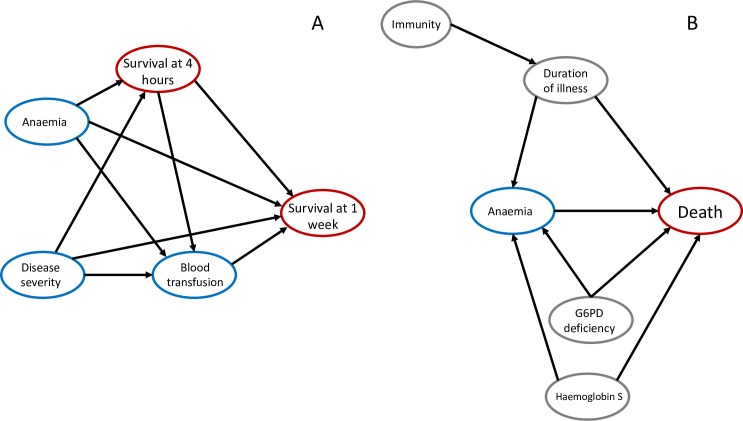
Fig 5. Mediation analysis and possible confounders for the protective effect of moderate anaemia on mortality in severe malaria.
(A) One explanation for the apparent protective effect of moderate anaemia on fatal outcomes in severe falciparum malaria might be that blood transfusions given to anaemic patients are independently beneficial. The probability of receiving a blood transfusion is affected by the presence and severity of anaemia at baseline and also depends on blood availability and local treatment guidelines and practices. This DAG shows the proposed causal relationships between admission covariates, blood transfusion status, and in-hospital mortality, stratified by the survival outcome at 4 hours from admission (square vertex). ‘Disease severity’ is a simplified representation of the complex web of interactions shown in Fig 3. In particular, we note that ‘Blood transfusion’ is a ‘collider’ between ‘Anaemia’ and ‘Survival at 1 week’, thereby introducing selection bias. (B) Possible unmeasured variables confounding the relationship between anaemia and fatal outcome. Grey vertices are unmeasured genetic variables such as G6PD deficiency and haemoglobinopathies, which both cause anaemia directly and are thought to protect against death from severe malaria, or unobserved variables related to underlying immunity to malaria, which has complex effects both protecting against death and potentially causing prolonged illness and more red cell loss [1]. DAG, directed acyclic graph; G6PD, glucose-6-phosphate dehydrogenase.