Abstract
Background
Cesarean section rates have been increasing dramatically during the past three decades and surgical site infections are becoming a leading cause of morbidity and mortality among women undergoing cesarean deliveries. However there is lack of sound evidence on both the magnitude of the problem and the associated factors in developing countries including Ethiopia. The purpose of this study was to assess proportion of surgical site infection and associated factors among women undergoing cesarean delivery in Debretabor General Hospital.
Methods
An institution based cross sectional study was conducted from May to December / 2017. All women delivered by cesarean section in Debretabor General Hospital during data collection period were our study population. Data were collected using Pre-tested, semi-structured questionnaire/ data extraction tool and post discharge phone follow up and analyzed using SPSS version 20. Logistic regression model was used to determine the association of independent variables with the outcome variable and odds ratios with 95% confidence interval were used to estimate the strength of the association.
Results
Proportion of surgical site infection among cesarean deliveries was about 8% (95%Cl: 5.4, 11.6). Pregnancy induced hypertension (AOR = 4.75, 95%CI: 1.62, 13.92), chorioaminitis (AOR = 4.37, 95%CI: 1.53, 12.50), midline skin incision (AOR = 5.19, 95% CI: 1.87, 14.37 and post-operative hemoglobin less than 11 g/deciliter (AOR = 5.28, 95%CI: 1.97, 14.18) were significantly associated with surgical site infection.
Conclusions
Pregnancy induced hypertension, chorioaminitis, midline skin incision and post-operative hemoglobin of less than 11 g/deciliter were independent factors associated with surgical site infection. Cesarean deliveries with concomitant pregnancy induced hypertension, chorioaminitis and post-operative anemia needs special care and follow up until surgical site infection is ruled out. It is also advisable to reduce generous midline skin incision and better replaced with pfannensteil incision.
Keywords: Surgical site infection, Cesarean delivery, Debretabor General Hospital
Background
Surgical site infection (SSI) is an infection occurring within 30 days after the operation and involves the skin and subcutaneous tissue and/or the deep soft tissue of the incision [1–3].
SSI is a leading cause of morbidity and mortality among women undergoing cesarean section (CS) with reported rates of 3–15% [4–6]. High rates of SSI following CS were reported in several lower and middle income countries: 16.2% in a study from Nigeria, 19% from Kenya, 10.9% from Tanzania and 9.7% from Viet Nam among others. [7, 8].
According to a study done in China, 3.34% of cesarean deliveries (CDs) were complicated by SSI [9]. In contrast,SSI complicated 12.6% [10] and 24.3% [11] of CDs at Dhulikhel Hospital (Nepal) and Karachi (Pakistan) respectively. A prevalence rate of 6.2% [12] SSI following CDs was reported in a study done in Ankara (Turkey) and lower rate of SSI (3.7%) was reported in study done in Israel [13]. A study at Teaching Hospital in Rwanda revealed that 4.9% CDs were complicated by SSI [14].
However, SSI following CDs was reported on almost half (48.2%) of CDs at Tanzanian Tertiary Hospital [15]. In Ethiopian context, the prevalence of SSI at Hawassa Teaching and Referral Hospital was 11% [16]. Meanwhile 9.4% of CDs were complicated by SSI at Assela Teaching and Referral Hospital [17]. Similarly study done at Lemlem karl General Hospital (Tigrai region) revealed 6.8% of CDs had developed SSI [18].
Pre-operative conditions such as prolonged labor, prolonged rupture of membrane (PROM), more than 5 digital vaginal examination, chorio-amnionitis, American society of Anesthesiologist (ASA) health status classification ≥3, fewer years of education, higher prior births, prior diagnosis of hypertension and Diabetes Mellitus (DM) were identified as significant factors for SSI following CDs [10, 15, 16, 19–22]. Similarly intra operative conditions like prolonged duration of surgery, wound contamination class III, vertical skin incision and interrupted skin suturing were associated factors for developing SSI [8, 9, 15, 16, 19, 23, 24]. CD for emergency conditions like non-reassuring fetal heart rate pattern (NRFHRP) was also significantly associated factor for developing SSI [19, 24, 25]. In addition, Postoperative anemia was also found to be a post-operative factor associated with SSI [16, 26].
In Ethiopian context post-partum infection is the fourth leading cause of maternal mortality and morbidity from which SSI shares the largest proportion [27]. Even if admissions following CDs due to SSI have been routine activities of health care institutions in our set up, there is lack of strong evidence on both the magnitude of the problem and the associated factors making prevention mechanisms less effective. Few efforts have been done in terms of both quantifying the problem and identifying the determinant factors.
A study conducted at Jimma University specialized hospital had reported the magnitude of then SSI on obstetric cases and had identified associated factors [28]. But the reported magnitude was not specific to SSI following CD and the identified factors were not tested for confounding effects. More over 8 years has been lapsed after this study and the tracing mechanism of study participants after discharge was not as such reliable. More recently three studies have been done in Hawassa, Assela and Maichew and reported their respective magnitude of SSI following CDs and the determinant factors. But all of them were conducted retrospectively using only secondary data. Therefore, this study aimed to quantify the proportions of post-caesarean wound infection and to identify the associated factors among cesarean deliveries (CDs) at Debretabor General Hospital (DGH). This will have a fundamental role in forming a basis for future studies and measures to prevent SSI following CDs at this hospital level in particular and nationwide in general.
Methods
Study design and period
Hospital based cross-sectional study was conducted from May 20 to December 15 /2017.
Study setting
This study was conducted in DGH located in Debretabor town of Amhara Regional State. Debretabor town is about 98 km away to the East of Bahir-Dar (the capital of Amhara regional state) and about 667 km away to North of Addis Ababa (the capital of Ethiopia). DGH is the only general hospital in the south Gondar Zone having over 102 beds. Obstetrics and gynecology service is organized to a ward with a capacity of 22 beds and an operation room for emergency cesarean deliveries, maternal and child health unit, gynecology referral clinic and safe abortion clinic. The service is provided by two obstetrician and gynecologists, five integrated emergency surgical officers and over 22 professional and diploma midwives. About 3600 deliveries are conducted every year of which about 700 of them are by CS.
Characteristics of participants
Women who delivered by CS from May 20 to December 15/2017 at DGH were included in this study. Women who didn’t have tracing mechanisms (if either the woman and/or her attendant/family didn’t have phone number) after discharge were excluded.
Variables of the study
Outcome variable
SSI following CD (present/absent).
Independent variables/predictor variables include
Age, residence, educational status, marital status, body mass index (BMI), health status classification, hypertension, DM, heart disease, anemia, gravidity, parity, onset of labor, status of membrane,duration of ROM, duration of labor, number of vaginal examination, gestational diabetes mellitus (GDM), gestational age, antenatal care (ANC) follow up, chorioaminionitis, steroid therapy, pregnancy induced hypertension (PIH), type of CS, duration of the operation, skin incision type, skin suturing type, wound classification, estimated blood loss (EBL), intraoperative blood transfusion, and post-operative hemoglobin level.
Enrolment of study participants
Census approach was used to include women delivered by CS from May 20 to December 15/2017. There were a total of 359 CDs of which 12 of them were excluded due to absence of tracing mechanism after discharge. The remaining 347 study participants were included in the study but 334 of them were traced for 30 days (Fig. 1).
Fig. 1.
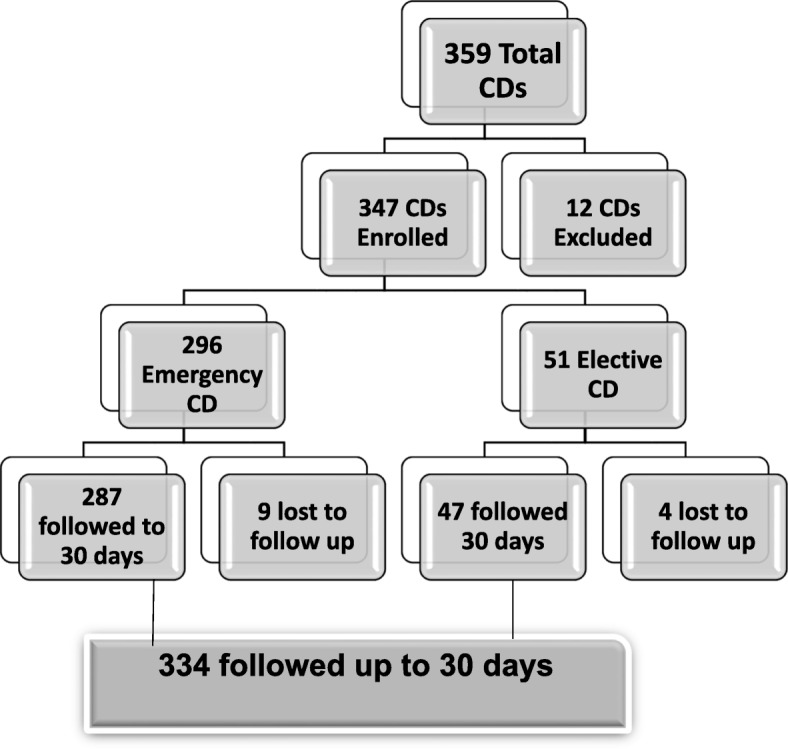
Schematic presentation of enrolment of study participants for surgical site infection and associated factors among cesarean deliveries at Debretabor general hospital, 2017
For the sake of clarity, some of the operational definitions used in this research include: SSI was defined as per the criteria of the Centers for Disease Control and Prevention (CDC) guideline [1]. ASA physical status was defined as assessment of the woman’s preoperative physical condition using the ASA Classification of Physical status [29].
Wound class was defined as assessment of the degree of contamination of a surgical wound at the time of the operation by a person involved in the surgical procedure [29]. Steroid therapy was defined as preoperative maternal treatment with either betamethasone or dexamethasone for fetal lung maturity. Duration of membrane rupture was determined by the time lapsed in hour from either mother’s complain of leakage of liquor or artificial rupture of membrane to skin incision. Duration of labor was determined by the time lapsed in hour from mother’s complain of symptoms of true labor to skin incision. Duration of operation was determined by the time lapsed in hour from skin incision to skin closure. EBL was determined by the number of packs and gauze used during time of operation multiplied by estimated absorbable amount of blood by a single pack (1 soaked pack = 100 ml) and gauze (1 soaked gauze = 20 ml of blood) respectively. Post-operative hemoglobin represented hemoglobin level in gram/deciliter after 8 hours of post-operative period. Obesity represented maternal preoperative BMI > 25 kg/m2.
Data collection tools and procedures
Training procedures for data collectors
Data collectors and supervisors had 1 day training before the actual data collection.
Data collection tools and procedures for risk factors and outcome
Ethical approval to conduct this study was obtained from department of midwifery Ethical Review Committee under the delegation of Institutional Review Board (IRB) of University of Gondar. Six diploma midwives (two per shift) from obstetrics and gynecology ward were used to collect both the risk factor and outcome data. Two other Bachelor of Science (BSc) midwives from Debretabor University were assigned to supervise the data collection process. Before data collection process the data collectors informed each study participant about the purpose and anticipated benefits of the research project. The study participants had also been informed on their full right to refuse, withdraw or completely reject part or all of their part in the study. They had also been informed that their address and phone number would be used for the sole purpose of follow up and all data obtained from them would be kept confidential. Written consent was obtained from study participants prior to data collection. Study participants who were ≥ 18 years of age gave their written consent. Study participants who were < 18 years of age gave their written consent via their family members. Family members used to provide consent on the behalf of participants under the age of 18 were participants’ husbands and either of the participants’ parents. Priority was given for husbands and parents were considered in cases of either husbands’ absence or husbands’ minority age (under 18 years of age). We can confirm that the ethics committee had approved the use of attendants (husband or either of the parents) on the behalf of participants under the age of 18.
Data were collected by face to face interview of study participants, direct observation of the CS procedure and by reviewing of study participants’ charts. A semi structured and pre-tested questionnaire/data extraction tool prepared in English, translated to Amharic (local language) and then translated back to English was used to collect data. Relevant preoperative and intra operative events were observed, asked and recorded. Postoperatively, surgical wounds were examined immediately before discharge and their status recorded. Discharging study participants were counseled about symptoms of SSI and the need to return to the hospital immediately for any infected wound complaints. Their relevant addresses (phone number, place of residence and the name of the nearest health care institution) were well documented. Regular telephone calls were made at 15th and 30th post operation day [14] with an option to communicate at any time if suspicion of wound infection arose. SSI was identified before discharge and/or by readmission and evaluation of those participants with concerns of wound infection during phone calls or came directly with complain of symptoms of wound infection after discharge based on the criteria of CDC [29].
CDC criteria for defining a SSI [29]
Superficial incisional SSI
Infection occurs within 30 days after the operation and infection involves only skin or subcutaneous tissue of the incision and at least one of the following:
Purulent drainage, with or without laboratory confirmation, from the superficial incision.
Organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision.
At least one of the following signs or symptoms of infection: pain or tenderness, localized swelling, redness, or heat and superficial incision is deliberately opened by surgeon, unless incision is culture-negative.
Diagnosis of superficial incisional SSI by the surgeon or attending physician.
Deep incisional SSI
Operation related infection involving deep soft tissues which occurs within 30 days after the operation and at least one of the following:
Purulent drainage from the deep incision but not from the organ/space component of the surgical site.
A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms: fever (> 38 °C), localized pain, or tenderness, unless site is culture-negative.
An abscess or other evidence of infection involving the deep incision is found on direct examination, during reoperation, or by histo-pathologic or radiologic examination.
Diagnosis of a deep incisional SSI by a surgeon or attending physician.
Endometritis [30]
Must meet at least one of the following criteria:
Patient has organism(s) identified from endometrial fluid or tissue by a culture or non-culture based microbiologic testing method which is performed for purposes of clinical diagnosis or treatment.
Patient has at least two of the following signs or symptoms: fever (> 38.0 °C), pain or tenderness (uterine or abdominal), or purulent drainage from uterus
Data quality control
Proper designing and pre-testing of the questionnaires was made on 18 study participants at Debark district Hospital. Data collectors and supervisors had 1 day training before the actual data collection. Every day after data collection, questionnaires/data extraction tools were reviewed and checked for consistency and completeness by the supervisors and the necessary feedback was offered to data collectors. Any missed or incorrectly filled questionnaire was sent back to the respective data collector for correction. Epi Info version 7 was used to control Data entry errors. Data clean up and cross-checking was done before analysis.
Data processing and analysis
All the questionnaires were checked for completeness manually and coded, then entered into Epi info 7 and exported to SPSS version 20 for further analysis. Descriptive analysis results were presented in the form of tables and text using frequencies and summary statistics such as mean, standard deviation and percentage. First Bivariate binary logistic regression analysis was done to determine the crude association of each independent variable with the outcome variable via enter method. Those crudely associated independent variables with the dependent variable using odds ratio with 95% confidence interval were entered via backward likelihood ratio for multivariate binary logistic regression analysis to adjust the influence of various independent variables (confounding effect) on the outcome variable. The Hosmer and Lemeshow (HL) test was used to check model fitness in our study. According to HL, if the significance value is more than 0.05, it indicates the model fits data well [31]. The HL test indicated that our final model was fit (p = 0.605). Odds ratio with 95% confidence interval were used to estimate the strength of the association between independent variables and dependent variable.
Results
Socio-demographic and medical characteristics
A total of 334 women were included in the study, making 96.25% response rate (Fig. 1). The age of the study participants were between 17 and 43 years with mean (±SD) age 26.38 ± 5.47 years. All of them were married and from Amhara ethnicity. About 96% of them were orthodox Christians and about 59% of them have attended secondary and above education. More than two-thirds (69%) of them were urban dwellers.
The health status of about 70% of study participants was ASA class I, about 8% of them were chronic hypertensive cases and 4.5% of them had preexisting anemia (Table 1).
Table 1.
Socio demographic and medical characteristics of study participants of SSI and associated factors among CDs at DGH, 2017. (n = 334)
| Variable | Frequency | Percent (%) |
|---|---|---|
| Age | ||
| < 20 | 47 | 14.1 |
| 20–34 | 232 | 74.4 |
| 35–49 | 35 | 10.5 |
| Residence | ||
| Urban | 232 | 69.5 |
| Rural | 102 | 30.5 |
| Educational status | ||
| Unable to read and write | 56 | 16.8 |
| Primary education | 79 | 23.6 |
| Secondary and above | 199 | 59.6 |
| Religion | ||
| Orthodox | 322 | 96.4 |
| Muslim | 12 | 3.6 |
| Health status | ||
| ASA class I | 238 | 71.2 |
| ASA class II | 48 | 14.4 |
| ASA class III | 48 | 14.4 |
| Chronic hypertension | ||
| Yes | 28 | 8.4 |
| No | 306 | 91.6 |
| Diabetes mellitus | ||
| Yes | 5 | 1.5 |
| No | 329 | 98.5 |
| Heart disease | ||
| Yes | 9 | 2.7 |
| No | 325 | 97.3 |
| Pre-existing anemia | ||
| Yes | 15 | 4.5 |
| No | 319 | 95.5 |
| Obesity | ||
| Yes | 14 | 4.2 |
| No | 320 | 95.8 |
ASA American society of Anesthesiologists
Pregnancy and labor related characteristics
About 43 and 50% of participants were primigravidas and primiparas respectively with respective mean gravity and mean parity status of 2.28 times and 1.59 times. The maximum number of gravidity and parity was nine pregnancies and eight deliveries respectively. About 78% of them had term pregnancy and bout 86% of them had ANC follow up. At least one form of PIH (either gestational hypertension, pre eclampsia or eclampsia) were diagnosed in 27.1% of study participants.
On labor status of study participants, about 75% of them had labor before the operation and about 43% of them had ruptured membrane before the operation with the mean duration of 14 h and 10.51 h respectively. Eleven percent of participants had either preoperative or intraoperative chorioaminitis based on clinical findings (Table 2).
Table 2.
Pregnancy and labor related characteristics of study participants of SSI and associated factors among CDs at DGH, 2017. (n = 334)
| Variable | Frequency | Percent (%) |
|---|---|---|
| Gravidity | ||
| 1 | 143 | 42.8 |
| 2–4 | 150 | 44.9 |
| ≥ 5 | 41 | 12.3 |
| Parity | ||
| 1 | 169 | 50.6 |
| 2–4 | 124 | 37.1 |
| ≥ 5 | 41 | 12.3 |
| Ante natal care follow-up | ||
| Yes | 288 | 86.2 |
| No | 46 | 13.8 |
| Pregnancy induced hypertension | ||
| Yes | 57 | 27.1 |
| No | 277 | 82.9 |
| Gestational diabetes mellitus | ||
| Yes | 5 | 1.5 |
| No | 329 | 98.5 |
| Gestational age | ||
| Preterm | 47 | 14.1 |
| Term | 260 | 77.8 |
| Post term | 27 | 8.1 |
| Steroid therapy | ||
| Yes | 38 | 11.4 |
| No | 296 | 88.6 |
| Labor before the operation | ||
| No labor | 84 | 25.1 |
| Yes (≤24 h) | 199 | 59.6 |
| Yes (> 24 h) | 51 | 15.3 |
| Way of labor initiation | ||
| No labor | 84 | 25.1 |
| Spontaneous | 195 | 58.4 |
| Induced | 55 | 16.5 |
| Vaginal examination | ||
| No | 38 | 11.4 |
| Yes (≤5) | 114 | 34.1 |
| Yes (> 5) | 182 | 54.5 |
| Status of membrane | ||
| Intact | 189 | 56.6 |
| Ruptured (≤ 12 h) | 108 | 32.3 |
| Ruptured (> 12 h) | 37 | 11.1 |
| Chorioaminitis | ||
| Yes | 40 | 12 |
| No | 294 | 88 |
Intra operation and post operation related variables
Of the total operations about 86% of them were emergency CDs. About 31% of indications for CD was NRFHRP (Table 3), Abdomen was entered via pfannensteil incision for about 87% of operations and lower uterine segment transverse cesarean section was done for all cases. Almost all wounds were clean contaminated wounds and skin was closed via sub cuticular suture for about 93% of case. About 57% of operations were done by integrated emergency surgical officers and about 17% of participants had post operation haemoglobin value of less than 11 g/decilitre (g/dl) (Table 4).
Table 3.
Indication for cesarean section of study participants of SSI and associated factors among CDs at DGH, 2017. (n = 334)
| Indication | Frequency | Percent (%) |
|---|---|---|
| Non reassuring fetal heart rate pattern | 103 | 30.8 |
| Non reassuring biophysical profile | 32 | 9.6 |
| Cephalo-pelvic disproportion | 46 | 13.8 |
| Previous scar | 34 | 10.2 |
| Breech | 23 | 6.9 |
| Failed induction | 17 | 5.1 |
| Cervical arrest | 15 | 4.5 |
| Failed instrumental delivery | 14 | 4.2 |
| Placenta Previa | 13 | 3.9 |
| Twin | 12 | 3.6 |
| Transverse lie | 7 | 2.1 |
| Cord prolapse | 5 | 1.5 |
| Othersa | 13 | 3.9 |
| Total | 334 | 100 |
aOthers: Macrosomia, Cord presentation, Triplet
Table 4.
Intra operation and post operation related characteristics of study participants of SSI and associated factors among CDs at DGH, 2017. (n = 334)
| Variable | Frequency | Percent (%) |
|---|---|---|
| Type of cesarean delivery | ||
| Emergency | 287 | 85.9 |
| Elective | 47 | 14.1 |
| Time Prophylaxis antibiotics given | ||
| ≤ 1 h before the operation | 300 | 89.8 |
| > 1 h before the operation | 34 | 10.2 |
| Skin incision | ||
| Pfannensteil | 291 | 87.1 |
| Midline | 43 | 12.9 |
| Procedure duration | ||
| ≤ 1 h | 331 | 99.1 |
| > 1 h | 3 | .9 |
| Dis-impaction of head | ||
| Yes | 8 | 2.4 |
| No | 333 | 97.6 |
| Estimated blood loss | ||
| ≤ 500 ml | 328 | 98.2 |
| > 500 ml | 6 | 1.8 |
| Intra-operation transfusion | ||
| Yes | 6 | 1.8 |
| No | 328 | 98.2 |
| Wound class | ||
| Clean contaminated | 325 | 97.3 |
| Contaminated | 9 | 2.7 |
| Skin closure | ||
| Interrupted | 22 | 6.6 |
| Sub-cuticular | 312 | 93.4 |
| Qualification of surgeon | ||
| Integrated emergency surgical officer | 191 | 57.2 |
| Obstetrician and gynecologist | 143 | 42.8 |
| Experience | ||
| 2–3 years | 120 | 36 |
| > 3 years | 214 | 64 |
| Post-operative hemoglobin | ||
| < 11 g/dl | 59 | 17.7 |
| ≥ 11 g/dl | 275 | 82.3 |
hr hour, Ml: milliliter, g/dl gram/ deciliter
Proportion of SSI
Of the total 334 study participants, 27 of them had developed SSI, making proportion of 8.1% (95%Cl: 5.4, 11.6). Three of them were identified before discharge and the remaining 24 were traced through follow up and readmission. All SSI cases were superficial incisional wound infection developed from emergency CDs.
Factors associated with surgical site infection
In bivariate logistic regression analysis, SSI was significantly associated with ASA class III health status classification, presence of both chronic hypertension and PIH, operation after onset of labor, operation after ROM, presence of chorioaminitis, midline skin incision, interrupted skin closure, and EBL of greater than 500 ml and post-operative hemoglobin of less than 11 g/dl. Among variables found to be significantly associated with development of surgical site infection using bivariate logistic regression analysis, PIH (AOR = 4.75, 95%CI: 1.62, 13.92), chorioaminitis (AOR = 4.37, 95%CI: 1.53, 12.50), midline skin incision (AOR = 5.19, 95% CI: 1.87, 14.37 and post-operative hemoglobin less than 11 g/dl (AOR = 5.28, 95%CI: 1.97, 14.18) were also found to be significant in multivariate logistic regression analysis (Table 5).
Table 5.
Bivariate and multivariate logistic regression analysis of Factors Associated with SSI among cesarean deliveries at DGH, 2017. (n = 334)
| Variable | SSI | COR (95% CI) | AOR (95% CI) | P value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Frequency | Frequency | ||||
| Health status based on ASA | |||||
| Class I | 13 | 225 | Reference | ||
| Class II | 6 | 42 | 2.47 (.89, 6.87) | ||
| Class III | 8 | 40 | 3.46 (1.35, 8.89) | ||
| Chronic hypertension | |||||
| Yes | 6 | 22 | 3.7 (1.35, 10.12) | ||
| No | 21 | 285 | Reference | ||
| PIH | |||||
| Yes | 12 | 45 | 4.66 (2.05,10.60) | 4.75 (1.62, 13.92) | 0.000 |
| No | 15 | 262 | Reference | ||
| Labor status | |||||
| Yes | 25 | 225 | 4.56 (1.06, 19.66) | 4.53 (.95, 21.57) | |
| No | 2 | 82 | Reference | ||
| Membrane status | |||||
| Ruptured | 19 | 126 | 3.41 (1.45, 8.04) | ||
| Intact | 8 | 181 | Reference | ||
| Chorioaminitis | Frequency | Frequency | |||
| Yes | 12 | 28 | 7.97 (3,40,18.70) | 4.37 (1.53,12.50) | 0.000 |
| No | 15 | 279 | Reference | ||
| Skin incision | |||||
| Midline | 12 | 31 | 7.12 (3.06, 16.58) | 5.19 (1.87,14.37) | 0.000 |
| Pfannensteil | 15 | 276 | Reference | ||
| Skin closure | |||||
| Interrupted | 7 | 15 | 6.81(2.49, 18.61) | ||
| Sub-cuticular | 20 | 292 | Reference | ||
| EBL | |||||
| ≤ 500 ml | 24 | 304 | Reference | ||
| > 500 ml | 3 | 3 | 12.67(2.42,66.18) | ||
| Post OP Hgb | |||||
| < 11 mg/dl | 15 | 44 | 7.47 (3.28, 17.02) | 5.28 (1.97, 14.18) | 0.000 |
| ≥ 11 mg/dl | 12 | 263 | Reference | ||
Discussion
This study assessed proportion of SSI among CDs and found 8.1% [14] of CDs developed SSI (95%Cl: 5.4, 11.6).
This finding was in line with findings in Cambodia-6.25% [32], Pennsylvania-6.5% [19], Thai-Myanmar border hospital-5.9 [20], London-9.8% [33], Ankara-6.2% [12], sub Saharan Africa-7.3% [34], Egypt-9% [22], Tanzania-10.9% [8], Hawassa Teaching and Referral Hospital-11% [16], Assela Teaching and Referral Hospital-9.4% [17] and a study done in Lemlem Karl General Hospital-6.8% [18].
The result was high when compared with study done in Nanjing-3.34% [9]. This might be due a difference in quality of surgical care provision, the later assumed to have high quality service. The finding was also high when compared with another study done in southern India [35] where 4.1% of CDs had developed SSI. The possible explanation might be the magnitude represented those SSI cases developed only in first post-operative week. The result was also high when compared with a study done Israel-3.7% [13]. This difference again might reveal the difference in the quality of surgical care provisions as the later country is expected to deliver high quality service. The magnitude was again high when compared with the finding in Rwanda − 4.9% [14]. This might be due to the difference in provision of quality standard surgical care.
The magnitude of SSI was lower when compared with a study done in Nepal [10] and India [36], where 12.6, 13% and of CDs ended up with SSI respectively. These discrepancies might be tailored to differences in sample size and the difference in duration between the studies. On the other hand, SSI was diagnosed in 24.3% of Karachi [11] women following Their CD, three times higher than the finding of this study. High prevalence of obesity and diabetes mellitus among Karachi women might have contributed for such an increase SSI rate. The proportion of SSI following CDs in Nnewi (Nigeria) [21] was 12.5% that is high when compared with this study. This might be due midline skin incision was used for all previous scar cases in Nigeria which in turn is presumed to be responsible for higher rates of SSI.
The result was again low when compared with the finding of an observational study done in Tanzania [15] where 48.2% of women were found having SSI following CDS. This might be due to the difference in study setting, the later done in tertiary hospital where flow of referral cases are expected to be high.
Mothers with PIH were about five times (AOR = 4.75, 95%CI: 1.62, 13.92) more likely to develop SSI than those mothers without the problem. This finding is consistent with the findings of previous studies done in Israel [13] and Tanzania [8]. The possible explanation might be hypo perfusion of the wound caused by peripheral vasoconstriction effect of PIH. In addition those mothers with such problems might have edematous wound edges responsible for further entry of organisms and establishment of infection.
Mothers with chorioaminitis were also about four point four times (AOR = 4.37, 95%CI: 1.53, 12.50) more likely to develop SSI than those mothers without the problem. This finding is in line with the findings of the studies done in Pennsylvania [19], china [9], Thailand [20], Burkina Faso [37] and Assela [17]. This is because organisms responsible for chorioaminitis might use metritis as focus of infection and disseminate through systemic circulation to easily establish wound infection.
Operations done via midline skin incision were about five times (AOR = 5.19, 95% CI: 1.87, 14.37 more likely to develop SSI than operations done via pfannensteil incision. There are similar associations among studies done in Nepal [10], Nigeria [21], Tanzania [15], Assela [17] and Maichew [18]. The reason might be vertical incisions are more likely to be affected by intra-abdominal pressure which in turn might be responsible for poor skin integrity thereby facilitating entry of organisms and development of SSI. In addition, vertical incision has low perfusion of gases and nutrients compared with transverse incision thereby delaying would healing and increasing the likely of infection. Additional explanation might be because of prolonged duration of surgery.
Those Mothers whose post-operative hemoglobin level was less than 11 g/dl were about five point three times (AOR = 5.28, 95%CI: 1.97, 14.18) more likely to develop SSI than mothers whose hemoglobin was greater than or equal to 11 g/dl. This finding is similar with the findings of other studies done in Thailand [20], Oman [38] and Hawassa [16]. The reason behind might be due to hypo perfusion of the wound secondary to anemia and reduced post-operative ambulation.
As a limitation this study had excluded 12 study participants for the sake of tracing mechanism which might have impact on the above result. The other limitation was possible information bias as the data collectors were staffs of the same hospital. Small sample size and short period of the study were also among the limitations of this study.
Conclusions
According to this study proportion of SSI following CDs in DGH was found to be significant in this country. PIH, chorioaminitis, midline skin incision and post-operative hemoglobin of less than 11 g/dl were independent factors associated with development of SSI. CDs with concomitant PIH, chorioaminitis and post-operative anemia needs special care and follow up until SSI is ruled out. It is also advisable to replace generous midline skin incision with pfannensteil incision.
Acknowledgements
We are very grateful to Department of Midwifery, College of Medicine and health sciences, University of Gondar for the approval of the ethical clearance and funding of the design and data collection cost of this research project. We would also like to thank all women who participated in this study, supervisors, the data collectors and the staff members at the hospital.
Abbreviations
- AOR
Adjusted Odds Ratio
- ASA
American Society of Anesthesiologists
- BMI
Body Mass Index
- CD
Cesarean Delivery
- CDC
Center for Disease Control and prevention
- CDs
Cesarean Deliveries
- CI
Confidence Interval
- COR
Crude Odds Ratio
- CS
Cesarean Section
- DGM
Debretabor General Hospital
- DM
Diabetes Mellitus
- EBL
Estimated Blood Loss
- GDM
Gestational Diabetes Mellitus
- IRB
Institutional Review Board
- NRFHRP
Non Reassuring Fetal Heart Rate Pattern
- PIH
Pregnancy Induced Hypertension
- ROM
Rupture of Membrane
- SPSS
Statistical Package for Social Sciences
- SSI
Surgical Site Infection
Authors’ contributions
MM wrote the proposal, supported and supervised data collection, analyzed the data and drafted the paper. KT, TS and MeM approved the proposal with some revisions, participated in data analysis and revised subsequent drafts of the paper. All authors read and approved the final manuscript.
Authors’ information
1. Mihretu Molla Enyew
Lecturer of Midwifery at university of Gondar
2. Kiber Temesgen
Lecturer of Midwifery at university of Gondar
3. Tewodros Syoum
Assistant professor of midwifery at university of Gondar
4. Mengstu Melkamu
Lecturer of midwifery at university of Gondar
Funding
The funding body (university of Gondar) had a role in covering of the financial costs related with the design and data collection of this study. However, the funding body had no role in the analysis, interpretation of data and in writing of the manuscript.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
Ethical approval was obtained from department of midwifery Ethical Review Committee under the delegation of IRB of University of Gondar (reference number: MIDW/10/263/09). Written consent was obtained from study participants prior to data collection. Study participants who were ≥ 18 years of age gave their written consent. Study participants who were < 18 years of age gave their written consent via their family members. Family members used to provide consent on the behalf of participants under the age of 18 were participants’ husbands and either of the participants’ parents. Priority was given for husbands and parents were considered in cases of either husbands’ absence or husbands’ minority age (under 18 years of age). We can confirm that the ethics committee had approved the use of attendants (husband or either of the parents) on the behalf of participants under the age of 18.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mihretu Molla, Email: mihretumolla143@gmail.com.
Kiber Temesgen, Email: kibermosu@gmail.com.
Tewodros Seyoum, Email: tedysha@gmail.com.
Mengstu Melkamu, Email: mengstum@gmail.com.
References
- 1.Berríos-Torres Sandra I., Umscheid Craig A., Bratzler Dale W., Leas Brian, Stone Erin C., Kelz Rachel R., Reinke Caroline E., Morgan Sherry, Solomkin Joseph S., Mazuski John E., Dellinger E. Patchen, Itani Kamal M. F., Berbari Elie F., Segreti John, Parvizi Javad, Blanchard Joan, Allen George, Kluytmans Jan A. J. W., Donlan Rodney, Schecter William P. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surgery. 2017;152(8):784. doi: 10.1001/jamasurg.2017.0904. [DOI] [PubMed] [Google Scholar]
- 2.Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276–ee87. doi: 10.1016/S1473-3099(16)30398-X. [DOI] [PubMed] [Google Scholar]
- 3.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Am J Infect Control. 1999;27(2):97–134. doi: 10.1016/S0196-6553(99)70088-X. [DOI] [PubMed] [Google Scholar]
- 4.Allegranzi B, Bischoff P, Kubilay Z, de Jonge S, Zayed B, Sudan R, et al. Global guidelines for the prevention of surgical site infection. World Health Organization; 2016. [PubMed]
- 5.Kirchengast S. Caesarean section: from the viewpoint of evolutionary medicine. 2017. [Google Scholar]
- 6.Saeed Khalid B M, Greene Richard A, Corcoran Paul, O'Neill Sinéad M. Incidence of surgical site infection following caesarean section: a systematic review and meta-analysis protocol. BMJ Open. 2017;7(1):e013037. doi: 10.1136/bmjopen-2016-013037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaiyeoba O. Postoperative infections in obstetrics and gynecology. Clin Obstet Gynecol. 2012;55(4):904–913. doi: 10.1097/GRF.0b013e3182714734. [DOI] [PubMed] [Google Scholar]
- 8.Mpogoro FJ, Mshana SE, Mirambo MM, Kidenya BR, Gumodoka B, Imirzalioglu C. Incidence and predictors of surgical site infections following caesarean sections at Bugando medical Centre, Mwanza, Tanzania. Antimicrob Resist Infect Control. 2014;3(1):25. doi: 10.1186/2047-2994-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng K, Li J, Kong Q, Wang C, Ye N, Xia G. Risk factors for surgical site infection in a teaching hospital: a prospective study of 1,138 patients. Patient Prefer Adherence. 2015;9:1171. doi: 10.2147/PPA.S86153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shrestha S, Shrestha R, Shrestha B, Dongol A. Incidence and risk factors of surgical site infection following cesarean section at Dhulikhel hospital. Kathmandu Univ Med J. 2015;12(2):113–116. doi: 10.3126/kumj.v12i2.13656. [DOI] [PubMed] [Google Scholar]
- 11.Jabbar S, Perveen S, Naseer Q. Surgical site infection (SSI): frequency and risk factors in post caesarean section cases in a tertiary care hospital. ASH KMDC. 2016;21(4):233–239. [Google Scholar]
- 12.Çınar M, Timur H, Güzel Aİ, Tokmak A, Ersak B, Saygan S, et al. The association between preterm premature rupture of membranes and surgical site infection following cesarean section. Gynecol Obstet Reprod Med. 2016;22(3):139–43.
- 13.Salim R, Braverman M, Teitler N, Berkovic I, Suliman A, Shalev E. Risk factors for infection following cesarean delivery: an interventional study. J Matern Fetal Neonatal Med. 2012;25(12):2708–12. doi: 10.3109/14767058.2012.705394. [DOI] [PubMed] [Google Scholar]
- 14.Bizimana JK, Ndoli J, Bayingana C, Baluhe I, Gilson G, Habimana E. Prevalence and risk factors for post cesarean delivery surgical site infection in a teaching hospital setting in rural Rwanda: a prospective cross sectional study. Int J Curr Microbiol App Sci. 2016;5(6):631–641. doi: 10.20546/ijcmas.2016.506.069. [DOI] [Google Scholar]
- 15.De Nardo P, Gentilotti E, Nguhuni B, Vairo F, Chaula Z, Nicastri E, et al. Post-caesarean section surgical site infections at a Tanzanian tertiary hospital: a prospective observational study. J Hosp Infect. 2016;93(4):355–359. doi: 10.1016/j.jhin.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 16.Wodajo S, Belayneh M, Gebremedhin S. Magnitude and factors associated with post-cesarean surgical site infection at Hawassa University teaching and referral hospital, southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. 2017;27(3):283–290. doi: 10.4314/ejhs.v27i3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mamo T, Abebe TW, Chichiabellu TY, Anjulo AA. Risk factors for surgical site infections in obstetrics: a retrospective study in an Ethiopian referral hospital. Patient Saf Surg. 2017;11(1):24. doi: 10.1186/s13037-017-0138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gelaw KA, Aweke AM, Astawesegn FH, Demissie BW, Zeleke LB. Surgical site infection and its associated factors following cesarean section: a cross sectional study from a public hospital in Ethiopia. Patient Saf Surg. 2017;11(1):18. doi: 10.1186/s13037-017-0131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shree R, Park SY, Beigi RH, Dunn SL, Krans EE. Surgical site infection following cesarean delivery: patient, provider, and procedure-specific risk factors. Am J Perinatol. 2016;33(02):157–164. doi: 10.1055/s-0035-1563548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assawapalanggool S, Kasatpibal N, Sirichotiyakul S, Arora R, Suntornlimsiri W. Risk factors for cesarean surgical site infections at a Thai-Myanmar border hospital. Am J Infect Control. 2016;44(9):990–995. doi: 10.1016/j.ajic.2016.01.031. [DOI] [PubMed] [Google Scholar]
- 21.Onyegbule OA, Akujobi CN, Ezebialu IU, Nduka AC, Anahalu IC, Okolie VE, et al. Determinants of post-caesarean wound infection in Nnewi. Nigeria: Journal of Advances in Medicine and Medical Research; 2015.
- 22.Borg TF, Aly KK, Salahaldeen AS, Alkallaf AS. Incidence and risk factors for surgical site infections following cesarean section in a tertiary care university hospital versus a rural hospital: a prospective, two-armed parallel cohort study. J Evid Based Womens Health J Soc. 2016;6(2):51–57. doi: 10.1097/01.EBX.0000481362.51250.6c. [DOI] [Google Scholar]
- 23.McKibben RA, Pitts SI, Suarez-Cuervo C, Perl TM, Bass EB. Practices to reduce surgical site infections among women undergoing cesarean section: a review. Infect Control Hosp Epidemiol. 2015;36(8):915–921. doi: 10.1017/ice.2015.116. [DOI] [PubMed] [Google Scholar]
- 24.Vallejo Manuel C., Attaallah Ahmed F., Shapiro Robert E., Elzamzamy Osama M., Mueller Michael G., Eller Warren S. Independent risk factors for surgical site infection after cesarean delivery in a rural tertiary care medical center. Journal of Anesthesia. 2016;31(1):120–126. doi: 10.1007/s00540-016-2266-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De D, Saxena S, Mehta G, Yadav R, Dutta R. Risk factor analysis and microbial etiology of surgical site infections following lower segment caesarean section. Int J Antibiot. 2013;2013:1–6. doi: 10.1155/2013/283025. [DOI] [Google Scholar]
- 26.Jido T, Garba I. Surgical-site infection following cesarean section in Kano, Nigeria. Ann Med Health Sci Res. 2012;2(1):33–36. doi: 10.4103/2141-9248.96934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berhan Y, Berhan A. Causes of maternal mortality in Ethiopia: a significant decline in abortion related death. Ethiop J Health Sci. 2014;24:15–28. doi: 10.4314/ejhs.v24i0.3S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amenu D, Belachew T, Araya F. Surgical site infection rate and risk factors among obstetric cases of Jimma University specialized hospital, Southwest Ethiopia. Ethiop J Health Sci. 2011;21(2):91–100. doi: 10.4314/ejhs.v21i2.69049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Surgical site infection (SSI) event: procedure-associated module. 2016. [Google Scholar]
- 30.Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. Atlanta: CDC; 2017.
- 31.Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. Wiley; 2013.
- 32.Srun S, Sinath Y, Seng AT, Chea M, Borin M, Nhem S, et al. Surveillance of post-caesarean surgical site infections in a hospital with limited resources, Cambodia. J Infect Dev Ctries. 2013;7(8):579–585. doi: 10.3855/jidc.2981. [DOI] [PubMed] [Google Scholar]
- 33.Wilson J, Wloch C, Saei A, McDougall C, Harrington P, Charlett A, et al. Inter-hospital comparison of rates of surgical site infection following caesarean section delivery: evaluation of a multicentre surveillance study. J Hosp Infect. 2013;84(1):44–51. doi: 10.1016/j.jhin.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 34.Chu K, Maine R, Trelles M. Cesarean section surgical site infections in sub-Saharan Africa: a multi-country study from Medecins sans Frontieres. World J Surg. 2015;39(2):350–355. doi: 10.1007/s00268-014-2840-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haq A, Abdullah A, Akhtar S. Analysis of risk factors in surgical site infection following caesarean section. Int J Reprod Contracept Obstet Gynecol. 2016;5(12):4256–62.
- 35.Vijayan C, Mohandas S, Nath AG. Surgical site infection following cesarean section in a teaching hospital. Int J Sci Study. 2016;3(12):97–101. [Google Scholar]
- 37.Kaboré B, Soudouem G, Seck I, Millogo T, Yaméogo WME, Kouanda S. A case–control study of risk factors for surgical site infection after cesarean delivery in eastern Burkina Faso. Int J Gynecol Obstet. 2016;135:S107–SS10. doi: 10.1016/j.ijgo.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 38.Dhar H, Al-Busaidi I, Rathi B, Nimre EA, Sachdeva V, Hamdi I. A study of post-caesarean section wound infections in a regional referral hospital, Oman. Sultan Qaboos Univ Med J. 2014;14(2):e211. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].


