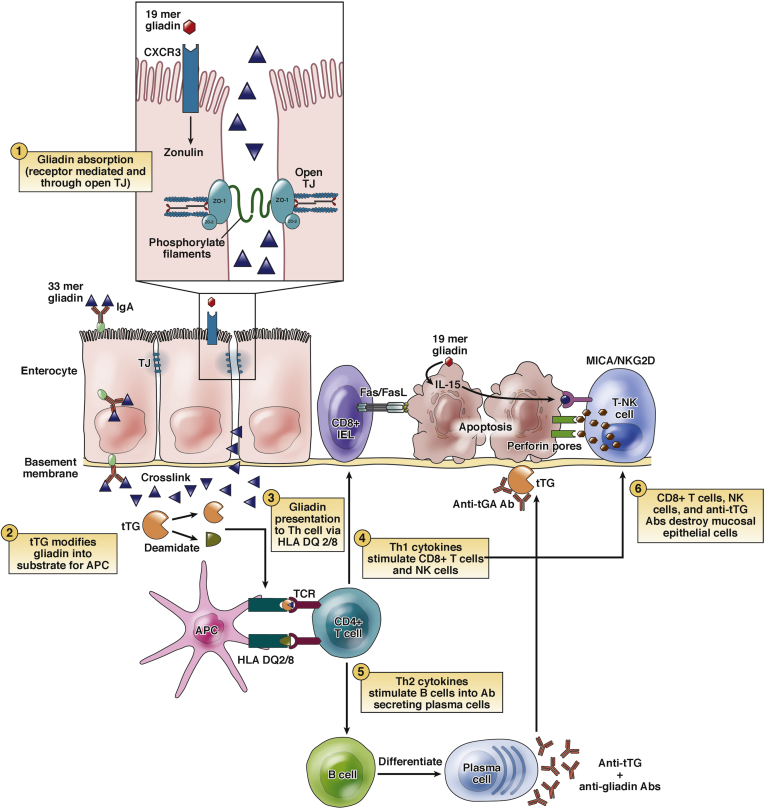
Figure 1.
Pathophysiology of celiac disease. Gliadin resists digestion in the duodenal lumen and may be directly toxic to the enterocytes of CeD patients. Undigested gliadin peptides cross into the intestinal submucosa via paracellular and transcellular passage. Tissue transglutaminase (tTG) deaminates gliadin peptides in the lamina propria. Deaminated gliadin is then recognized by HLA-DQ2 or HLA-DQ8 molecules on antigen-presenting cells (APCs), stimulating an immune reaction. This leads to the activation of Th1 and Th2 inflammatory pathways. Th1 cells stimulate CD8+ and natural killer (NK) cells, which causes apoptosis of the enterocytes via the Fas/FasL system. Th2 cells stimulate B cells to differentiate into plasma cells that produce antibodies (anti-tTG and antigliadin). The interaction between extracellular tTG and anti-tTG may cause further epithelial damage. Modified with permission from Di Sabatino and Corazza.58 NK, natural killer; TJ, tight junction.