ). 2002;31(11):622–624. [PubMed] [Google Scholar]
- 39. Frangiamore S, Mannava S, Sanchez G. et al. Shoulder injuries in collegiate football athletes: impact on draft status and professional performance. Paper presented at: AOSSM 2017; June 20-23, 2017; Toronto, Canada. [Google Scholar]
- 40. Gamradt SC, Brophy RH, Barnes R, Warren RF, Thomas Byrd JW, Kelly BT. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37(7):1370–1374. [DOI] [PubMed] [Google Scholar]
- 41. Gibbs DB, Lynch TS, Gombera MM. et al. Preexisting rotator cuff tears as a predictor of outcomes in National Football League athletes. Sports Health. 2016;8(3):250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6(5):638–643. [DOI] [PubMed] [Google Scholar]
- 43. Gray B, Buchowski JM, Bumpass DB, Mall NA, Matava MJ. Spinal injuries in professional American football players. Paper presented at: 27th Annual Meeting of the North American Spine Society; October 24-27, 2012; Dallas, Texas. [Google Scholar]
- 44. Gray BL, Buchowski JM, Bumpass DB, Lehman RA, Jr, Mall NA, Matava MJ. Disc herniations in the National Football League. Spine (Phila Pa 1976). 2013;38(22):1934–1938. [PubMed] [Google Scholar]
- 45. Greenfield S, Anderson R. Return to play after mini-open repair of Achilles tendon ruptures in the NFL athlete. Paper presented at: AOFAS Annual Meeting 2017; July 12-15, 2017; Seattle, Washington. [Google Scholar]
- 46. Hershman EB, Anderson R, Bergfeld JA. et al. An analysis of specific lower extremity injury rates on grass and FieldTurf playing surfaces in National Football League Games: 2000-2009 seasons. Am J Sports Med. 2012;40(10):2200–2205. [DOI] [PubMed] [Google Scholar]
- 47. Hirshorn KC, Cates T, Gillogly S. Magnetic resonance imaging-documented chondral injuries about the knee in college football players: 3-year National Football League Combine data. Arthroscopy. 2010;26(9):1237–1240. [DOI] [PubMed] [Google Scholar]
- 48. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int. 2015;36(11):1272–1278. [DOI] [PubMed] [Google Scholar]
- 49. Hsu JC, Fischer DA, Wright RW. Proximal rectus femoris avulsions in National Football League kickers: a report of 2 cases. Am J Sports Med. 2005;33(7):1085–1087. [DOI] [PubMed] [Google Scholar]
- 50. Hsu WK. Outcomes following nonoperative and operative treatment for cervical disc herniations in National Football League athletes. Spine (Phila Pa 1976). 2011;36(10):800–805. [DOI] [PubMed] [Google Scholar]
- 51. Hsu WK. Performance-based outcomes following lumbar discectomy in professional athletes in the National Football League. Spine (Phila Pa 1976). 2010;35(12):1247–1251. [DOI] [PubMed] [Google Scholar]
- 52. Hsu WK, McCarthy KJ, Savage JW. et al. The Professional Athlete Spine Initiative: outcomes after lumbar disc herniation in 342 elite professional athletes. Spine J. 2011;11(3):180–186. [DOI] [PubMed] [Google Scholar]
- 53. Jack RA, Evans DC, Echo A. et al. Performance and return to sport after sports hernia surgery in NFL players. Orthop J Sports Med. 2017;5(4):2325967117699590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jack RA, 2nd, Sochacki KR, Gardner SS. et al. Performance and return to sport after Achilles tendon repair in National Football League players. Foot Ankle Int. 2017;38(10):1092–1099. [DOI] [PubMed] [Google Scholar]
- 55. Jack RA, 2nd, Sochacki KR, Navarro SM, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after clavicle open reduction and internal fixation in National Football League players. Orthop J Sports Med. 2017;5(8):2325967117720677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jack RA, 2nd, Sochacki KR, Navarro SM, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after nonoperative treatment of clavicle fractures in National Football League players. Orthopedics. 2017;40(5):e836–e843. [DOI] [PubMed] [Google Scholar]
- 57. Johnston JT, Mandelbaum BR, Schub D. et al. Video analysis of anterior cruciate ligament tears in professional American football athletes. Am J Sports Med. 2018;46(4):862–868. [DOI] [PubMed] [Google Scholar]
- 58. Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33(8):1142–1146. [DOI] [PubMed] [Google Scholar]
- 59. Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop (Belle Mead NJ). 2011;40(1):40–44. [PubMed] [Google Scholar]
- 60. Keller RA, Mehran N, Austin W, Marshall NE, Bastin K, Moutzouros V. Athletic performance at the NFL Scouting Combine after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(12):3022–3026. [DOI] [PubMed] [Google Scholar]
- 61. Kelly BT, Barnes RP, Powell JW, Warren RF. Shoulder injuries to quarterbacks in the National Football League. Am J Sports Med. 2004;32(2):328–331. [DOI] [PubMed] [Google Scholar]
- 62. Kent RW, Lievers WB, Riley PO, Frimenko RE, Crandall JR. Etiology and biomechanics of tarsometatarsal injuries in professional football players: a video analysis. Orthop J Sports Med. 2014;2(3):2325967114525347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kenter K, Behr CT, Warren RF, O’Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elbow Surg. 2000;9(1):1–5. [DOI] [PubMed] [Google Scholar]
- 64. Knapik DM, Gebhart JJ, Nho SJ, Tanenbaum JE, Voos JE, Salata MJ. Prevalence of surgical repair for athletic pubalgia and impact on performance in football athletes participating in the National Football League Combine. Arthroscopy. 2017;33(5):1044–1049. [DOI] [PubMed] [Google Scholar]
- 65. Knapik DM, Gebhart JJ, Sheehan J, Tanenbaum JE, Salata MJ, Voos JE. Recurrent labral tearing on magnetic resonance imaging is not predictive of diminished participation among National Football League athletes. Arthroscopy. 2018;34(1):66–72. [DOI] [PubMed] [Google Scholar]
- 66. Knapik DM, Gillespie RJ, Salata MJ, Voos JE. Prevalence and impact of glenoid augmentation in American football athletes participating in the National Football League Scouting Combine. Orthop J Sports Med. 2017;5(8):2325967117722945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Krill MK, Borchers JR, Hoffman JT, Krill ML, Hewett TE. Effect of position, time in the season, and playing surface on Achilles tendon ruptures in NFL games: a 2009-10 to 2016-17 review. Phys Sportsmed. 2017;45(3):259–264. [DOI] [PubMed] [Google Scholar]
- 68. Krych AJ, Richman D, Drakos M. et al. Epidural steroid injection for lumbar disc herniation in NFL athletes. Med Sci Sports Exerc. 2012;44(2):193–198. [DOI] [PubMed] [Google Scholar]
- 69. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37(1):8–16. [DOI] [PubMed] [Google Scholar]
- 70. Larson CM, Sikka RS, Sardelli MC. et al. Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate National Football League prospects. Arthroscopy. 2013;29(3):405–410. [DOI] [PubMed] [Google Scholar]
- 71. Lawrence DW, Comper P, Hutchison MG. Influence of extrinsic risk factors on National Football League injury rates. Orthop J Sports Med. 2016;4(3):2325967116639222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012-2014. Orthop J Sports Med. 2015;3(5):2325967115583653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. LeBus GF, Chahla J, Sanchez G. et al. The Latarjet procedure at the National Football League Scouting Combine: an imaging and performance analysis. Orthop J Sports Med. 2017;5(9):2325967117726045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Leclere LE, Asnis PD, Griffith MH, Granito D, Berkson EM, Gill TJ. Shoulder instability in professional football players. Sports Health. 2013;5(5):455–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT., 3rd Intramuscular corticosteroid injection for hamstring injuries: a 13-year experience in the National Football League. Am J Sports Med. 2000;28(3):297–300. [DOI] [PubMed] [Google Scholar]
- 76. Low K, Noblin JD, Browne JE, Barnthouse CD, Scott AR. Jones fractures in the elite football player. J Surg Orthop Adv. 2004;13(3):156–160. [PubMed] [Google Scholar]
- 77. Lynch TS, Saltzman MD, Ghodasra JH, Bilimoria KY, Bowen MK, Nuber GW. Acromioclavicular joint injuries in the National Football League: epidemiology and management. Am J Sports Med. 2013;41(12):2904–2908. [DOI] [PubMed] [Google Scholar]
- 78. Lynch TS, Schroeder G, Gibbs D. et al. Lumbar spine injury/pathology as a predictor of outcomes in National Football League athletes. Orthop J Sports Med. 2014;2(suppl 2):2325967114S00077. [DOI] [PubMed] [Google Scholar]
- 79. Mai HT, Alvarez AP, Freshman RD. et al. The NFL Orthopaedic Surgery Outcomes Database (NO-SOD): the effect of common orthopaedic procedures on football careers. Am J Sports Med. 2016;44(9):2255–2262. [DOI] [PubMed] [Google Scholar]
- 80. Mai HT, Burgmeier RJ, Mitchell SM. et al. Does the level of cervical disc herniation surgery affect performance-based outcomes in National Football League athletes? Spine (Phila Pa 1976). 2016;41(23):1785–1789. [DOI] [PubMed] [Google Scholar]
- 81. Mair SD, Isbell WM, Gill TJ, Schlegel TF, Hawkins RJ. Triceps tendon ruptures in professional football players. Am J Sports Med. 2004;32(2):431–434. [DOI] [PubMed] [Google Scholar]
- 82. Mall NA, Buchowski J, Zebala L, Brophy RH, Wright RW, Matava MJ. Spine and axial skeleton injuries in the National Football League. Am J Sports Med. 2012;40(8):1755–1761. [DOI] [PubMed] [Google Scholar]
- 83. Mall NA, Carlisle JC, Matava MJ, Powell JW, Goldfarb CA. Upper extremity injuries in the National Football League, part I: hand and digital injuries. Am J Sports Med. 2008;36(10):1938–1944. [DOI] [PubMed] [Google Scholar]
- 84. Mall NA, Matava MJ, Wright RW, Brophy RH. Relation between anterior cruciate ligament graft obliquity and knee laxity in elite athletes at the National Football League Combine. Arthroscopy. 2012;28(8):1104–1113. [DOI] [PubMed] [Google Scholar]
- 85. Mansour A, Porter DA, Young JP, Hammer D, Boublik M, Schlegel TF. Corticosteroid injections hasten return to play of National Football League players following stable ankle syndesmosis sprains. Orthop J Sports Med. 2013;1(4 suppl 1):2325967113S00023. [Google Scholar]
- 86. Mansour AA, 3rd, Genuario JW, Young JP, Murphy TP, Boublik M, Schlegel TF. National Football League athletes’ return to play after surgical reattachment of complete proximal hamstring ruptures. Am J Orthop (Belle Mead NJ). 2013;42(6):e38–e41. [PubMed] [Google Scholar]
- 87. McAdams TR, Deimel JF, Ferguson J, Beamer BS, Beaulieu CF. Chondral rib fractures in professional American football: two cases and current practice patterns among NFL team physicians. Orthop J Sports Med. 2016;4(2):2325967115627623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. McCarty EC, Kraeutler MJ, Langner P, Cook S, Ellis B, Godfrey JM. Historical patterns and variation in treatment of injuries in NFL (National Football League) players and NCAA (National Collegiate Athletic Association) Division I football players. Am J Orthop (Belle Mead NJ). 2016;45(6):e319–e327. [PubMed] [Google Scholar]
- 89. McCullough KA, Shaw CM, Anderson RB. Mini-open repair of Achilles rupture in the National Football League. J Surg Orthop Adv. 2014;23(4):179–183. [PubMed] [Google Scholar]
- 90. McHale KJ, Rozell JC, Milby AH, Carey JL, Sennett BJ. Outcomes of Lisfranc injuries in the National Football League. Am J Sports Med. 2016;44(7):1810–1817. [DOI] [PubMed] [Google Scholar]
- 91. McHale KJ, Vopat BG, Beaulieu-Jones BR. et al. Epidemiology and outcomes of Lisfranc injuries identified at the National Football League scouting combine. Am J Sports Med. 2017;45(8):1901–1908. [DOI] [PubMed] [Google Scholar]
- 92. Menge TJ, Bhatia S, McNamara SC, Briggs KK, Philippon MJ. Femoroacetabular impingement in professional football players: return to play and predictors of career length after hip arthroscopy. Am J Sports Med. 2017;45(8):1740–1744. [DOI] [PubMed] [Google Scholar]
- 93. Meredith DS, Jones KJ, Barnes R, Rodeo SA, Cammisa FP, Warren RF. Operative and nonoperative treatment of cervical disc herniation in National Football League athletes. Am J Sports Med. 2013;41(9):2054–2058. [DOI] [PubMed] [Google Scholar]
- 94. Morgan RJ, Bankston LS, Jr, Hoenig MP, Connor PM. Evolving management of middle-third clavicle fractures in the National Football League. Am J Sports Med. 2010;38(10):2092–2096. [DOI] [PubMed] [Google Scholar]
- 95. Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28(10):1396–1403. [DOI] [PubMed] [Google Scholar]
- 96. Nepple JJ, Wright RW, Matava MJ, Brophy RH. Full-thickness knee articular cartilage defects in National Football League Combine athletes undergoing magnetic resonance imaging: prevalence, location, and association with previous surgery. Arthroscopy. 2012;28(6):798–806. [DOI] [PubMed] [Google Scholar]
- 97. Nicholas SJ, Nicholas JA, Nicholas C, Diecchio JR, McHugh MP. The health status of retired American football players: Super Bowl III revisited. Am J Sports Med. 2007;35(10):1674–1679. [DOI] [PubMed] [Google Scholar]
- 98. Nwachukwu BU, Bedi A, Premkumar A, Draovitch P, Kelly BT. Characteristics and outcomes of arthroscopic femoroacetabular impingement surgery in the National Football League. Am J Sports Med. 2018;46(1):144–148. [DOI] [PubMed] [Google Scholar]
- 99. Okoroha KR, Kadri O, Keller RA, Marshall N, Cizmic Z, Moutzouros V. Return to play after revision anterior cruciate ligament reconstruction in National Football League players. Orthop J Sports Med. 2017;5(4):2325967117698788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Okoroha KR, Taylor KA, Marshall NE. et al. Return to play after shoulder instability in National Football League athletes. J Shoulder Elbow Surg. 2018;27(1):17–22. [DOI] [PubMed] [Google Scholar]
- 101. Olson DE, Sikka RS, Hamilton A, Krohn A. Football injuries: current concepts. Curr Sports Med Rep. 2011;10(5):290–298. [DOI] [PubMed] [Google Scholar]
- 102. Orchard JW, Powell JW. Risk of knee and ankle sprains under various weather conditions in American football. Med Sci Sports Exerc. 2003;35(7):1118–1123. [DOI] [PubMed] [Google Scholar]
- 103. Osbahr DC, Drakos MC, O’Loughlin PF. et al. Syndesmosis and lateral ankle sprains in the National Football League. Orthopedics. 2013;36(11):e1378–e1384. [DOI] [PubMed] [Google Scholar]
- 104. Osbahr DC, O’Loughlin PF, Drakos MC, Barnes RP, Kennedy JG, Warren RF. Midfoot sprains in the National Football League. Am J Orthop (Belle Mead NJ). 2014;43(12):557–561. [PubMed] [Google Scholar]
- 105. Parekh SG, Wray WH, 3rd, Brimmo O, Sennett BJ, Wapner KL. Epidemiology and outcomes of Achilles tendon ruptures in the National Football League. Foot Ankle Spec. 2009;2(6):283–286. [DOI] [PubMed] [Google Scholar]
- 106. Paxton ES, Moorman CT, Chehab EL, Barnes RP, Warren RF, Brophy RH. Effect of hyperconcavity of the lumbar vertebral endplates on the playing careers of professional American football linemen. Am J Sports Med. 2010;38(11):2255–2258. [DOI] [PubMed] [Google Scholar]
- 107. Powell JW. Incidence of injury associated with playing surfaces in the National Football League 1980-1985. J Athl Train. 1987;22:202–206. [Google Scholar]
- 108. Powell JW, Schootman M. A multivariate risk analysis of selected playing surfaces in the National Football League: 1980 to 1989. An epidemiologic study of knee injuries. Am J Sports Med. 1992;20(6):686–694. [DOI] [PubMed] [Google Scholar]
- 109. Presciutti S, Schweitzer KM, DeLuca P, Marchetto P, Wilsey JT, Vaccaro AR. Assessment of cervical spine canal geometry by football position in athletes in the NFL Scouting Combine. Orthopedics. 2008;31(11):1–7. [Google Scholar]
- 110. Presciutti SM, DeLuca P, Marchetto P, Wilsey JT, Shaffrey C, Vaccaro AR. Mean subaxial space available for the cord index as a novel method of measuring cervical spine geometry to predict the chronic stinger syndrome in American football players. J Neurosurg Spine. 2009;11(3):264–271. [DOI] [PubMed] [Google Scholar]
- 111. Price MD, Rossy WH, Sanchez G, McHale KJ, Logan C, Provencher MT. The epidemiology of injuries identified at the National Football League Scouting Combine and their impact on professional sport performance: 2203 athletes, 2009-2015. Paper presented at: AOSSM 2017; June 20-23, 2017; Toronto, Canada. [Google Scholar]
- 112. Raab DJ, Fischer DA, Quick DC. Lunate and perilunate dislocations in professional football players: a five-year retrospective analysis. Am J Sports Med. 1994;22(6):841–845. [DOI] [PubMed] [Google Scholar]
- 113. Read CR, Aune KT, Cain EL, Jr, Fleisig GS. Return to play and decreased performance after anterior cruciate ligament reconstruction in National Football League defensive players. Am J Sports Med. 2017;45(8):1815–1821. [DOI] [PubMed] [Google Scholar]
- 114. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Rodeo SA, O’Brien S, Warren RF, Barnes R, Wickiewicz TL, Dillingham MF. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med. 1990;18(3):280–285. [DOI] [PubMed] [Google Scholar]
- 116. Rosenbaum A, DeSandis BA, Warren R, Taylor SA, Murphy C, Drakos MC. Can fifth metatarsal morphology predict proximal fifth metatarsal fracture risk? A radiographic analysis of National Football League players. Paper presented at: AOFAS Annual Meeting 2016; July 21-23, 2016; Toronto, Canada. [Google Scholar]
- 117. Ross J, Brophy RH, Wright RW. The elite football players with a fifth metatarsal fracture. Orthop J Sports Med. 2013;1(suppl 4):2325967113S00020. [Google Scholar]
- 118. Savage JW, Hsu WK. Statistical performance in National Football League athletes after lumbar discectomy. Clin J Sport Med. 2010;20(5):350–354. [DOI] [PubMed] [Google Scholar]
- 119. Schallmo M, Singh SK, Freshman R, Barth K, Mai H, Hsu W. Performance-based outcomes among American professional athletes following microfracture of the knee: a cross-sport analysis. Paper presented at: AOSSM 2017; June 20-23, 2017; Toronto, Canada. [Google Scholar]
- 120. Schlegel TF, Bushnell BD, Godfrey J, Boublik M. Success of nonoperative management of adductor longus tendon ruptures in National Football League athletes. Am J Sports Med. 2009;37(7):1394–1399. [DOI] [PubMed] [Google Scholar]
- 121. Schroeder GD, Lynch TS, Gibbs DB. et al. Does a lumbar disc herniation affect performance-based outcomes in National Football League athletes? Paper presented at: North American Spine Society 29th Annual Meeting; November 12-15, 2014; San Francisco, California. [Google Scholar]
- 122. Schroeder GD, Lynch TS, Gibbs DB. et al. The impact of a cervical spine diagnosis on the careers of National Football League athletes. Spine (Phila Pa 1976). 2014;39(12):947–952. [DOI] [PubMed] [Google Scholar]
- 123. Schroeder GD, Lynch TS, Gibbs DB. et al. Pre-existing lumbar spine diagnosis as a predictor of outcomes in National Football League athletes. Am J Sports Med. 2015;43(4):972–978. [DOI] [PubMed] [Google Scholar]
- 124. Scillia AJ, Aune KT, Andrachuk JS. et al. Return to play after chondroplasty of the knee in National Football League athletes. Am J Sports Med. 2015;43(3):663–668. [DOI] [PubMed] [Google Scholar]
- 125. Scranton PE, Jr, Whitesel JP, Powell JW. et al. A review of selected noncontact anterior cruciate ligament injuries in the National Football League. Foot Ankle Int. 1997;18(12):772–776. [DOI] [PubMed] [Google Scholar]
- 126. Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes. Orthop J Sports Med. 2016;4(8):2325967116663921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Shaffer B, Wiesel S, Lauerman W. Spondylolisthesis in the elite football player: an epidemiologic study in the NCAA and NFL. J Spinal Disord. 1997;10(5):365–370. [PubMed] [Google Scholar]
- 128. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38(11):2233–2239. [DOI] [PubMed] [Google Scholar]
- 129. Sikka RS, Dhami R, Dunlay R, Boyd JL. Isolated fibular collateral ligament injuries in athletes. Sports Med Arthrosc. 2015;23(1):17–21. [DOI] [PubMed] [Google Scholar]
- 130. Sikka RS, Fetzer GB, Sugarman E. et al. Correlating MRI findings with disability in syndesmotic sprains of NFL players. Foot Ankle Int. 2012;33(5):371–378. [DOI] [PubMed] [Google Scholar]
- 131. Singh SK, Larkin KE, Kadakia AR, Hsu WK. Risk factors for reoperation and performance-based outcomes after operative fixation of foot fractures in the professional athlete: a cross-sport analysis. Sports Health. 2018;10(1):70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Smith MV, Nepple JJ, Wright RW, Matava MJ, Brophy RH. Knee osteoarthritis is associated with previous meniscus and anterior cruciate ligament surgery among elite college American football athletes. Sports Health. 2017;9(3):247–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Sochacki KR, Jack RA, 2nd, Nauert R. et al. Performance and return to sport after thumb ulnar collateral ligament surgery in National Football League players. Hand (N Y). 2019;14(4):487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Steadman JR, Miller BS, Karas SG, Schlegel TF, Briggs KK, Hawkins RJ. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16(2):83–86. [PubMed] [Google Scholar]
- 135. Tabacco J, Lamour RJ, Hackel JG, Andrews JR, Milchteim C. Outcomes of autologous stem cell therapy for knee osteoarthritis in National Football League players. Paper presented at: American Medical Society for Sports Medicine 2015 Annual Meeting; April 14-19, 2015; Hollywood, Florida. [Google Scholar]
- 136. Tarity TD, Garrigues GE, Ciccotti MG. et al. Pectoralis major ruptures in professional American football players. Phys Sportsmed. 2014;42(3):131–135. [DOI] [PubMed] [Google Scholar]
- 137. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the National Football League. Am J Sports Med. 2007;35(7):1162–1167. [DOI] [PubMed] [Google Scholar]
- 138. Tewes DP, Fischer DA, Quick DC, Zamberletti F, Powell J. Lumbar transverse process fractures in professional football players. Am J Sports Med. 1995;23(4):507–509. [DOI] [PubMed] [Google Scholar]
- 139. Trofa DP, Miller JC, Jang ES, Woode DR, Greisberg JK, Vosseller JT. Professional athletes’ return to play and performance after operative repair of an Achilles tendon rupture. Am J Sports Med. 2017;45(12):2864–2871. [DOI] [PubMed] [Google Scholar]
- 140. Tu LA, Knapik DM, Sheehan J, Salata MJ, Voos JE. Prevalence of Jones fracture repair and impact on short-term NFL participation. Foot Ankle Int. 2018;39(1):6–10. [DOI] [PubMed] [Google Scholar]
- 141. Weistroffer JK, Hsu WK. Return-to-play rates in National Football League linemen after treatment for lumbar disk herniation. Am J Sports Med. 2011;39(3):632–636. [DOI] [PubMed] [Google Scholar]
- 142. Werner BC, Belkin NS, Kennelly S. et al. Acute gastrocnemius-soleus complex injuries in National Football League athletes. Orthop J Sports Med. 2017;5(1):2325967116680344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Werner BC, Belkin NS, Kennelly S. et al. Injuries to the collateral ligaments of the metacarpophalangeal joint of the thumb, including simultaneous combined thumb ulnar and radial collateral ligament injuries, in National Football League athletes. Am J Sports Med. 2017;45(1):195–200. [DOI] [PubMed] [Google Scholar]
- 144. Werner BC, Mack C, Franke K, Barnes RP, Warren RF, Rodeo SA. Distal fibula fractures in National Football League athletes. Orthop J Sports Med. 2017;5(9):2325967117726515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. White M, Fleisig GS, Aune K, Andrews JR, Dugas JR, Cain EL. Return to play after shoulder stabilization in National Football League athletes. Orthop J Sports Med. 2014;2(suppl 2):2325967114S00024. [Google Scholar]
- 146. Yang J, Hodax JD, Machan JT. et al. National Football League skilled and unskilled positions vary in opportunity and yield in return to play after an anterior cruciate ligament injury. Orthop J Sports Med. 2017;5(9):2325967117729334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Zvijac JE, Toriscelli TA, Merrick S, Kiebzak GM. Isokinetic concentric quadriceps and hamstring strength variables from the NFL Scouting Combine are not predictive of hamstring injury in first-year professional football players. Am J Sports Med. 2013;41(7):1511–1518. [DOI] [PubMed] [Google Scholar]