1 |. INTRODUCTION
Despite efforts to protect patients against high out-of-pocket (OOP) cost burden, the cost of necessary medical care remains a significant problem for many Americans.1 The OOP costs associated with treatment and management of cancer may be particularly burdensome to patients. According to the Medical Panel Expenditure Survey (MEPS) (the authors’ own analysis), from 2008 to 2016, yearly OOP costs for households with a cancer survivor averaged $2304 (median $1344).2 The strain associated with high-cost medical care has been the subject of increased research in recent years, with studies showing detrimental effects to quality of life, treatment adherence, and even survival.3–5
Treatment-related financial strain may affect more than individuals living with cancer. Studies describe physical and psychosocial needs and outcomes for caregivers,6 but less attention is given to how medical costs affect members of the household. In this brief, we highlight that the impact of high-cost medical care can have both to individuals living with cancer and to other members of the household.
2 |. DATA AND METHODS
The MEPS is an ongoing, nationally representative, cross-sectional survey of noninstitutionalized US residents.2 The survey collects individual-level data on medical costs—including patient-paid costs (supplemented by hospital, physician, and pharmacy records collected by Agency for Healthcare Research and Quality [AHRQ])—health insurance coverage, socio-demographics, and other self-reported health metrics over 2 years.Wecombine data from 2008 through 2016.
The sample of adults (aged ≥ 18 y) includes two groups: those (1) previously diagnosed with cancer of any type (excluding nonmelanoma skin cancers) by self-report or (2) residing in a household with a cancer patient. Subgroup analyses stratify by insurance type. OOP costs are defined as the amount paid by the individual not reimbursed by insurance or other aid, including deductibles, copayments, and insurance premiums as well as any additional self-financed medical bills. Categorical exposure of financial burden was constructed as follows: total household-paid medical costs less than 5%, 5% to 10%, and exceeding 10% of household income.
Also contained within the MEPS, the SF-12v2 is a validated 12-item quality-of-life questionnaire with domains for physical and mental health.7 Scores are normalized between 0 and 100, where higher scores indicate better health and 50 represents the US national average. We use the mental health component score as a measure of mental health well-being—an outcome shown to be directly affected by OOP medical financial burden.4
We took a number of steps to mitigate an obvious association between self-reported well-being and more frequent/advanced disease. First, we control for clinical and socio-demographic characteristics, including age, sex, race/ethnicity, education, and family size. We also include measures of general disease burden including individual comorbidities, self-reported physical health well-being, and total amount spent on all medical care as a household to proxy severity of illness. Next, we present a set of heterogenous effects by insurance type to account for differences in cost exposure and burden of disease across insurance. Finally, we tested alternative specifications (not shown), including alternative measurements of comorbidities, thresholds for OOP cost as a percent of household income, and time-series modeling—none of which qualitatively affected our main findings.
Survey-weighted multiple linear regression models produce adjusted mean mental health well-being scores, by financial burden level, for those with cancer and those living with someone with cancer, respectively. All models account for the MEPS sampling design in the estimates of variance. Primary analyses are complete case, with less than 10% missingness across the full sample. Additional models stratified by insurance type include the following: Medicare, Medicaid, private insurance, and uninsured—each of which generates policy interest with respect to cancer and cancer care costs.
3 |. RESULTS
The sample includes 8257 cancer patients and 7475 household members representing 29 959 person-years from 2008 to 2016. Of the household members, 5594 (75%) were spouse or domestic partner to cancer patients. Median household income was $55 550, and median spending on medical care was 2.4% of household income. Total medical expenses paid OOP exceeded 10% of household income for 13.9% of the population, 5% to 10% of household income for 14.1% of the population, and less than 5% for 72.0% of the population (additional sample characteristics, Table S1).
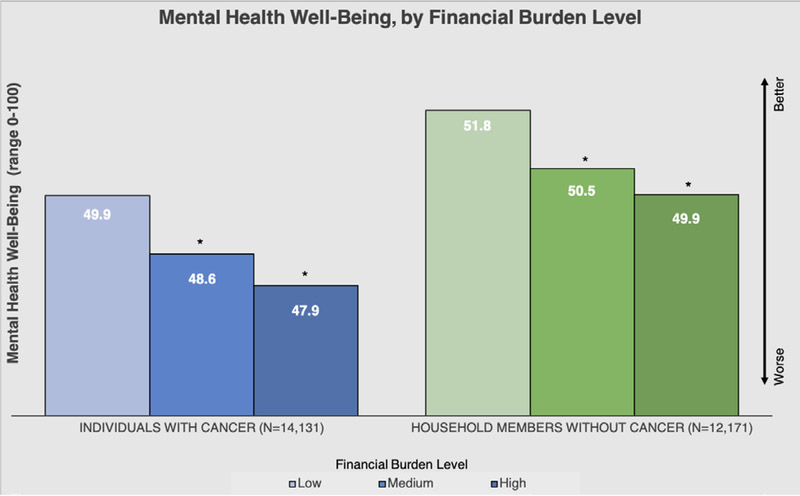
The adjusted differences by financial burden are nearly identical for cancer and household member groups (Figure 1). For individuals with cancer, there is a 1.30 (95% CI, 0.64–1.95) unit reduction in mental health score when medical expenditures are 5% to 10% of household income relative to those spending less than 5% of household income on medical costs. For those, in the same household as someone with cancer, this difference is 1.33 (059–2.06). Higher financial burden (>10% of household income) increases the magnitude of the association to 1.97 (1.23–2.71) and 1.87 (1.07–2.66) for cancer and household members, respectively. A full table of regression results is available in Table S2.
FIGURE 1.
*Statistically distinguishable from the “Less than 5%” group (P < 0.05). Data from the Medical Panel Expenditure Survey (MEPS) 2008 to 2015. Financial burden is defined as percent of household income spent on out-of-pocket medical costs (low = <5%; medium = 5%−10%; high = >10%)
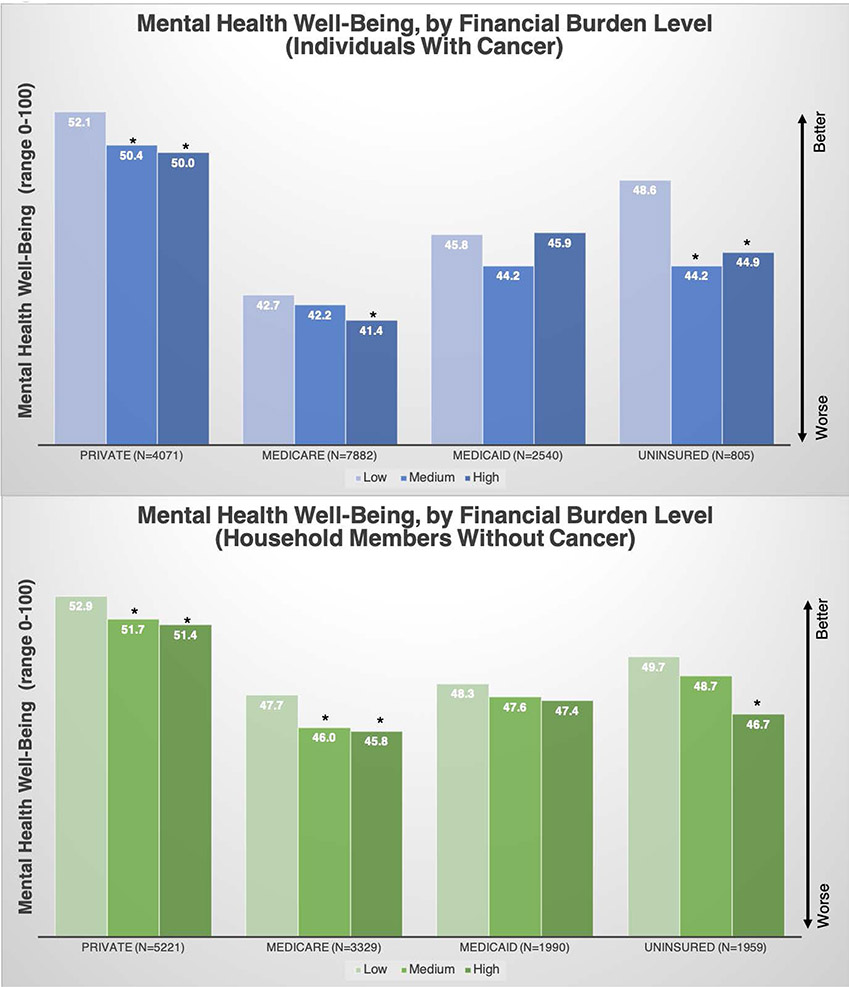
All insurance groups exhibit a similar pattern of lower quality of life at higher OOP costs, controlling for other measures of health, though for Medicaid enrollees, a smaller subgroup, this difference is not statistically distinguishable from 0 at traditional significance levels (Figure 2). As above, the effect of OOP spending on mental health is similar across cancer and household member groups. The uninsured and privately insured show the largest difference in mental health well-being comparing low vs high financial burden (cancer private = 2.12 [0.722−3.51]; cancer uninsured = 4.39 [0.97−7.81]) (adjusted mean mental component score [MCS] by insurance group available in Table S3).
FIGURE 2.
*Statistically distinguishable from the “Less than 5%” group (P < 0.05). Data from the Medical Panel Expenditure Survey (MEPS) 2008 to 2015. Financial burden is defined as percent of household income spent on out-of-pocket medical costs (low = <5%; medium = 5%−10%; high = >10%)
4 |. DISCUSSION
The dialog around cancer care financial burden is often appropriately focused on the needs of patients. However, this brief presents data suggesting that other members of the household may also be affected by high financial burden. We find that this association is robust to controls for health status, household structure, and social determinants.
The association between OOP cost burden and mental health well-being among cancer patients and noncancer household members also persists across insurance types, though to varying degrees. For Medicaid beneficiaries, the difference between high and low OOP cost is considerably smaller (<1 unit on the SF12 1–100 scale) than the same difference in the uninsured (>3 units). One would expect the uninsured to be strongly affected by different tiers of OOP cost relative to income but might expect the same in Medicaid. One explanation for this difference posits that at very low levels of income, mental health scores are already low and any cost is burdensome—the difference between 2%, 5%, and 10% OOP costs may not be as meaningful.
Both Medicare and privately insured individuals experience differences across financial burden levels similar to the full sample average. Notably, Medicare beneficiaries with cancer report considerably lower mental health scores at baseline (42.7 compared with 52.1 with private insurance). We attribute this potentially to an increased risk of poor prognosis, as well as competing comorbidity in the Medicare population.8
Our primary finding—that household members living with cancer patients experience similar decrement to mental health well-being from financial burden as their cancer cohabitants—is consistent with a considerable literature on caregiver burden in cancer. Studies have shown increased fatigue, lost hours of work, and overall lower quality of life for caregivers, especially in cases of advanced disease.9 Our findings suggest that financial burden may add to or even compound family and caregiver strain. Additional research is needed to separate and elucidate these effects, including how marital status, number and age of dependents, and family support modify management of cancer care costs.
Our research underscores that the impact financial burden may have on families struggling with disease. Although general solutions, such as those implemented in the 2010 Patient Protection and Affordable Care Act (ACA), are intended reduce exposure to high OOP cost burden, some early research suggests that these programs, while successful in many respects, still leave some individuals at risk for high financial burden.10 We are not aware of research estimating the effect of these programs on outcomes for the larger family unit.
We are careful to highlight these data as exploratory—though we attempt to mitigate unobserved differences, it is impossible for us to be certain; we have isolated the full impact of confounding factors. Longitudinal designs or quasiexperimental methods may be able to separate these aspects to identify the causal effect of financial burden on outcomes; we urge future research in this direction. We also urge a better understanding of relationships within households as an important factor in household burden, acknowledging our own limitations and data constraints. Finally, we are limited by survey response. Errors in self-report are unavoidable but may be an acceptable tradeoff for gains in generalizability.
5 |. CONCLUSION
In recent years, patient advocacy, policy changes, and research have brought into sharp focus the potential impact of high OOP costs for patients with cancer. As we continue to explore this problem and develop solutions, it is important to broaden the scope of investigation to consider the impact of cancer-related financial burden on all household members. An environment lacking financial transparency may contribute to significant financial instability and and impact on mental health. We hope that these findings help to spark additional research and conversation—that which ultimately translates to improved policy and better outcomes for all.
Supplementary Material
Key Points.
The cost of medical care is a significant problem for many patients with a history of cancer.
Cost burden is commonly focused on patients but may equally extend to other members of the household.
Data from the Medical Panel Expenditure Survey (MEPS) support the hypothesis that individuals living in the same household as a cancer survivor may also experience lower quality of life than similar households without a cancer survivor.
We find that the decrement to quality of life associated with higher financial burden is nearly identical for cancer and household member groups.
As we explore financial burden in cancer and develop solutions, it is important to broaden the scope investigation to consider the impact on all household members.
ACKNOWLEDGEMENTS
This research was supported by the University of North Carolina’s (UNC) Cancer Care Quality Training Program (R25 CA116339).
Funding information
University of North Carolina’s (UNC) Cancer Care Quality Training Program, Grant/Award Numbers: R25 CA116339, NCI: T32CA11633
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of the article.
REFERENCES
- 1.Dixon MS, Cole AL, Dusetzina SB. Out-of-pocket spending under the affordable care act for patients with cancer. Cancer J. 2017;23(3): 175–180. 10.1097/PPO.0000000000000262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medical Panel Expenditure Survey (MEPS). Agency for Healthcare Research and Quality (AHRQ) https://meps.ahrq.gov/mepsweb/. [Google Scholar]
- 3.Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34(9):980–986. 10.1200/JCO.2015.64.6620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yousuf Zafar S, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 10.1634/theoncologist.2012-0279. 18(4):381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaisaeng N, Harpe SE, Carroll NV. Out-of-pocket costs and oral cancer medication discontinuation in the elderly. J Manag Care Pharm. 2014;20(7):669–675. 10.18553/jmcp.2014.20.7.669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307(4):398–403. 10.1001/jama.2012.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. 10.2307/3766749 [DOI] [PubMed] [Google Scholar]
- 8.Park B-W, Lee S, Lee AR, Lee K-H, Hwang SY. Quality of life differences between younger and older breast cancer patients. J Breast Cancer. 2011;14(2):112–118. 10.4048/jbc.2011.14.2.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170(12):1795–1801. http://www.ncbi.nlm.nih.gov/pubmed/15184333. Accessed August 10, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dusetzina SB, Keating NL. Mind the gap: why closing the doughnut hole is insufficient for increasing Medicare beneficiary access to oral chemotherapy. J Clin Oncol. 2016;34(4):375–380. 10.1200/JCO.2015.63.7736 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.