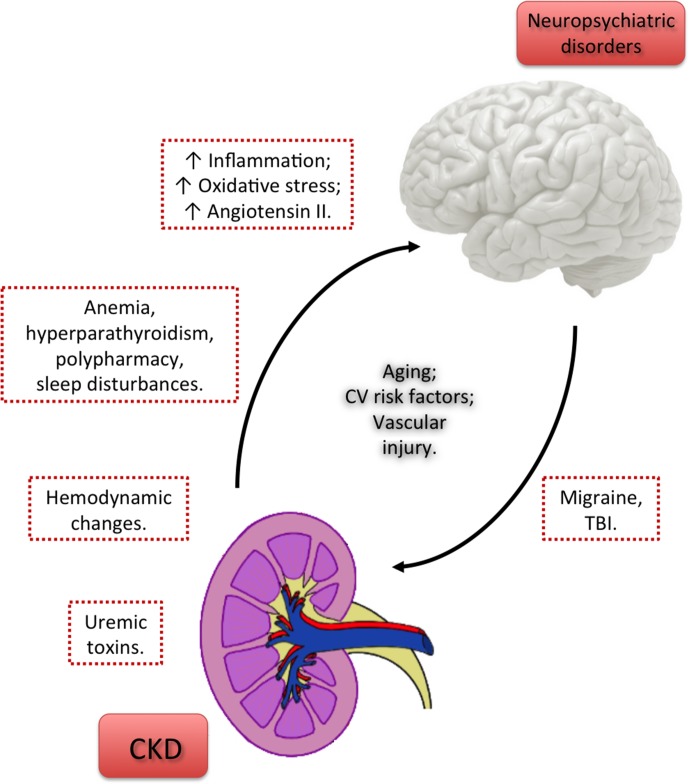
Figure 1.
Factors linking chronic kidney disease and neuropsychiatric disorders. Uremic toxins released as a result of CKD directly contribute to brain damage and the consequent cognitive decline and psychiatric disorders. However, the persistence of neuropsychiatric conditions despite adequate dialysis prescription points out that other factors may probably contribute to brain dysfunction. Hemodynamic changes, anemia, hyperparathyroidism, polypharmacy, and sleep disturbances due to CKD may represent a link between CKD and neuropsychiatric disorders. Other factors, shared by kidney and brain tissue injuries, as the increase in the levels of inflammatory molecules, reactive oxygen species and Angiotensin II may also contribute to kidney-to-brain interactions and, consequently, to neuropsychiatric comorbidities in CKD patients. The cross-talk between brain and kidney seems to be bidirectional, since central nervous system diseases, like migraine and TBI, are independent risk factors for CKD. Aging, CV risk factors, and vascular injury represent risk factors shared by CKD and neuropsychiatric disorders, notably cognitive impairment.CKD, chronic kidney disease; CV, cardiovascular; TBI, traumatic brain injury.