Abstract
Background
The purpose of this study was to use second-look arthroscopic findings and clinical assessment to determine outcome in two cases of knee osteoarthritis treated by intra-articular knee injection of adipose-derived regenerative cells (ADRCs).
Case presentation
This study involved two patients who received ADRC therapy for knee osteoarthritis and completed the six-month post-treatment follow-up period. For each treatment, 130 mL of subcutaneous adipose tissue was harvested using tumescent liposuction technique and manual aspiration of tissue from the thigh using a suction cannula under local anesthesia in the operating room. The adipose tissue harvested was processed using the Celution® Centrifuge in a dedicated cell processing room. The ADRCs were injected into the articular cavity of both knees for one patient and into a single affected knee in the second patient (three joints). Pain and knee function were assessed using a Visual Analogue Scale (VAS) and the Knee Outcome in Osteoarthritis Score (KOOS) respectively. The cartilage defect was assessed by direct visualization (arthroscopy). No serious adverse events were reported throughout follow-up. Pain and knee function were significantly improved from baseline in all treated knees at one, three and six months after ADRCs. At six-months after ADRCs treatment, the second-look arthroscopy showed that almost all the cartilage defect areas were covered by regenerated cartilage, some cartilage fibrillation area was reduced, and meniscus tear areas were repaired.
Conclusions
Cartilage and meniscus repair were observed six-months after ADRCs therapy under second-look arthroscopy. It was shown that a single administration of ADRCs might be effective as a treatment for knee osteoarthritis.
Keywords: Adipose-derived regenerative cells, Second-look arthroscopy, Knee osteoarthritis, Cartilage, Meniscus
1. Introduction
Osteoarthritis (OA) of the knee is a common and painful degenerative condition with few effective treatments [1], [2]. For mild to moderate OA, medical care usually includes weight control, NSAIDs, intra-articular hyaluronic acid, and rehabilitation. However, each of these is limited by the chronic progressive nature of the disease and by the limited ability of cartilage to regenerate [3]. As a result, despite best available care for many patients, pain and dysfunction progress to the point of requiring total knee arthroplasty in which the dysfunctional joint is replaced with an artificial implant [4].
Regenerative medicine is a novel approach that applies the natural capacity of the body's stem and regenerative cells to promote healing of organs or tissues that, like cartilage, are otherwise unable to repair themselves. In recent years it has been demonstrated that adipose (fat) tissue is a rich source of cells capable of promoting regeneration [5], [6], [7], [8], [9]. Transplantation of adipose-derived regenerative cells (ADRCs) involves applying clinical-grade processes and reagents to isolate and concentrate stromal vascular fraction (SVF) cells existing in subcutaneous adipose tissue, and delivering them to the target area. These cells include adipose-derived stem cells that have been shown to be capable of differentiating into cartilage [10], [11], [12]. They also include cell types capable of modulating the low level chronic inflammation and synovitis present in OA thereby potentially increasing anabolic, cartilage-formation while simultaneously reducing catabolic, cartilage-damaging processes [5]. The abundance of these cells in adipose tissue and the limited morbidity of adipose tissue collection allows the patient to be treated with their own cells and without the need for cell culture thereby eliminating risks associated with donor tissue or with contamination or other culture-related problem.
There are several reports on the treatment of knee osteoarthritis with ADRCs or SVF cells [13], [14], [15], [16], [17], [18], [19], however we are aware of only a few reports applying second-look arthroscopy and that was following injection of both SVF cells and platelet-rich plasma rather than SVF cells or ADRCs alone [20], [21], [22], [23]. The purpose of this article is to report two cases where second-look arthroscopy was performed six months after single administration of ADRCs for treatment of knee osteoarthritis in which evidence of cartilage repair, meniscus repair and functional recovery was observed.
2. Case presentation
Following review by the Certified Special Committee for Regenerative Medicine (Anzen Mirai Committee of Regenerative Medicine), this treatment was accepted by Kinki Regional Bureau of Health and Welfare in accordance with the Act on the Safety of Regenerative Medicine (Protocol Acceptance Number: PB5170004). Patients signed a written informed consent before receiving this treatment.
2.1. 1st case
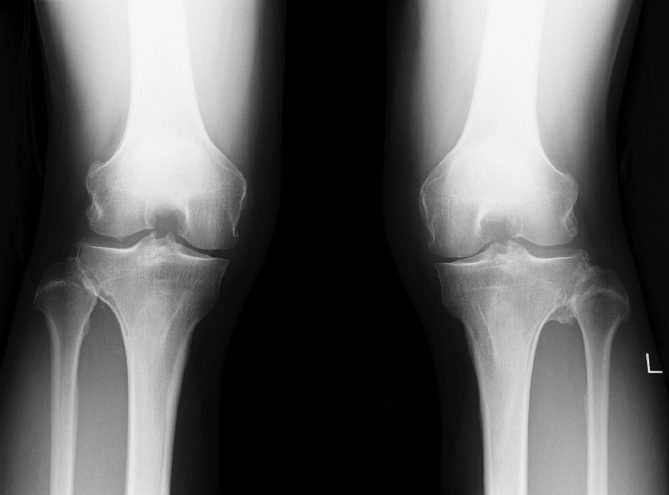
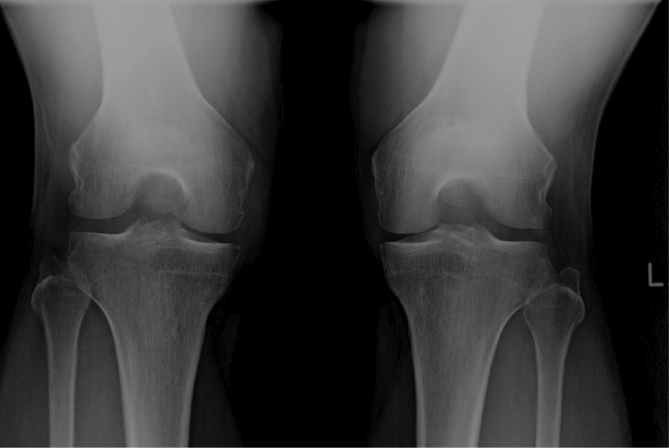
A 54-year-old male occupational therapist visited our outpatient department complaining of pain in both knees for more than seven months. Despite having undergone conservative treatment including analgesics, hyaluronic acid injections and rehabilitation by a general practitioner, his symptoms did not improve and gradually limited his sport activities including marathon running and soccer. Upon physical examination, although no instability was observed, there was mild swelling with a positive McMurray test, and tenderness on the medial joint space in both knees. X-ray showed the joint space narrowing in the medial compartment of the right knee (Kellgren–Lawrence (KL) grade Ⅱ [24]) and that of the left knee (KL grade Ⅲ) (Fig. 1). MRI showed the medial cartilage loss and the degeneration of the medial meniscus especially in the posterior horn in the both knees.
Fig. 1.
1st case X-ray was taken in a weighted postero-anetrior view in knee 45° flexion (Rosenburg's view). A slight and moderate medial joint space narrowing was seen in right and left knee, respectively (KL grade Ⅱ,Ⅲ).
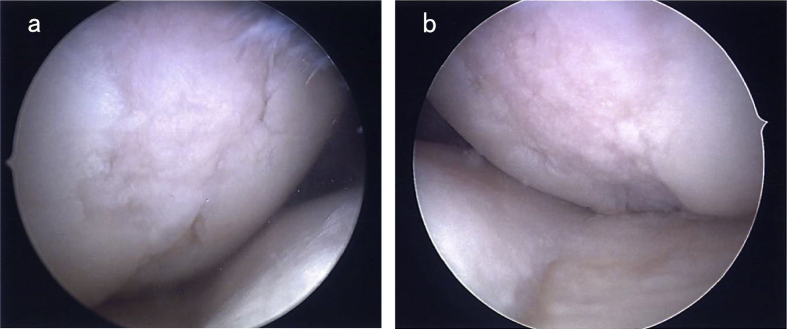
Before treatment with ADRCs, the patient underwent diagnostic arthroscopy on both knees. The right medial femoral condyle had a 2.5 × 1.5 cm cartilage defect area with a depth of grade Ⅲ according to the International Cartilage Repair Association (ICRS) cartilage injury classification. The left medial femoral condyle had a 3 × 1.5 cm cartilage tear of ICRS grade Ⅲ (Fig. 2). Degeneration without apparent tear was found on the right side but degenerative tear was found on the left medial meniscus posterior horn.
Fig. 2.
Preoperative arthroscopic findings in the right and left medial femoral condyles in 1st case. 2.5 × 1.5 cm cartilage defect was seen in the right knee (2a). 3 × 1.5 cm cartilage defect was seen in the left knee (2b).
ADRCs were prepared by enzymatic digestion of 130 ml of adipose tissue collected from both thighs using manual aspiration into 60 mL syringes following infiltration of tumescent solution comprising 500 mL of lactated ringers solution supplemented with 20 mL of 1% lidocaine and 1 mg of epinephrine under general anesthesia. Tissue was processed using the Celution® Centrifuge (Cytori Therapeutics K.K., Tokyo, Japan) according to the manufacturer's instructions. Briefly, the system washes the aspirated tissue with sterile lactated Ringer's solution to remove blood and free lipid and then digests the extracellular matrix releasing buoyant adipocytes and ADRCs. The ADRCs are then concentrated and washed within the closed fluid path of the Celution® Disposable Set to prepare the final ADRC product. Viability and cell number were determined in triplicate with a Nucleocounter NC-100 (ChemoMetec A/S, Allerod, Denmark), according to manufacturer's instructions. For this patient a total of 12,000,000 viable ADRCs/5 mL (viability = 94.1%), were injected into the intra-articular space of the both knees (2.5 mL each). Injection was performed following aspiration of 0.5 mL synovial fluid.
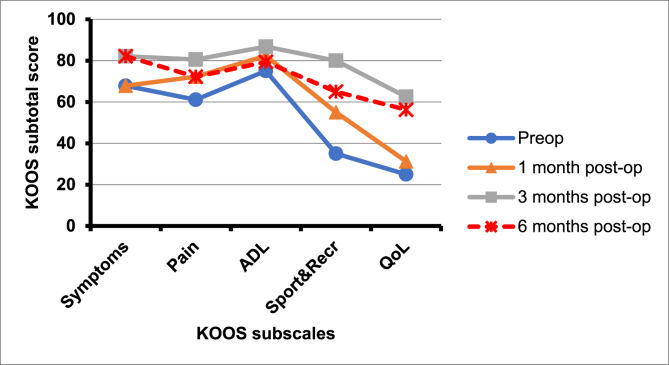
One month after the operation, the patient reported that knee pain was reduced. The patient's KOOS [25] was also substantially improved (Table 1, Fig. 3) without any rehabilitation. Further improvement was evident at 3 months though there was a small decrease between 3 and 6 months such that benefit at 6 months was essentially the same as that at 1 month. By the time of the six months visit the patient had returned to sports. At that time the patient underwent a second look arthroscopy. The cartilage defect areas were found to be covered by regenerated cartilage on the medial and lateral condyle in both knees. Although width of cartilage was not same as surrounding cartilage, almost all of the cartilage defect area was covered by regenerated tissue (Fig. 4).
Table 1.
Outcome of VAS and KOOS in 1st case. VAS was scored by 10-point scale (0–10) (0 = no pain; 10 = worst possible pain).
| Preoperative | 1 month | 3 months | 6 months | |
|---|---|---|---|---|
| VAS | 4 | 1 | 1 | 1 |
| KOOS | 61.3 | 69.6 | 81.5 | 74.4 |
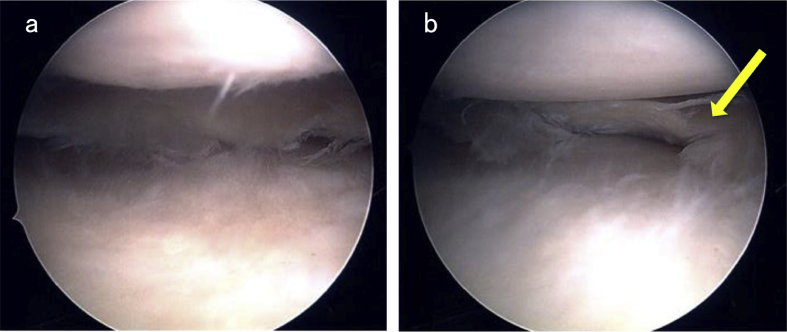
Fig. 3.
KOOS scores at the preoperative, 1-, 3-, 6-month assessments after ADRCs therapy in 1st case. ADL: activities of daily living, Sports&Recr: sports and recreation, QoL: quality of life.
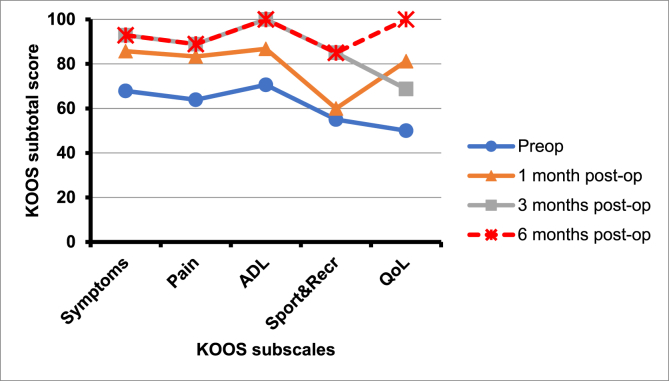
Fig. 4.
Second-look arthroscopic findings in the right and left medial femoral condyles at 6 months after operation in 1st case. The cartilage defect areas were covered by regenerated cartilage respectively (4a:right, 4b:left).
2.2. 2nd case
A 63-year-old male visited our outpatient department complaining of pain in right knee for more than one year. Despite having undergone conservative treatment including analgesics, hyaluronic acid injections and rehabilitation by a general practitioner, his symptoms had not improved and gradually limited his sport activities (specifically, table tennis). Upon physical examination, although no instability was observed, mild swelling and tenderness were present on the medial joint space in the right knee. Joint space narrowing was not seen but osteophyte development was evident by X-ray analysis (KL grade Ⅰ) (Fig. 5). MRI showed degeneration of the medial meniscus especially in the posterior horn, but medial cartilage loss was unclear.
Fig. 5.
2nd case X-ray was taken in Rosenburg's view. Joint space narrowing was not seen but osteophyte development was seen in right knee (KL grade Ⅰ).
Before treatment with ADRCs, the patient underwent diagnostic arthroscopy on right knee. Partial thickness cartilage tear of ICRS grade Ⅱ and fibrillation were found to be 2 × 1.5 cm in femoral medial condyle and 1.5 × 1.5 cm in tibial medial condyle. Degenerative tear was found on the medial meniscus posterior horn and partial meniscectomy was carried out (Fig. 6).
Fig. 6.
Preoperative arthroscopic findings in the medial condyle of the right knee in 2nd case. 2 × 1.5 cm and 1.5 × 1.5 cm cartilage partial thickness tears were seen in femoral and tibial condyles respectively (6a). Degenerative tear was seen on the posterior horn of the medial meniscus (6b).
As in case 1, ADRCs were prepared by enzymatic digestion of 130 ml of adipose tissue collected from both femurs. For this patient, a total of 5,500,000 total viable ADRCs/5 mL (viability = 89.4%) were injected into the intra-articular space of the right knee in 5 mL after the aspiration of 0.5 mL synovial fluid.
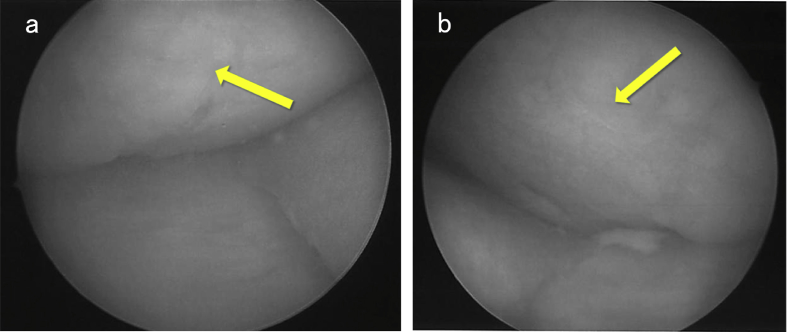
Pain and function were both improved at one month after treatment (Table 2, Fig. 7) without any rehabilitation. As with the first patient, these effects were sustained to 6 months at which time the patient had returned to normal sports activity. Second look arthroscopy performed at 6 months showed that the cartilage injury area was completely covered by regenerated cartilage on the medial femoral condyle. On the medial tibial condyle, the cartilage fibrillation area remained but was reduced. Additionally, the resected part of medial meniscus posterior hone was repaired (Fig. 8).
Table 2.
Outcome of VAS and KOOS in 2nd case.
| Preoperative | 1 month | 3 months | 6 months | |
|---|---|---|---|---|
| VAS | 5 | 1 | 2 | 1 |
| KOOS | 64.9 | 82.1 | 91.7 | 94.6 |
Fig. 7.
KOOS scores at the preoperative, 1-, 3-, 6-month assessments after ADRCs therapy in 2nd case. ADL: activities of daily living, Sports&Recr: sports and recreation, QoL: quality of life.
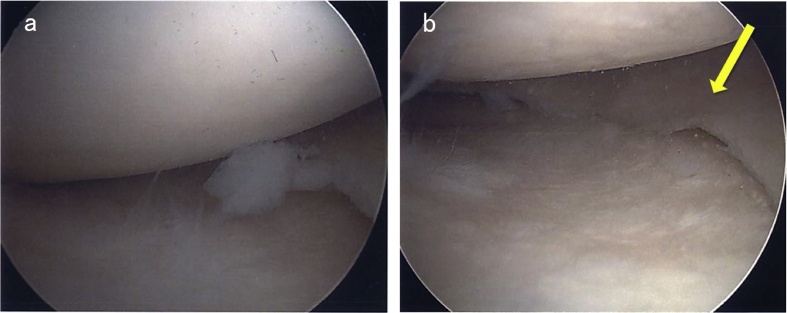
Fig. 8.
Second-look arthroscopic findings in the medial condyle of the right knee at 6 months after operation in 2nd case. The cartilage damage area in medial femoral condyle was covered by regenerated cartilage (8a). On the medial tibial condyle, the cartilage fibrillation area was remained but reduced (8a,b). Degenerative tear on the posterior horn was repaired with only administering of ADRCs (8b).
3. Discussion
In these cases, regeneration of cartilage was confirmed by arthroscopy with a single administration of ADRCs alone. There have been several past reports of ADRCs therapy for treatment of knee osteoarthritis; however these are mainly focused on clinical symptoms [13], [14], [15], [16], [17], [18], [19] and a few have reported visualization of the articular surface by second-look arthroscopy [20], [21], [22], [23]. However, Koh et al. [20] reported a combined use of platelet-rich plasma and SVF cells was introduced. In addition, there is a possibility of qualitative improvements even though no morphological improvements are seen, hence it will be necessary to consider T2 mapping etc for evaluation.
We were able to confirm cartilage repair macroscopically during arthroscopy this time. In the past, Kim et al. [21] reported cartilage was seen through arthroscopy when MSCs were implanted in the knee joint with fibrin glue. We were able to see similar results, but we believe regeneration seen with a single dose of ADRCs is significant.
In the present cases, improvement in both pain and function were seen within a month after treatment with ADRCs. Three months later, the patients had returned to previous sports activity without any limitation. These benefits appeared to be sustained to 6 months although there was a small worsening between 3 and 6 months for the first patient. This may have been due to normal variations evident in patient-reported outcome instruments such as the KOOS or to premature return to sports. For that reason the patient was advised to moderate his sports activity.
The primary limitation of this study is that it is based on two cases with a short follow-up period of six months. However, due to the progressive degenerative nature of the disease state, natural recovery is not expected. It seems significant that we are able to see such improvements in a half year period. However, longer-term follow-up will be useful to determine the utility of this standalone procedure based on a single dose of ADRCs. While it is possible that further improvement may be expected with the addition of a second treatment or, perhaps, co-administration of SVF with PRP [20], the benefits of a standalone treatment has substantial advantages from a cost and labor perspective. Our hospital plans to continue performing second-look arthroscopy in future patients according to the approach described herein. More cases will be evaluated and reported in the future.
4. Conclusion
We report two cases of patients with debilitating OA of the knee exhibiting evidence of cartilage and meniscal repair six months after treatment with ADRCs. Concomitant improvements were seen in clinical symptoms and activity. Although further long-term follow-up and a larger sample size will be needed to confirm this finding these data indicate that administration of ADRCs alone might be effective as a treatment for knee osteoarthritis.
Footnotes
Peer review under responsibility of the Japanese Society for Regenerative Medicine.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.reth.2019.07.010.
Contributor Information
Yuma Onoi, Email: yuma.onoi.51@gmail.com.
Takafumi Hiranaka, Email: takafumi.hiranaka@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Buckwalter J.A., Martin J.A. Osteoarthritis. Adv Drug Deliv Rev. 2006;58(2):150–167. doi: 10.1016/j.addr.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Matsui Y., Harada A. Aging of joint. Clin Calcium. 2013;23(1):15–22. [PubMed] [Google Scholar]
- 3.Coleman C.M., Curtin C., Barry F.P., O'Flatharta C., Murphy J.M. Mesenchymal stem cells and osteoarthritis: remedy or accomplice? Hum Gene Ther. 2010;21(10):1239–1250. doi: 10.1089/hum.2010.138. [DOI] [PubMed] [Google Scholar]
- 4.Buckwalter J.A., Saltzman C., Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res. 2004;427:S6–S15. doi: 10.1097/01.blo.0000143938.30681.9d. [DOI] [PubMed] [Google Scholar]
- 5.Kesten S., Fraser J.K. Autologous adipose derived regenerative cells:A platform for therapeutic applications. Surg Technol Int. 2016;29:38–44. [PubMed] [Google Scholar]
- 6.Folgiero V., Migliano E., Tedesco M., Iacovelli S., Bon G., Torre M.L. Purification and characterization of adipose-derived stem cells from patients with lipoaspirate transplant. Cell Transplant. 2010;19(10):1225–1235. doi: 10.3727/09638910X519265. [DOI] [PubMed] [Google Scholar]
- 7.Lindroos B., Suuronen R., Miettinen S. The potential of adipose stem cells in regenerative medicine. Stem Cell Rev. 2011;7(2):269–291. doi: 10.1007/s12015-010-9193-7. [DOI] [PubMed] [Google Scholar]
- 8.Fujimura J., Sugihara H., Fukunaga Y., Suzuki H., Ogawa R. Adipose tissue is a better source of immature non-hematopoietic cells than bone marrow. Int J Stem Cells. 2009;2(2):135–140. doi: 10.15283/ijsc.2009.2.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madonna R., Geng Y.J., De Caterina R. Adipose tissue-derived stem cells: characterization and potential for cardiovascular repair. Arterioscler Thromb Vasc Biol. 2009;29(11):1723–1729. doi: 10.1161/ATVBAHA.109.187179. [DOI] [PubMed] [Google Scholar]
- 10.Zuk P.A., Zhu M., Ashjian P., De Ugarte D.A., Huang J.I., Mizuno H. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13(12):4279–4295. doi: 10.1091/mbc.E02-02-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang J.I.1, Zuk P.A., Jones N.F., Zhu M., Lorenz H.P., Hedrick M.H. Chondrogenic potential of multipotential cells from human adipose tissue. Plast Reconstr Surg. 2004;113(2):585–594. doi: 10.1097/01.PRS.0000101063.27008.E1. [DOI] [PubMed] [Google Scholar]
- 12.O'Sullivan J., D'Arcy S., Barry F.P., Murphy J.M., Coleman C.M. Mesenchymal chondroprogenitor cell origin and therapeutic potential. Stem Cell Res Ther. 2011;2(1):8–14. doi: 10.1186/scrt49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yokota N., Yamakawa M., Shirata T., Kimura T., Kaneshima H. Clinical results following intra-articular injection of adipose-derived stromal vascular fraction cells in patients with osteoarthritis of the knee. Regen Ther. 2017;19(6):108–112. doi: 10.1016/j.reth.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hurley E.T., Yasui Y., Gianakos A.L., Seow D., Shimozono Y., Kerkhoffs G.M.M.J. Limited evidence for adipose-derived stem cell therapy on the treatment of osteoarthritis. Knee Surg Sport Traumatol Arthrosc. 2018;26(11):3499–3507. doi: 10.1007/s00167-018-4955-x. [DOI] [PubMed] [Google Scholar]
- 15.Fodor P.B., Paulseth S.G. Adipose derived stromal cell (ADSC) injections for pain management of osteoarthritis in the human knee joint. Aesthet Surg J. 2016;36(2):229–236. doi: 10.1093/asj/sjv135. [DOI] [PubMed] [Google Scholar]
- 16.Black L.L., Gaynor J., Gahring D., Adams C., Aron D., Harman S. Effect of adipose-derived mesenchymal stem and regenerative cells on lameness in dogs with chronic osteoarthritis of the coxofemoral joints: a randomized, double-blinded, multicenter, controlled trial. Vet Ther. 2007;8(4):272–284. [PubMed] [Google Scholar]
- 17.Wakitani S., Imoto K., Yamamoto T., Saito M., Murata N., Yoneda M. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. Osteoarthr Cartil. 2002;10(3):199–206. doi: 10.1053/joca.2001.0504. [DOI] [PubMed] [Google Scholar]
- 18.Veronesi F., Maglio M., Tschon M., Aldini N.N., Fini M. Adipose-derived mesenchymal stem cells for cartilage tissue engineering: state-of-the-art in in vivo studies. J Biomed Mater Res A. 2014;102(7):2448–2466. doi: 10.1002/jbm.a.34896. [DOI] [PubMed] [Google Scholar]
- 19.Orozco L., Munar A., Soler R., Alberca M., Soler F., Huguet M. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: two-year follow-up results. Transplantation. 2014;971(11):e66–e68. doi: 10.1097/TP.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 20.Koh Y.G., Choi Y.J., Kwon S.K., Kim Y.S., Yeo J.E. Clinical results and second-look arthroscopic findings after treatment with adipose-derived stem cells for knee osteoarthritis. Knee Surg Sport Traumatol Arthrosc. 2015;23(5):1308–1316. doi: 10.1007/s00167-013-2807-2. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y.S., Kwon O.R., Choi Y.J., Suh D.S., Heo D.B., Koh Y.G. Comparative matched-pair analysis of the injection versus implantation of mesenchymal stem cells for knee osteoarthritis. Am J Sports Med. 2015;43(11):2738–2746. doi: 10.1177/0363546515599632. [DOI] [PubMed] [Google Scholar]
- 22.Jo C.H., Lee Y.G., Shin W.H., Kim H., Chai J.W., Jeong E.C. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014;32(5):1254–1266. doi: 10.1002/stem.1634. [DOI] [PubMed] [Google Scholar]
- 23.Koh Y.G., Choi Y.J., Kwon O.R., Kim Y.S. Second-look arthroscopic evaluation of cartilage lesions after mesenchymal stem cell implantation in osteoarthritic knees. Am J Sports Med. 2014;42(7):1628–1637. doi: 10.1177/0363546514529641. [DOI] [PubMed] [Google Scholar]
- 24.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roos E.M., Roos H.P., Lohmander L.S., Ekdahl C., Beynnon B.D. Knee injury and osteoarthritis outcome score (KOOS)-development of a self-administered outcome measure. J Orthop Sport Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.