Fig. 1 |. Ligands and receptors transducing pro–resolving signalling in macrophages.
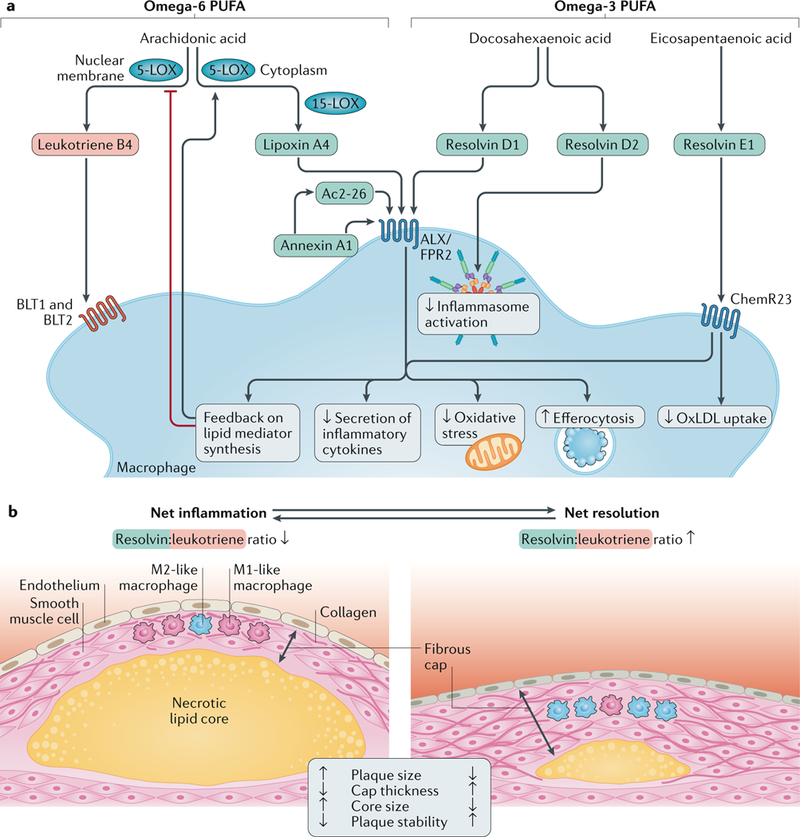
a |Specialized pro-resolving lipid mediators (in blue) include lipoxin A4, derived from the metabolism of the omega-6 polyunsaturated fatty acid (PUFA) arachidonic acid, and D-series and E-series resolvins formed from the metabolism of the omega-3 PUFAs docosahexaenoic acid and eicosapentaenoic acid, respectively. The protein pro-resolving mediator annexin A1 and the derivative peptide Ac2–26, as well as lipoxin A4 and resolvin D1, signal through N-formyl peptide receptor 2 (ALX/FPR2), whereas resolvin E1 transduces its effects through the ChemR23 receptor. These ligand-receptor interactions result in various effects, such as decreased secretion of inflammatory cytokines, reduced oxidative stress and improved efferocytosis. Resolvin E1 signalling through ChemR23 inhibits uptake of oxidized LDL (oxLDL), and resolvin D2 inhibits inflammasome activation. The ratio between pro-resolving and pro-inflammatory mediators (exemplified in the Figure by leukotriene B4 and its receptors BLT1 and BLT2) determines the macrophage phenotype. A disturbed balance in favour of pro-inflammatory pathways might serve as a marker of non-resolving inflammation in atherosclerosis. A pro-resolving amplification loop inhibits nuclear membrane localization of 5-lipoxygenase (5-LOX) and thereby further favours the formation of pro-resolving over pro-inflammatory mediators. b | Atherosclerotic plaques with net inflammation (left) and with net resolution of inflammation (right) are shown. Both atherosclerotic plaques are characterized by ongoing inflammation in which both pro-inflammatory and pro-resolving processes are concurrently active. However, the levels of these opposing processes are different in the two plaques: the resolvin:leukotriene ratio is low in the plaque with net inflammation and high in the plaque with net resolution. The plaque with net inflammation is larger and has a thin fibrous cap (with mainly pro-inflammatory M1-like macrophages, few smooth muscle cells and cleaved collagen) and a large necrotic lipid core. The plaque with net resolution is smaller and has a thicker fibrous cap (with mainly anti-inflammatory M2-like macrophages, abundant smooth muscle cells and intact collagen) and a smaller necrotic lipid core. The plaque with net inflammation is unstable and susceptible to rupture, whereas the plaque with net resolution is stable and not susceptible to rupture. During the long-lasting period of plaque development, the relative magnitude of pro-inflammatory and pro-resolving processes can vary over time. Therefore, during periods of net inflammation, plaque size tends to increase, and during periods of net resolution, plaque size tends to decrease — that is, plaque regression takes place.
