Supplemental digital content is available in the text.
Key words/Abbreviations: anxiety, attention-deficit/hyperactivity disorder, autism, depression, disorders of sex development, intersex conditions, AQ-10 = Short Autism Spectrum Quotient, ADHD = attention-deficit/hyperactivity disorder, ASRS = Adult ADHD Self-Report Scale, AIS = androgen insensitivity syndrome, BIS = Body Image Scale, CAH = congenital adrenal hyperplasia, CSQ = Customer Satisfaction Questionnaire, DSD = disorders/differences of sex development, GD = gonadal dysgenesis, HADS = Hospital Anxiety and Depression Scale, KS = Klinefelter syndrome, RSES = Rosenberg Self-Esteem Scale, TS = Turner syndrome, WHO = World Health Organization
ABSTRACT
Objective
The aim of the study was to evaluate psychiatric symptoms among 1022 persons with various disorders of sex development (DSDs).
Methods
The study was a European multicenter cross-sectional clinical evaluation in six countries. The mean (SD) age of participants was 32.1 (13.4) years. The cohort consisted of 325 individuals with Turner syndrome, 219 individuals with Klinefelter syndrome (KS), female individuals with various XY-DSD conditions (107 with and 67 without androgenization), 87 male individuals with XY-DSD conditions, and 221 female individuals with congenital adrenal hyperplasia. The Hospital Anxiety and Depression Scale, the Short Autism Spectrum Quotient, the Adult Attention-Deficit/Hyperactivity Disorder Self-Report Scale, and self-reported mental health history were used to assess psychiatric symptoms.
Results
Across the six DSD diagnostic groups, clinical cutoff symptom scores were reached in 19.5% of participants for anxiety, in 7.1% for depression, in 4.1% for attention-deficit/hyperactivity disorder, and in 9.1% for autism. The mean depression and anxiety scores were higher compared with population norms in men with KS and men with XY-DSD. Compared with participants with other DSD conditions, men with KS reported significantly more mental health symptoms. Self-esteem, satisfaction with care, body dissatisfaction, and experiences of shame were associated with psychiatric symptoms in many DSD conditions.
Conclusions
A substantial minority of adults with DSD, with KS in particular, experience psychiatric morbidity. Across DSD conditions, adults may share feelings of shame. Developing a positive self-esteem and body image may be challenging. Multidisciplinary DSD care that involves specialized mental health support can be of important value.
Trial Registration
German Clinical Trials Register DRKS00006072.
INTRODUCTION
Disorders of sex development (DSDs) are defined as congenital conditions in which the development of chromosomal, gonadal, and anatomic sex is atypical. Following the statement of the Chicago Consensus Meeting in 2005, DSDs include sex chromosome conditions (including Turner syndrome (TS), Klinefelter syndrome (KS), and mixed gonadal dysgenesis (GD) with or without androgenization, conditions with a 46,XY karyotype (including complete/partial androgen insensitivity syndrome (AIS), complete/partial GD, steroid synthesis errors, and severe hypospadias), and conditions with a 46,XX karyotype (including congenital adrenal hyperplasia (CAH), GD, and XX men) (1).
Instead of DSD, the term intersex conditions is used as well, particularly by advocacy groups (2). Because most DSD conditions are not inherently pathological terminology such as variations or differences of sex development (DSD) is often more appropriate (3). Therefore, in this article, the term DSD refers to disorders/differences of sex development. Most of the DSD conditions associated with genital ambiguity are rare (1 in 4500–5500 live births), but others such as TS and KS are much more frequent (1 in 2500 female individuals and 1 in 450–600 male individuals, respectively).(3) DSD care is surrounded by various uncertainties, for example, concerning sex assignment at birth and the timing of genital surgery, and the field of DSD is continuously developing (2,3).
According to the current consensus guidelines, psychosocial care should be an integrated part of multidisciplinary DSD management (3). Most existing knowledge on psychological functioning of people with DSD concerns psychosexual outcomes (4) and neurocognitive functioning, whereas knowledge regarding psychosocial adaptation and psychiatric morbidity in individuals with DSD is relatively sparse. The research that has been conducted is mostly within specific DSD conditions.
In women and girls with TS, an increased prevalence rate of attention-deficit/hyperactivity disorder (ADHD) and autism has been reported (5,6). Several studies also show more self-reported shyness, anxiety, and depression symptoms than controls (7) and impaired social competence, although women with TS generally seem to cope well with life (8). In men and boys with KS, psychiatric problems (bipolar, autistic, attention, and psychotic disorders) are found at increased rates compared with the general population (9–11). In male and female participants with various other XY-DSD conditions, clinically significant psychological distress is reported in 42% to 68% of participants (12–14), and high levels of anxiety, depression, behavioral problems, and suicidality have been observed (15–18). In women with CAH, an increased risk of various psychiatric disorders (alcohol misuse, stress and adjustment disorders, ADHD, increased autism traits, anxiety, and depression) compared with the healthy population has been observed (19–21). However, other studies find no psychiatric comorbidities in CAH (22,23).
Despite the diversity in clinical presentation and courses, the mere suffering from a DSD may stem from similar underlying mechanisms across the various DSD conditions. Studies show that emotional difficulties, such as anxiety and depression, may be related to the negative psychosocial impact that a DSD condition can have on self-esteem (KS, TS (24,25)) and body image (KS, TS, XY-DSD conditions (25–27)). It may also be related to negative experiences with health care (XY-DSD, XX-DSD, and CAH (28)), shame and stigma (XY-DSD conditions, CAH, (29,30)), or minority stress, which is the distress from prejudice that homosexual, lesbian, bisexual, and transgender persons experience as well (31). Intrinsic biological factors are considered to play a role in observed neurodevelopmental difficulties in several DSDs. For example, in CAH prenatal testosterone, exposure may be related to a more male typical neural development and increased self-reported autistic traits (32). In various XY-DSD conditions, these androgenization effects can also be expected. ADHD and autism symptoms in TS and KS are likely to be associated with the specific neurocognitive profile accompanying these conditions, for example, the difficulties in mental flexibility that occur in KS (33,34) and the discrepancy between good verbal capacities but poor visuospatial and executive skills that is typical in TS (35,36).
The aforementioned studies on mental health in DSD conditions are limited by the fact that they do not compare different conditions and often comprise very small sample sizes. The aim of the European Commission–funded dsd-LIFE project was to improve quality of life and clinical management of persons with DSD (37). Because mental health is strongly related to quality of life, understanding of the psychological vulnerabilities is necessary to improve health care so that it serves the specific needs of people with different DSD conditions. The objectives of the current report were to study the differences and similarities of psychiatric symptoms in a broad range of DSD conditions. Depression and anxiety symptom levels of participants were compared with the general population norms. It was further examined if psychiatric symptoms (depression, anxiety, autism, and ADHD) were associated with various factors that may affect mental health in the following DSD conditions: satisfaction with treatment/care, self-esteem, body satisfaction, and experiences of shame.
METHODS
Procedure and Participants
The methods of the multicenter cross-sectional clinical evaluation study dsd-LIFE are described in detail elsewhere (37). The dsd-LIFE consortium consisted of 16 European partners from Germany, France, the Netherlands, Poland, Sweden, and the United Kingdom, of whom 14 were active recruiting sites. Recruitment of adolescents (≥16 years old) and adults with DSD took place from February 2014 to September 2015.
The sample was a convenience sample recruited by 14 different specialized centers across six European countries and via support groups. The overall participation rate was 36% of invited persons (range = 30%–54%, the Netherlands–Sweden). Because of ethical restrictions, retrieving relevant information on, for example, diagnoses of the nonresponders and reason for nonparticipation, could not be collected, which should caution against generalizability of the results (37).
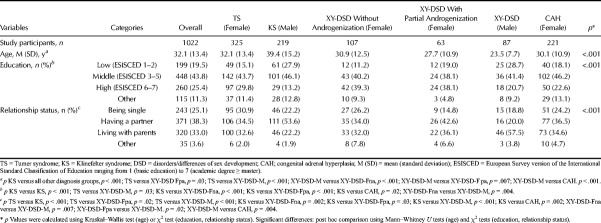
Individuals were included when being clinically diagnosed with any of the conditions stated in the Chicago consensus statement (1). A total number of 1040 persons took part in the study. The study consisted of an online patient-reported outcome questionnaire and, if participants wanted to, a hospital visit including a medical interview, physical examination, and laboratory and blood testing. Participants were classified as male, female, or other than male or female, based on how they identified in the medical interview. Participants who identified other than male or female sex or not the typical sex for the condition (e.g., a person with KS identifying as female) were excluded from the diagnosis-specific analyses (n = 18, 6 nonmale identifying KS, 5 nonfemale identifying 46,XX CAH, and 7 other sex; their mental health outcome is partly described elsewhere (3)). This way, each diagnostic group could be compared with the reference norm of either male or female. The remaining 1022 participants (716 female, 70.1%; 306 male, 29.9%) were grouped into the following six categories: 325 women with TS, 219 men with KS, 107 women with XY-DSD without androgenization effects (including complete GD, complete AIS, and XX-DSD GD), 63 women with XY-DSD with partial androgenization effects (including partial AIS, 45X/46,XY partially androgenized, and XX ovotesticular DSD), 87 men with XY-DSD, and 221 women with CAH (Table 1).
TABLE 1.
Characteristics of the Study Sample Included Into Analyses (n = 1022)
Ethics
Ethical approval was obtained as appropriate to each country, for example, Ethics Commission of the Charité Universitätsmedizin (Reference Number EA2/069/13). All participants gave written informed consent, and if the participant was underage, both the participants and the parents did so. dsd-LIFE was registered in the German Clinical Trials Register (DRKS00006072) and funded by the European Seventh Framework Programme (FP7/2007-2013) under Grant Agreement Number 305373.
Instruments and Measurements
Background Measures
The online self-report questionnaire for participants (patient-reported outcomes) included sociodemographic data (including age, the European Survey version of International Standard Classification of Education as an European standardized education measurement, place of living, and relationship status).
Outcome Measures
Self-reported data on previous and current psychiatric diagnoses were collected, including the following: eating disorder, chronic anxiety, chronic depression, attention problems, hyperactivity, eruptive/aggressive behavior, burnout syndrome, schizophrenia, autism, Asperger syndrome or pervasive developmental disorder, and other mental health problems. In addition, participants answered two questions about suicide attempts, “Have you ever thought about committing suicide?” and “Have you ever tried to committing suicide?” both with the answering options “Yes,” “No,” and “Don’t want to answer this question.”
The following standardized measures were taken to screen for psychiatric conditions:
The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-rating instrument for dimensional and categorical aspects of anxiety and depression (38). The instrument includes two subscales: depression and anxiety. Answers are ticked on a four-point Likert scale (from most of the time to not at all). For each subscale, scores between 0 and 7 indicate normal, between 8 and 10 indicate borderline, and 11 or more pathological levels are indicative of an anxiety or depressive disorder. A pathological result does not establish a clinical diagnosis but an elevated risk for anxiety disorder or depression.
The Adult ADHD Self-Report Scale (ASRS v1.1) was developed by the World Health Organization as a screening instrument for ADHD. The assessment scale is scored on a five-point Likert scale (ranging from “never” to “very often”). One point can be scored for each question: for “sometimes, often or very often” in the first three questions and one point for “often or very often” for the second three. If the individual scores ≥4 of 6, the screening test is considered positive (39). The ASRS screener has a high sensitivity (68.7%) and specificity (99.5%) with a κ value of 0.76 (38). In addition, Kessler and colleagues (40) calculated a sum score ranging from 0 to 24, with a cut point of ≥14 of 24.
The Short Autism Spectrum Quotient (AQ-10) is a brief 10-item screening instrument for autistic spectrum disorders developed from the Autism Spectrum Quotient long version with 50 items (41). Agreement with statements is rated on a four-point Likert scale (from “definitely agree” to “definitely disagree”). Scores higher than 6 of 10 indicate autistic symptoms, and referring to a specialist for diagnostic assessment is recommended. The AQ-10 has a high internal consistency (Cronbach α = 0.85) and predictive value (>.90) (40).
Measures on Moderating Concepts
The following standardized measures were taken to assess psychological characteristics that may impact the outcome measures:
The Customer Satisfaction Questionnaire (CSQ-4) is a self-report four-item questionnaire measuring satisfaction with services in general (42) and asks, for example, “To what extent have the health services you received met your needs?” The verbal anchors of the response choice options differ from item to item but are all based on a four-point Likert scale without a neutral position. A high CSQ-4 score reflects more satisfaction.
The Rosenberg Self-Esteem Scale (RSES) assesses global self-esteem, defined as a person’s overall evaluation of his or her worthiness as a human being (43). The RSES is a 10-question scale, in which individuals rate their agreement with statements, ranging from strongly agree to strongly disagree, with a total score ranging from 0 to 30, in which higher scores indicate more self-esteem.
Body image is not only the way one perceives one’s body but also how one feels about these perceptions. The Body Image Scale (BIS) consists of 30 body features, which an individual is asked to rate on a five-point scale of satisfaction (1 (very satisfied) to 5 (very dissatisfied)). Sex-specific items are scrotum/vagina, penis/clitoris, and testicles/uterus/ovaries (44) (see the study by van de Grift et al. (27) for further information). Lindgren and Pauly (44) classified the following three subscales: primary sex characteristics, secondary sex characteristics, and neutral body characteristics. In the current study, instead of the complete primary sex characteristics, only satisfaction with genitals (penis for men and vagina for women) was used. Reason was too many missing data because participants failed to fill out items, such as breasts (in men) and Adam’s apple (in women). To all study participants, both sex versions were presented, which might have led to confusion and a high rate of missing scores on many BIS items.
Dealing with the DSD condition was measured with the Coping with DSD questionnaire, developed by Kleinemeier and colleagues (29) in adolescents with DSD. Respondents were asked to consider four statements of the Shame/Stigmatization scale and one statement of the Openness scale (“I don’t want to talk to other people about my condition”) on a four-point scale (from completely true to not true at all). Higher scores indicate less shame and (self-)stigmatization and a more open way of coping with DSD.
If one of the previous questionnaires was not available in an official version of one of the dsd-LIFE languages, they were translated according to international quality standards.
Comparison of the Level of Anxiety and Depression to a Reference Population
dsd-LIFE participants were compared with an adult sample of 20,992 employees who filled out the HADS as part of their biennial occupational examination in France in 2011 (45). French norm data were chosen as reference because French participants constituted the largest subsample (n = 311; 26% of participants).
Statistics
The current study followed the same procedure that was developed for all publications within the dsd-LIFE project; for each publication, before any data were provided or analyzed, a proposal including an analysis plan had to be submitted to the dsd-LIFE steering committee, reviewed, and approved.
Continuous data are presented as means and SDs (or median and interquartile range in case of the HADS scores), whereas categorical data are shown as frequencies and percentages. We used analyses of variance or Kruskal–Wallis tests to compare continuous scores across the defined diagnostic groups. Frequencies were compared by χ2 tests. Post hoc pairwise comparisons between diagnostic groups were performed using χ2 tests for categorical parameters and using t tests with pooled SD or Mann–Whitney U tests for continuous variables. The HADS anxiety and depression values of the studied cohort and diagnostic groups were compared with a reference population from France (45) using t tests.
For each diagnostic group, linear regression models were calculated with the HADS anxiety score, the HADS depression score, the AQ-10 score, and the ASRS score as dependent variables, using age, the education level (low, medium, high), the living condition (single, living with parents, living with a partner), the sexual orientation, the RSES score, the CSQ-4 score, openness, shame/stigma score, and the body image (genital, secondary, neutral) as independent variables. The independent variables were selected based on clinical expertise and existing literature before the analysis to investigate the amount of explained variance (R2 and adjusted R2 including bootstrapped 95% confidence intervals using 1000 bootstrap samples) in the dependent variables by the set of independent parameters in each diagnostic group. Furthermore, the relative importance of parameters (i.e., the amount of explained variance accounted for by a certain parameter) was investigated using the approach of Lindeman et al. (46).
The data analysis was performed using the R environment statistics (Version 3.2.2) (47) including the package relaimpo and SAS software, Version 9.4 of the SAS System for Windows (48). A p value of less than .05 was considered significant. Because of the explorative nature of the dsd-LIFE study, no corrections for multiple comparisons were performed and the results are to be considered as exploratory.
RESULTS
General Characteristics
Age, level of education, and relationship status of participants and between-group differences are presented in Table 1.
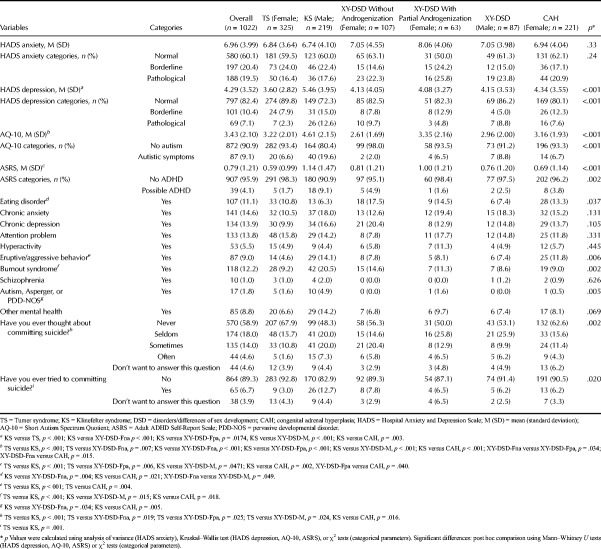
Between-Group Comparisons on Measures of Mental Health
In the sample as a whole, reported (past or current) diagnosis of mental health problems ranged from 1% for schizophrenia to 14.6% for chronic anxiety (Table 2). There were few noticeable differences between the various DSD diagnoses (p < .05), except for eating disorders, eruptive disorders, burnout, and autism spectrum disorders. Post hoc analyses revealed that individuals with KS reported most frequently a lifetime burnout diagnosis compared with individuals with TS or CAH, and autism-spectrum disorders compared with female participants with XY-DSD without androgenization and CAH. Suicidal thoughts were reported less frequently by participants with TS compared with participants with KS, female participants with XY-DSD with partial and without androgenization, and male participants with XY-DSD.
TABLE 2.
Psychiatric Symptoms in DSD, Separated by Diagnosis Groups
On the screening instruments, noticeable differences between the DSD conditions existed (p < .05) regarding depressive, autistic, and ADHD symptoms. Screening measures for anxiety (HADS) indicated a score with elevated risk for clinical range anxiety in approximately one-fifth of the participants, independent from the diagnosis group. The same measure for depression (HADS) revealed an elevated risk for clinical range depression in 7% of participants. Individuals with KS reported more depressive symptoms than did individuals with TS, female participants with XY-DSD without androgenization, male participants with XY-DSD, or female participants with CAH. Screening scores for ADHD with the ASRS were positive in 4% when grouped together, but up to 9% in individuals with KS. Positive screening scores were obtained in approximately 9% for autism (AQ-10), with the highest frequency of positive scores in participants with KS with 19.6% (Table 2).
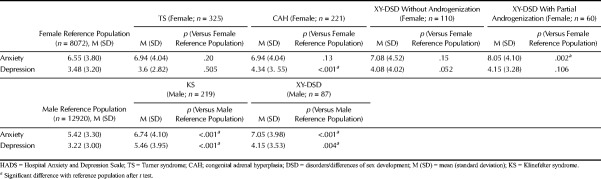
Comparison With Reference Population
Compared with sex-specific reference values, scores for anxiety were significantly higher (p < .05) in female individuals with XY-DSD with partial androgenization and in individuals with KS as well as male individuals with XY-DSD (Table 3). Scores for depression were higher for both male diagnosis groups and female groups with CAH. No such differences were observed for female individuals diagnosed with a XY-DSD condition without androgenization (Table 3).
TABLE 3.
Comparison of the HADS Value Per Overall Sample and Per Diagnosis With a Reference Population in France
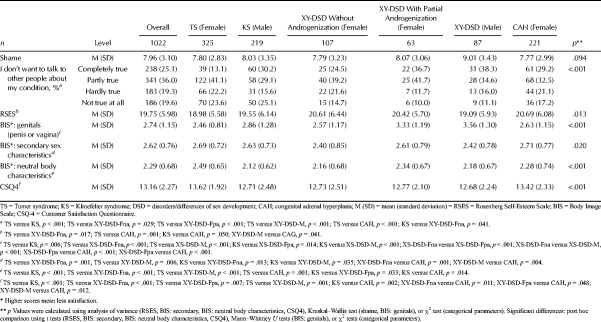
Regression Analyses of Associations With Mental Health
The distribution of the possible factors associated with psychiatric symptoms is shown in Table 4. Post hoc analyses revealed noticeable (p < .05) differences between the DSD conditions in all factors except shame.
TABLE 4.
Distribution of Possible Determinants for Mental Health Problems in Individuals With DSD (n = 1022)
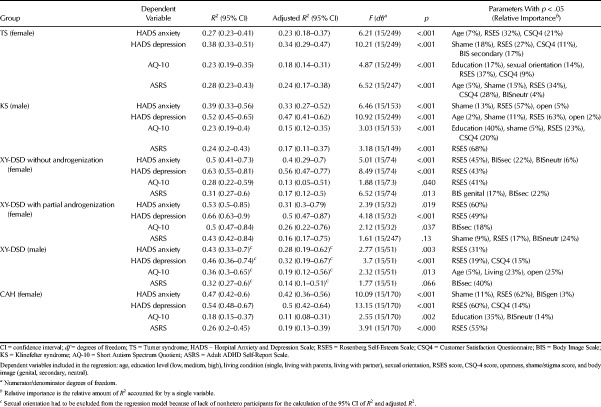
See Table 5 for the summary of the regression models (i.e., explained variance denoted by R2 and adjusted R2 and important factors denoted by relative importance) for depressive and anxiety symptoms (HADS domain scores), autistic features (AQ-10 overall score), and ADHD symptoms (ASRS overall score). Details for each regression are given in the Appendix (Supplemental Digital Content 1, http://links.lww.com/PSYMED/A568).
TABLE 5.
Results of Multiple Linear Regressions Divided by Group and Dependent Variables
For HADS anxiety, the model explained 27% to 53% of the outcome (R2) while also yielding reasonable adjusted R2 values (0.23–0.42). Self-esteem was negatively associated with anxiety (p < .05) in all subgroups. Body satisfaction was negatively associated with anxiety (p < .05) in female individuals with XY-DSD without androgenization and in CAH. Other factors negatively associated (p < .05) in some subgroups were openness (KS) and shame (CAH).
For HADS depression, the model explained 38% to 66% of the variance of outcome (R2) while also yielding the highest adjusted R2 values of all models (0.34–0.56). Self-esteem was negatively associated (p < .05) with depression in all subgroups, and shame was negatively associated (p < .05) in TS and KS. In addition, satisfaction with care was a negatively associated factor (p < .05) with depression in individuals with TS, in male individuals with XY-DSD, and in women with CAH, and body satisfaction was a negatively associated factor (p < .05) with depressive symptoms in women with TS.
For the AQ-10 (autistic symptoms), the model explained 18% to 50% of the variance of outcome (R2), although adjusted R2 values were rather low (<0.30). Self-esteem was negatively associated (p < .05) with autistic symptoms in four of the six subgroups (not in male individuals with XY-DSD and individuals with CAH). Education was negatively associated (p < .05) with autistic symptoms in participants with TS, KS, and CAH. Living alone was associated (p < .05) with autistic symptoms in male individuals with XY-DSD. Satisfaction with care was negatively associated (p < .05) with autistic symptoms in individuals with TS and KS.
For the ASRS (ADHD symptoms), the model explained 24% to 43% of the variance of outcome (R2), whereas the adjusted R2 values were rather low (<0.30). Self-esteem was associated (p < .05) with anxiety in four of the six subgroups (not in female individuals with XY-DSD nonandrogenized and male individuals with XY-DSD). Shame and satisfaction with care were negatively associated (p < .05) with ADHD symptoms in individuals with TS. Body image was negatively associated (p < .05) with ADHD symptoms in participants with TS, in female participants with XY-DSD with and without androgenization, and in male participants with XY-DSD.
DISCUSSION
The findings of this multicenter study on mental health of a very large sample of people with different DSD conditions show that many of them do well. Current self-reported anxiety levels were similar among the subgroups but self-reported depressive symptoms, autistic characteristics, and attention difficulties differed across the various DSD groups. Compared with the general population norms, anxiety and depression levels were higher in both male DSD conditions (KS and XY-DSD male individuals), whereas in female DSD conditions, only female individuals with XY-DSD with partial androgenization had more anxiety and female individuals with CAH had more depressive symptoms.
Compared with the other DSD conditions, women with TS did not have higher levels of autistic, attention difficulties, or anxiety, and depressive symptoms were fewest. Several other studies in adult women with TS show that they cope well in adult life (8,49), although their self-esteem was lowest of all DSD groups. Other studies, one in the same cohort, show that body dissatisfaction is associated with the physical characteristics typical of TS, such as webbed neck and short stature and being overweight (25–27).
Individuals with KS in our study seem to be the most vulnerable group. Not only were their autistic and attention difficulties high compared with the other conditions but also their levels of depression and anxiety. Their self-reported anxiety, depression, ADHD, and autism symptom levels were also higher when compared with the French reference population or population prevalence rates (43,50,51). Another article on the general health status in the same dsd-LIFE cohort already showed that the participants with KS not only reported highest percentages of having physical problems but also reported psychiatric health problems (45%) and a lifetime psychiatric diagnosis (59%) (52). Clearly, the stresses and strains of this most prevalent chromosomal aberration in male participants are high.
In female participants with 46, XX CAH, the present study did not reveal higher rates of psychiatric symptoms compared with the other DSD conditions. Anxiety score did not differ, but the depression score was higher than scores of normative samples (45). Affective distress in CAH might be due to trauma through distressing procedures, stress from chronic illness, and psychosocial consequences of the disorder (13). Autism symptoms suggestive of a clinically relevant problem occurred in 6.7%, which is higher than the adult estimated population rate (1%) (50,51) and in line with the suggested relation with increased prenatal testosterone exposure typical of CAH (32).
Of interest, self-reported symptoms of anxiety, depression, ADHD, and autism did not differ between the female individuals with XY-DSD with or without androgenization, leaving the relation to (prenatal) testosterone exposure inconclusive. Of further interest, only in conditions with an androgen effect (male individuals with XY-DSD, female individuals with XY-DSD with partial androgenization, female individuals with CAH), anxiety and depression scores were higher compared with the norm population. These mixed results may be due to the variability of underlying conditions within the XY-DSD groups (12,15,17) but may also warrant clinicians that within the DSD population, individuals with TS and XY-DSD without androgenization may show some yet unexplained resilience against developing emotional diffculties.
With regard to psychiatric histories, a recently published study of the same cohort showed that psychiatric conditions occurred more often compared with controls (52). The reported 11.1% eating disorder is higher than the lifetime prevalence of 3% in population studies (53). The reported percentages of chronic anxiety (14.6%) and depression (13.9%) are in line with the European population lifetime prevalence rates (54,55), but attention difficulty (13.8%), eruptive disorder (9.0%), and autism/pervasive developmental disorder not otherwise specified (1.8%) were higher than the general population estimates of ADHD (4.2%), conduct disorder (3.0%), and autism spectrum disorder (1%) (50,51,55). In another study in the same cohort on general health status, a history of a psychiatric disorder was partly predicted by age at diagnosis (the older, the more disorders) and healthy life-style (defined as never smoked in combination with sport activities ≥2 h/wk) (52). Of interest, the study on quality of life in the same dsd-LIFE cohort showed that a good perceived general health status was an important predictor of psychological quality of life (56). Thus, in persons with DSD conditions, mental health and physical health are strongly connected.
A worrisome finding was the almost 20% of participants who sometimes or frequently had suicidal thoughts and the almost 7% of participants who had ever tried to commit suicide (see the study by Falhammar et al. (52)). This is also higher than the reported lifetime prevalence of suicidal ideation of 9.2% and of the suicide attempts of 2.7% in the World Mental Health Survey general population study (57). Although the finding should be interpreted carefully because of the retrospective nature and the unspecified character of the questions (questions such as “How intrusive were the thoughts?” “How often is frequent?” “How serious was the act?” were not included), and considering the absence of a control group, this finding is in line with other studies showing even higher suicidality rates in individuals with XY-DSD and XX-DSD (12,13).
Because the dsd-LIFE project aimed at improving quality of life and care for people with DSD, we tried to identify possible factors associated with mental health. Shame and stigma around XY-DSD and XX-DSD conditions have been found by some to negatively influence well-being (29,30). In line with these studies, we found much discomfort and a reluctance to talk about the diagnosis to other people (55%–70%). This shows that having a DSD diagnosis that may influence appearance, sex role, fertility, and sexuality often is still perceived as a taboo that is better kept to oneself. Particularly in persons with the chromosomal DSD conditions TS and KS, shame was significantly associated with depressive symptoms, showing the relevance of addressing shame in clinical care. Clinicians in multidisciplinary DSD teams should therefore not only give medical advice but also support the care seekers to find a satisfying coping style with the condition. Through open and proactive communication, affected individuals may gain a sense of control and become empowered with regard to their conditions. For that reason, it is important that mental health providers are part of the DSD team. Another form of support can take place through peer counseling, which connects care seekers with persons with similar conditions and their families. Another factor associated with emotional (anxiety and depression) as well as behavioral (autistic and attention) symptoms in almost all DSD conditions was self-esteem. Helping the individual with DSD develop a healthy self-esteem and thereby build resilience against emotional and behavioral difficulties is an aspect of care that deserves much more specific attention in DSD care than clinicians may realize (58). Furthermore, satisfaction with care was significantly correlated with mental health in some of the groups, confirming earlier findings in a sample with various XY-DSD and XX-DSD conditions (including CAH but no KS and TS, see the study by Thyen et al. (28)). Although we do not know the direction of the causality, the experience of having received good care, being equipped with knowledge, and having consented to interventions may have laid the base for a favorable mental health. It is of note to mention that satisfaction with care is also related to how care for rare diseases is organized within a specific country or center, as another study on the same cohort has shown (59). More specialized centers received more satisfaction from the respondents. Of note, body image (genital dissatisfaction, sex characteristic dissatisfaction, and sex neutral body characteristics) was, though to a smaller extent, also related to psychological well-being in individuals with TS and in male individuals with XY-DSD. This may be associated with the variance in physical characteristics of certain DSD conditions, infertility, or ambiguous genitalia that were operated on (24,25,27,60). Finally, educational level was correlated with autistic symptoms in participants with TS, KS, and CAH. Indeed, individuals with TS and KS can have specific learning difficulties that deserve special attention to promote their psychological well-being (35,61).
Of interest, significant differences existed between the various DSD conditions on factors that were tested to be related to mental health status such as educational level, shame and stigma, self-esteem, body image, and satisfaction with care and relationship status. For example, individuals with XY-DSD had the highest educational level, persons with KS were most often in a relationship, whereas people with TS experienced the fewest shame and stigma. Because of the descriptive explorative character of the present study, further analyses were not performed, but these findings deserve future studies.
The study had several limitations. There were significant numbers of missing values on some of the items of the survey. For example, on the BIS, satisfaction with certain sexual sex characteristics was often not filled out. Another limitation is that, although the present study included large numbers of participants, the respective numbers of the more rare XY-DSD conditions were still too small to allow for condition-specific analyses. Registry studies might be a way to include larger numbers specifically of these more rare conditions. A final limitation is that it should be realized that this study only used retrospective psychiatric history data and psychiatric symptom screening measures, and no validated diagnostic instruments, so that the reported prevalence rates should be interpreted carefully.
Clinical Implications
The current study demonstrates that individuals with a wide diversity of DSD conditions can experience similar mental health issues. Emotional difficulties were expected in all conditions because having a chronic condition can be stressful in general. More unexpectedly, neurodevelopmental difficulties did occur also in the nonchromosomal DSD conditions, a finding that is important for clinicians in DSD care. They should also be aware of the relevance of shame, self-esteem, body image, and satisfaction with care for mental health in people with DSD conditions. Individuals among the different DSD conditions shared that they easily have feelings of shame. Developing a healthy self-esteem and positive body image can be challenging. Although DSD conditions cannot be cured, building resilience and coping with the previous issues will substantially improve the mental health of persons with DSD.
Supplementary Material
Acknowledgments
The dsd-LIFE Group are as follows: Birgit Kohler, Berlin; Peggy Cohen-Kettenis and Annelou de Vries, Amsterdam; Wiebke Arlt, Birmingham; Claudia Wiesemann, Gottingen; Jolanta Slowikowska-Hilczer, Lodz; Aude Brac de la Perriere, Lyon; Charles Sultan and Francoise Paris, Montpellier; Claire Bouvattier, Paris; Ute Thyen, Lubeck; Nicole Reisch, Munich; Annette Richter-Unruh, Munster; Hedi Claahsen-van der Grinten, Nijmegen; Anna Nordenstrom, Stockholm; Catherine Pienkowski, Toulouse; and Maria Szarras-Czapnik, Warsaw.
We thank the persons who participated in dsd-LIFE and to all staff at the recruiting centers. We also thank the support groups in the different countries that have supported the study.
Source of Funding and Conflicts of Interest: This study was funded by the European Union Seventh Framework Program (Grant 305373 [FP7/2007-2013], to all authors). The authors report no conflicts of interest.
Footnotes
Supplemental Content
Birgit Köhler is deceased.
Contributor Information
Collaborators: on behalf of the dsd-LIFE Group
REFERENCES
- 1.Lee PA, Houk CP, Ahmed SF, Hughes IA. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. Pediatrics 2006;118:e488–500. [DOI] [PubMed] [Google Scholar]
- 2.Meyer-Bahlburg HF. Intersex care development: current priorities. LGBT Health 2017;4:77–80. [DOI] [PubMed] [Google Scholar]
- 3.Lee PA, Nordenström A, Houk CP, Ahmed SF, Auchus R, Baratz A, Baratz Dalke K, Liao LM, Lin-Su K, Looijenga LH, 3rd, Mazur T, Meyer-Bahlburg HF, Mouriquand P, Quigley CA, Sandberg DE, Vilain E, Witchel S, Global DSDUC. Global disorders of sex development update since 2006: perceptions, approach and care. Horm Res Paediatr 2016;85:158–80. [DOI] [PubMed] [Google Scholar]
- 4.Kreukels BPC, Kohler B, Nordenstrom A, Roehle R, Thyen U, Bouvattier C, de Vries ALC, Cohen-Kettenis PT, dsd Lg. Gender dysphoria and gender change in disorders of sex development/intersex conditions: results from the dsd-LIFE study. J Sex Med 2018;15:777–85. [DOI] [PubMed] [Google Scholar]
- 5.Russell HF, Wallis D, Mazzocco MM, Moshang T, Zackai E, Zinn AR, Ross JL, Muenke M. Increased prevalence of ADHD in Turner syndrome with no evidence of imprinting effects. J Pediatr Psychol 2006;31:945–55. [DOI] [PubMed] [Google Scholar]
- 6.Creswell CS, Skuse DH. Autism in association with Turner syndrome: genetic implications for male vulnerability to pervasive developmental disorders. Neurocase 1999;5:511–8. [Google Scholar]
- 7.Schmidt PJ, Cardoso GM, Ross JL, Haq N, Rubinow DR, Bondy CA. Shyness, social anxiety, and impaired self-esteem in Turner syndrome and premature ovarian failure. JAMA 2006;295:1374–6. [DOI] [PubMed] [Google Scholar]
- 8.Naess EE, Bahr D, Gravholt CH. Health status in women with Turner syndrome: a questionnaire study on health status, education, work participation and aspects of sexual functioning. Clin Endocrinol (Oxf) 2010;72:678–84. [DOI] [PubMed] [Google Scholar]
- 9.Bojesen A, Juul S, Birkebaek NH, Gravholt CH. Morbidity in Klinefelter syndrome: a Danish register study based on hospital discharge diagnoses. J Clin Endocrinol Metab 2006;91:1254–60. [DOI] [PubMed] [Google Scholar]
- 10.Bruining H, Swaab H, Kas M, van Engeland H. Psychiatric characteristics in a self-selected sample of boys with Klinefelter syndrome. Pediatrics 2009;123:e865–70. [DOI] [PubMed] [Google Scholar]
- 11.Cederlof M, Ohlsson Gotby A, Larsson H, Serlachius E, Boman M, Langstrom N, Landen M, Lichtenstein P. Klinefelter syndrome and risk of psychosis, autism and ADHD. J Psychiatr Res 2014;48:128–30. [DOI] [PubMed] [Google Scholar]
- 12.Schutzmann K, Brinkmann L, Schacht M, Richter-Appelt H. Psychological distress, self-harming behavior, and suicidal tendencies in adults with disorders of sex development. Arch Sex Behav 2009;38:16–33. [DOI] [PubMed] [Google Scholar]
- 13.Johannsen TH, Ripa CP, Mortensen EL, Main KM. Quality of life in 70 women with disorders of sex development. Eur J Endocrinol 2006;155:877–85. [DOI] [PubMed] [Google Scholar]
- 14.Bennecke E, Thyen U, Gruters A, Lux A, Kohler B. Health-related quality of life and psychological well-being in adults with differences/disorders of sex development. Clin Endocrinol (Oxf) 2017;86:634–43. [DOI] [PubMed] [Google Scholar]
- 15.Schweizer K, Brunner F, Gedrose B, Handford C, Richter-Appelt H. Coping with diverse sex development: treatment experiences and psychosocial support during childhood and adolescence and adult well-being. J Pediatr Psychol 2017;42:504–19. [DOI] [PubMed] [Google Scholar]
- 16.D’Alberton F, Assante MT, Foresti M, Balsamo A, Bertelloni S, Dati E, Nardi L, Bacchi ML, Mazzanti L. Quality of life and psychological adjustment of women living with 46,XY differences of sex development. J Sex Med 2015;12:1440–9. [DOI] [PubMed] [Google Scholar]
- 17.de Neve-Enthoven NG, Callens N, van Kuyk M, van Kuppenveld JH, Drop SL, Cohen-Kettenis PT, Dessens AB. Psychosocial well-being in Dutch adults with disorders of sex development. J Psychosom Res 2016;83:57–64. [DOI] [PubMed] [Google Scholar]
- 18.Ediati A, Faradz SM, Juniarto AZ, van der Ende J, Drop SL, Dessens AB. Emotional and behavioral problems in late-identified Indonesian patients with disorders of sex development. J Psychosom Res 2015;79:76–84. [DOI] [PubMed] [Google Scholar]
- 19.Engberg H, Butwicka A, Nordenstrom A, Hirschberg AL, Falhammar H, Lichtenstein P, Nordenskjold A, Frisen L, Landen M. Congenital adrenal hyperplasia and risk for psychiatric disorders in girls and women born between 1915 and 2010: a total population study. Psychoneuroendocrinology 2015;60:195–205. [DOI] [PubMed] [Google Scholar]
- 20.Mueller SC, Ng P, Sinaii N, Leschek EW, Green-Golan L, VanRyzin C, Ernst M, Merke DP. Psychiatric characterization of children with genetic causes of hyperandrogenism. Eur J Endocrinol 2010;163:801–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jenkins-Jones S, Whitaker MJ, Holden SE, Morgan CL, Ross RJ, Currie CJ. The burden of illness of congenital adrenal hyperplasia in the United Kingdom: a retrospective, observational study. Value Health 2015;18:A749. [Google Scholar]
- 22.Kung KT, Spencer D, Pasterski V, Neufeld S, Glover V, O’Connor TG, Hindmarsh PC, Hughes IA, Acerini CL, Hines M. No relationship between prenatal androgen exposure and autistic traits: convergent evidence from studies of children with congenital adrenal hyperplasia and of amniotic testosterone concentrations in typically developing children. J Child Psychol Psychiatry 2016;57:1455–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reisch N, Hahner S, Bleicken B, Flade L, Pedrosa Gil F, Loeffler M, Ventz M, Hinz A, Beuschlein F, Allolio B, Reincke M, Quinkler M. Quality of life is less impaired in adults with congenital adrenal hyperplasia because of 21-hydroxylase deficiency than in patients with primary adrenal insufficiency. Clin Endocrinol (Oxf) 2011;74:166–73. [DOI] [PubMed] [Google Scholar]
- 24.Herlihy AS, McLachlan RI, Gillam L, Cock ML, Collins V, Halliday JL. The psychosocial impact of Klinefelter syndrome and factors influencing quality of life. Genet Med 2011;13:632–42. [DOI] [PubMed] [Google Scholar]
- 25.Cragg SJ, Lafreniere KD. Effects of Turner syndrome on women’s self-esteem and body image. J Dev Phys Disabil 2010;22:433–45. [Google Scholar]
- 26.Lagrou K, Froidecoeur C, Verlinde F, Craen M, De Schepper J, François I, Massa G, Belgian Study Group of Paediatric E. Psychosocial functioning, self-perception and body image and their auxologic correlates in growth hormone and oestrogen-treated young adult women with Turner syndrome. Horm Res 2006;66:277–84. [DOI] [PubMed] [Google Scholar]
- 27.van de Grift TC, Cohen-Kettenis PT, de Vries ALC, Kreukels BPC. Body image and self-esteem in disorders of sex development: a European multicenter study. Health Psychol 2018;37:334–43. [DOI] [PubMed] [Google Scholar]
- 28.Thyen U, Lux A, Jürgensen M, Hiort O, Köhler B. Utilization of health care services and satisfaction with care in adults affected by disorders of sex development (DSD). J Gen Intern Med 2014;29(Suppl 3):S752–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kleinemeier E, Jürgensen M, Lux A, Widenka PM, Thyen U, Disorders of Sex Development Network Working G. Psychological adjustment and sexual development of adolescents with disorders of sex development. J Adolesc Health 2010;47:463–71. [DOI] [PubMed] [Google Scholar]
- 30.Meyer-Bahlburg HF, Reyes-Portillo JA, Khuri J, Ehrhardt AA, New MI. Syndrome-related stigma in the general social environment as reported by women with classical congenital adrenal hyperplasia. Arch Sex Behav 2017;46:341–51. [DOI] [PubMed] [Google Scholar]
- 31.Ploderl M, Tremblay P. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry 2015;27:367–85. [DOI] [PubMed] [Google Scholar]
- 32.Knickmeyer R, Baron-Cohen S, Fane BA, Wheelwright S, Mathews GA, Conway GS, Brook CG, Hines M. Androgens and autistic traits: a study of individuals with congenital adrenal hyperplasia. Horm Behav 2006;50:148–53. [DOI] [PubMed] [Google Scholar]
- 33.van Rijn S, Swaab H. Vulnerability for psychopathology in Klinefelter syndrome: age-specific and cognitive-specific risk profiles. Acta Paediatr 2011;100:908–16. [DOI] [PubMed] [Google Scholar]
- 34.van Rijn S, Swaab H. Executive dysfunction and the relation with behavioral problems in children with 47,XXY and 47,XXX. Genes Brain Behav 2015;14:200–8. [DOI] [PubMed] [Google Scholar]
- 35.Hong D, Scaletta Kent J, Kesler S. Cognitive profile of Turner syndrome. Dev Disabil Res Rev 2009;15:270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Knickmeyer RC, Davenport M. Turner syndrome and sexual differentiation of the brain: implications for understanding male-biased neurodevelopmental disorders. J Neurodev Disord 2011;3:293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Röhle R, Gehrmann K, Szarras-Czapnik M, Claahsen-van der Grinten H, Pienkowski C, Bouvattier C, Cohen-Kettenis P, Nordenström A, Thyen U, Köhler B, dsd-LIFE group. Participation of adults with disorders/differences of sex development (DSD) in the clinical study dsd-LIFE: design, methodology, recruitment, data quality and study population. BMC Endocr Disord 2017;17:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 39.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med 2005;35:245–56. [DOI] [PubMed] [Google Scholar]
- 40.Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int J Methods Psychiatr Res 2007;16:52–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allison C, Auyeung B, Baron-Cohen S. Toward brief “Red Flags” for autism screening: The Short Autism Spectrum Quotient and the Short Quantitative Checklist for Autism in toddlers in 1,000 cases and 3,000 controls [corrected]. J Am Acad Child Adolesc Psychiatry 2012;51:202–12 e7. [DOI] [PubMed] [Google Scholar]
- 42.Attkisson CC. The CSQ Scales Reprint Portfolio. Mill Valley, CA: Tamalpais Matrix Systems, LLC; CD-R available for purchase on this web site. Available at: http://www.csqscales.com/%5D.2012. Accessed July 18, 2019. [Google Scholar]
- 43.Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 44.Lindgren TW, Pauly IB. A body image scale for evaluating transsexuals. Arch Sex Behav 1975;4:639–56. [DOI] [PubMed] [Google Scholar]
- 45.Bocéréan C, Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry 2014;14:354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindeman RH, Merenda PF, Gold RZ. Introduction to Bivariate and Multivariate Analysis. Glenview IL: Scott, Foresman and Comp; 1980. [Google Scholar]
- 47.Team RC. R: A Language and Environment for Statistical Computing. Vienna, Austria; 2014. [Google Scholar]
- 48.Grömping U. Relative importance for linear regression in R: the package relaimpo. J Stat Softw 2006;17:1–27. [Google Scholar]
- 49.Lepage JF, Lortie M, Deal CL, Théoret H. Empathy, autistic traits, and motor resonance in adults with Turner syndrome. Soc Neurosci 2014;9:601–9. [DOI] [PubMed] [Google Scholar]
- 50.Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, Bebbington P, Jenkins R, Meltzer H. Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry 2011;68:459–65. [DOI] [PubMed] [Google Scholar]
- 51.Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, De Girolamo G, Haro JM, Karam EG, Lara C, Lepine JP, Ormel J, Posada-Villa J, Zaslavsky AM, Jin R. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 2007;190:402–9. [DOI] [PubMed] [Google Scholar]
- 52.Falhammar H, Claahsen-van der Grinten H, Reisch N, Slowikowska-Hilczer J, Nordenstrom A, Roehle R, Bouvattier C, Kreukels BPC, Kohler B, dsd Lg. Health status in 1040 adults with disorders of sex development (DSD): a European multicenter study. Endocr Connect 2018;7:466–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med 1998;28:109–26. [DOI] [PubMed] [Google Scholar]
- 54.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lépine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martínez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacín C, Romera B, Taub N, Vollebergh WA, EsemeD/Mhedea Investigators ESotEoMDP. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004;:21–7. [DOI] [PubMed] [Google Scholar]
- 55.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, Steinhausen HC. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011;21:655–79. [DOI] [PubMed] [Google Scholar]
- 56.Rapp M, Mueller-Godeffroy E, Lee P, Roehle R, Kreukels BPC, Köhler B, Nordenström A, Bouvattier C, Thyen U, dsd Lg. Multicentre cross-sectional clinical evaluation study about quality of life in adults with disorders/differences of sex development (DSD) compared to country specific reference populations (dsd-LIFE). Health Qual Life Outcomes 2018;16:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, de Graaf R, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, Ono Y, Posada-Villa J, Williams D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 2008;192:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson J, Panagioti M, Bass J, Ramsey L, Harrison R. Resilience to emotional distress in response to failure, error or mistakes: a systematic review. Clin Psychol Rev 2017;52:19–42. [DOI] [PubMed] [Google Scholar]
- 59.Thyen U, Ittermann T, Flessa S, Muehlan H, Birnbaum W, Rapp M, Marshall L, Szarras-Capnik M, Bouvattier C, Kreukels BPC, Nordenstroem A, Roehle R, Koehler B, dsd Lg. Quality of health care in adolescents and adults with disorders/differences of sex development (DSD) in six European countries (dsd-LIFE). BMC Health Serv Res 2018;18:527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Migeon CJ, Wisniewski AB, Gearhart JP, Meyer-Bahlburg HF, Rock JA, Brown TR, Casella SJ, Maret A, Ngai KM, Money J, Berkovitz GD. Ambiguous genitalia with perineoscrotal hypospadias in 46,XY individuals: long-term medical, surgical, and psychosexual outcome. Pediatrics 2002;110:e31. [DOI] [PubMed] [Google Scholar]
- 61.Boada R, Janusz J, Hutaff-Lee C, Tartaglia N. The cognitive phenotype in Klinefelter syndrome: a review of the literature including genetic and hormonal factors. Dev Disabil Res Rev 2009;15:284–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.