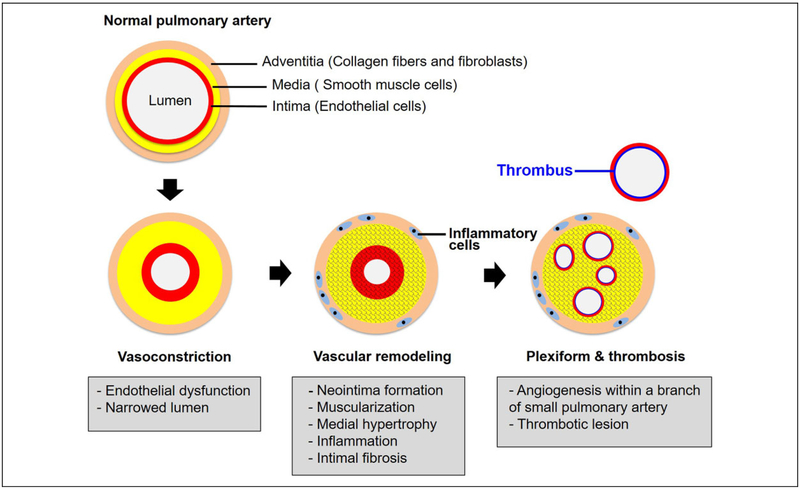
Figure 1.
Pathogenesis of PAH. Multiple vascular cell types, endothelial cells, smooth muscle cells, and fibroblasts are involved in pulmonary arterial pathobiology. Healthy endothelium modulates the balance between vasodilation and vasoconstriction and inhibits smooth muscle cell proliferation in order to maintain a low-resistance pulmonary vasculature. Pulmonary vasoconstriction has long been regarded as an early event, and excessive pulmonary vasoconstriction has been related to endothelium dysfunction characterized by reduced production of vasodilators (nitric oxide and prostacyclin), along with overexpression of vasoconstrictors (endothelin-1). Abnormal proliferation of smooth muscle cells is the earliest pathobiological features of vascular remodeling, leading to muscularization of peripheral pulmonary arteries and medial hypertrophy in pulmonary muscular arteries. Recruitment of inflammatory cells and progressive migration of smooth muscle cells further results in intimal fibrosis. In the late stage of disease progression, formation of plexiform lesions and in situ thrombus occlude the vessel lumen leads to progressive reduction of the blood flow, thus establishing PAH. PAH indicates pulmonary arterial hypertension.