Figure 4. Loss of the mucosal firewall allows systemic spread of ACPA response.
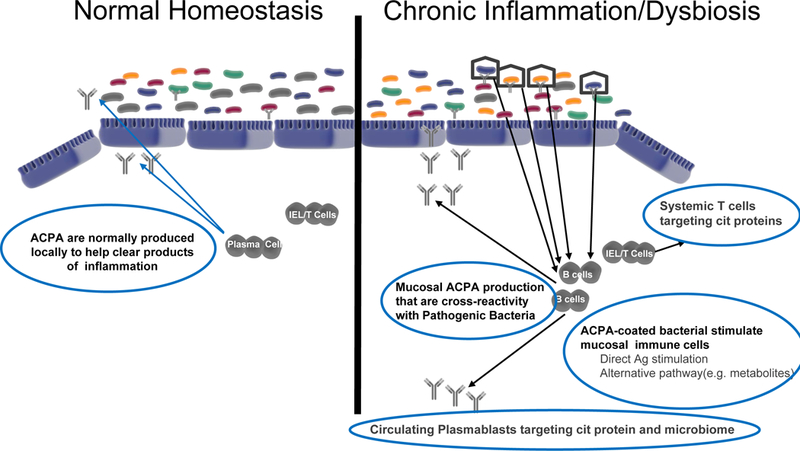
Hypothetical model for RA initiation as chronic mucosal inflammation and then transition to systemic autoimmune disease, focusing on the potential roles for normal and dysregulated local mucosal ACPA generation. Depicted at left is the reversible production of IgA ACPA in individuals as part of normal surveillance or who have transient mild inflammation. This process is common and part of normal homeostasis at the mucosal surface. At right is the postulated status of individuals in the pre-clinical RA state where persistent inflammation leads to increased ACPA production and systemic spread of an autoimmune process through multiple potential processes described herein. The drivers of this local and then systemic process could include cytokines, metabolomic changes, cross-reactive ACPA with bacterial antigens, or the presence of other antigen-specific cells that are expanded. Regardless of the mechanisms involved, these antibodies and cells begin to circulate as a reflection of the chronic inflammation and are detectable through serologic and other biomarker studies.
