Abstract
Multiple primary tumors may develop in patients with head and neck squamous cell carcinoma. The coincidence of head and neck squamous cell carcinoma with papillary thyroid carcinoma is a rare finding. This study reports a case of papillary thyroid carcinoma, which was incidentally detected during the microscopic examination of lymph nodes of a patient diagnosed as gingival squamous cell carcinoma. A review of literature is also presented.
Keywords: Squamous cell carcinoma , Thyroid carcinoma , Gingiva , Lymph node , Metastasis
Introduction
Squamous cell carcinoma (SCC) accounts for 90% of oral cancers. Carcinomas of this region has tendency to metastasize to cervical lymph nodes in the early stages. Therefore, evaluation of lymph nodes can improve the survival rate of patients with oral SCC (OSCC)[1].
Because of the exposure to similar carcinogens, the coexistence of multiple primary tumors is established in patients with head and neck SCC[2]. As reported by Jones et al.[3], the most common regions for such phenomenon are mouth, followed by larynx and oropharynx. It is reported that 7% of such lesions develop synchronously and 25% will develop metachronously4. The differentiated thyroid carcinoma, as a second primary tumor, is rarely detected incidentally in the thyroid gland or in the cervical lymph nodes from patients with head and neck SCC[4]. Up to now, almost 49 cases of simultaneous head and neck SCC and papillary thyroid carcinoma (PTC) have been reported in the literature. Some authors believe that these lesions are unusual migration of benign tissues during embryogenesis[5]. Meanwhile, other researchers consider the presence of follicular structure with normal appearance as a benign structure, whereas, papillary transformation reflects malignancy[6]. However, Pitman et al.[4] claimed the malignant transformation of such tissues to be unusual. Ashraf et al.[7] announced that several metastatic lymph nodes, psammoma bodies, and 30% (or more) involvement of the structure of each lymph node are all indicative of metastatic PTC[7].
In the present study, we define a new case of PTC in a patient with OSCC. A review of literature focusing on the carcinomas of the oral cavity will also be presented.
Case Report
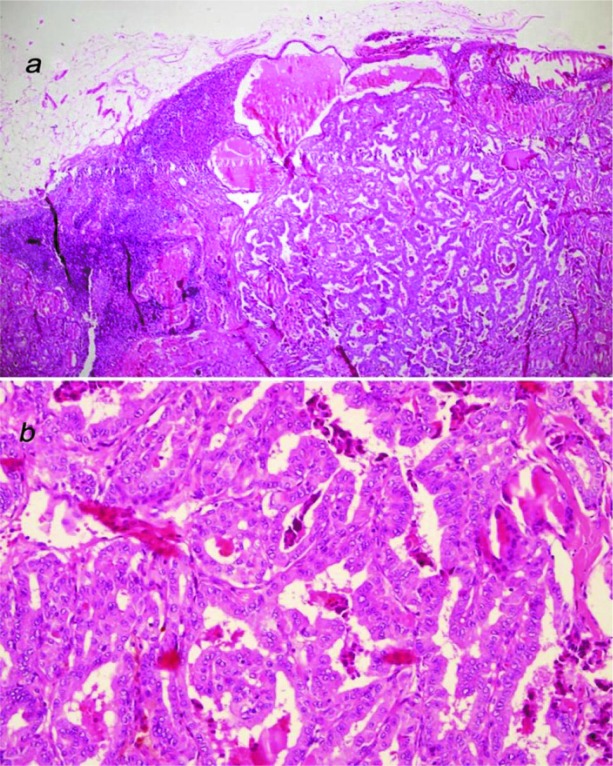
A 65-year-old female referred to a private dental clinic with the history of a painless, non-healing ulcer on the buccal gingiva of anterior area of the mandible extending from right canine to first premolar for about 7 months. She had negative history of smoking or alcohol consumption. No palpable lymph node was found in the neck examination. In addition, computed tomography (CT) with contrast revealed no lymph node, neck, chest, and abdominal involvement by the tumor. No lesion was noted in CBCT study of the head and neck. Incisional biopsy of the lesion showed a well- differentiated SCC. The tumor clinically was assessed as stage II. After preoperative assessment, the patient was subjected to radical excision with safe margins and right side selective neck dissection at the level II and III for prophylactic reasons. The histopathologic examination of frozen sections confirmed the presence of free margins. In the gross examination, there was a tumoral lesion with white color and cauliflower surface in the area of right mandibular canine and the first premolar tooth. The tumor size was 2.5cm in its greater diameter. Post-operative histopathologic examination showed a low-grade SCC composed of nests of neoplastic squamous cells with mild atypia and keratin pearl formation (Figure 1).
Figure1.
Well-differentiated squamous cell carcinoma with nests of malignant squamous cells and keratin pearl formation (a: H&E ×40, b: H&E ×100)
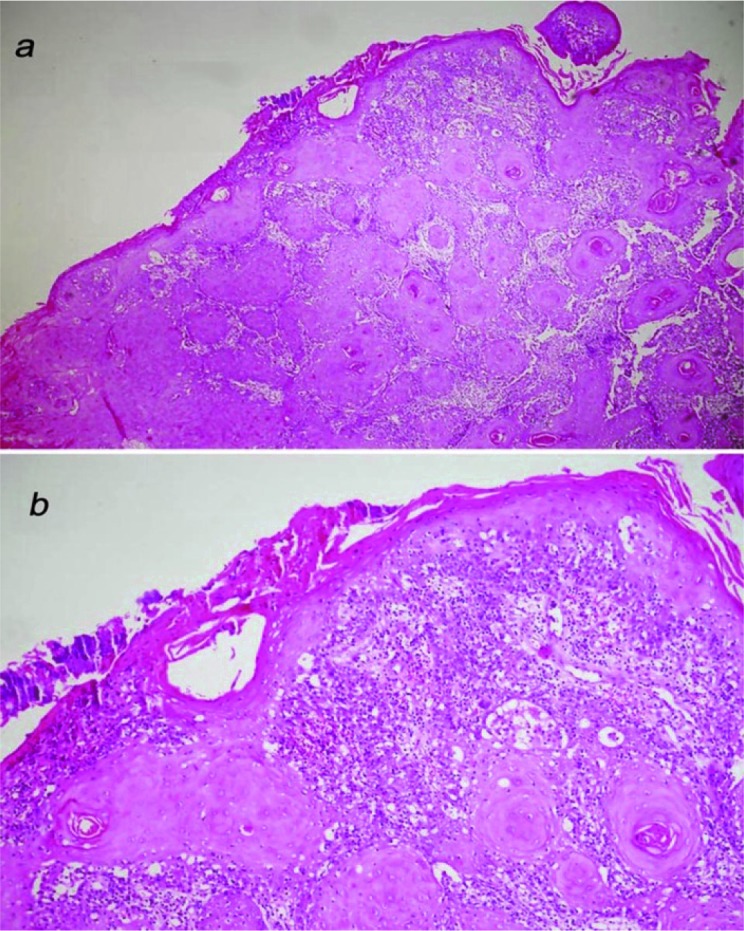
Surgical margins were tumor-free. Two out of the three resected lymph nodes demonstrated papillary and follicular structures lined by cuboidal cells with intranuclear groove and pseudo- intranuclear inclusion suggestive of metastatic PTC. The lymph nodes were not involved by SCC (Figure 2). Laboratory tests and ultrasound-guided fine needle aspiration confirmed the diagnosis of PTC. Subsequently, total thyroidectomy was performed and patient underwent postoperative radionuclide (I131) therapy. In addition, the patient received post-operative radiotherapy for oral tumor. After 18 months of follow-up, the patient was free of tumors.
Figure2.
Metastatic cervical lymph node with papillary structures (a: H&E ×40, b: H&E ×200)
Discussion
Thyroid carcinoma is responsible for 1.5% of adult cancers, and is more prevalent among females[8]. The most common subtype of thyroid carcinomas are PTC, followed by follicular, medullary, and anaplastic subtypes. PTC accounts for 85% of thyroid cancers, which are induced by head and neck radiation[8]. Several studies have revealed a correlation between PTC and iodine deficiency. PTC frequently metastasizes to cervical lymph nodes[8].
In the present report, PTC was found incidentally in a 65-year-old female with a low- grade gingival SCC (stage II) with negative history of smoking. Up to now, of all published cases of thyroid carcinoma coexistent with head and neck SCC, 31 cases with age range of 17 to 76 years (mean age = 58 years) were reported in patients with OSCC, out of which 18 cases were diagnosed as papillary subtype (Table 1).
Table 1.
Summary of studies about thyroid carcinoma in patients with head and neck squamous cell carcinoma
| Author | Cases with head and neck SCC | Thyroid carcinoma | Gender | Mean age | Location of SCC | |
|---|---|---|---|---|---|---|
| NO | Type | |||||
| Clark et al.[6] | 16 | 5 | Fo | M | 63 | Mouth floor=1, Lip=1 Pharynx=1, Larynx=2 |
| 9 | P+Fo | F=1,M=8 | Mouth floor=1, Buccal mucosa=1, Tongue=1,Larynx=6 | |||
| 2 | S | F=1,M=1 | Lip=1, P.sinus=1 | |||
| Vassilopoulou-Sellin et al.[14] | 2855 | 4 | F | F=2,M=2 | 47 | Tongue |
| 4 | P | F=2,M=2 | ||||
| Pitman et al.[4] | _ | 1 | P | M | 50 | Larynx |
| Lopez-Escamez et al.[11] | _ | 1 | P | M | 76 | Larynx |
| Fliegelman et al.[12] | 5 | 4 | P | F=1,M=3 | 58 | Tongue=1, Alveolar ridge=1 |
| Ansari-Lari et al.[5] | 14 | 10 | P | F=2,M=8 | 53 | Head and Neck |
| Resta et al.[15] | 1500 | 8 | P | M | 58 | Larynx, P. sinus=7, Tongue=1 |
| Sheahan et al.[16] | 202 | 1 | P | F | 58 | Maxilla |
| Leon et al.[10] | 11 | 5 | P | M | 59 | Tongue=1, Glottis, P.sinus=4 |
| Altumbabić et al.[18] | - | 1 | P | M | 58 | Palatine, Tonsil, Soft palate, Hypopharynx |
| Ashraf et al.[7] | 250 | 3 | P | M | 66 | Larynx |
| Bishen et al.[8] | - | 1 | P | M | 17 | Mandibular gingiva |
| Kim et al.[2] | - | 1 | P | M | 72 | Mandibular gingiva |
| Verma et al.[9] | - | 1 | P | M | 65 | Mandibular gingiva |
| Perie et al.[13] | 266 | 8 | Fo | F=1,M=7 | 54 | Supraglottis=2, Mouth floor =1 P.sinus=1,Oral cavity=3 Tongue=1 |
| 13 | P | M | Supraglottis=4, Mouth floor=1 P. sinus=3, Oral cavity=1 Glottis=4 | |||
| Present study | - | 1 | P | F | 65 | Mandibular gingiva |
| TOTAL | - | 9 | Fo | F=2,M=7 | 58 | Oral cavity= 31, Pharynx=1 |
| 49 | P | F=8,M=43 | Larynx=39 | |||
| 2 | S | F=1, M=1 | Head and neck=10 | |||
Fo: follicular type; P: papillary type; S: solid type; M: male; F: female, P.sinus: Piriform sinus
Coexistence of metastatic PTC with SCC of gingival was found in three patients in separate studies and unlike our case, they had positive history of smoking and Gutka chewing[2,8-9]. Some researchers reported the cases generally as head and neck SCC without determining the details of location[5]. However, other studies reported more accurately the coincidence of PTC to be more frequently in SCC of the tongue (n=8), followed by gingiva (n=4) and floor of the mouth (n=2) (Table 1).
Metastatic PTC as an incidental finding during neck dissection, is unusual and its incidence estimated to be less than 0.5% by some researchers[4]. Cervical metastases occur in 50% of all small tumors and 75% of larger ones. Thus, a wide sampling and precise study of all specimens must be performed for ultimate diagnosis[8]. Regardless of histological specifications of thyroid tissue inclusions, the prognosis is good, 10-year survival rate is more than 90%, and metastasis does not affect its outcome, though literature shows high risks in elderly patients[2,10].
In Clark et al.’s study[6], thyroid cancer was discovered incidentally during treatment of 16 out of 1516 patients for an unrelated head and neck cancer, including three cases with oral and six cases with laryngeal SCC. In two patients with metastatic lymph nodes, no evidence of thyroid carcinoma was found in thyroid tissue. They elucidated that thyroid carcinomas with 2-3 mm diameter would not be detectable through any procedure, unless the subserial sectioning of the gland was performed[6]. Nonetheless, in Lopez-Escamez et al.’s study[11], serial sectioning of thyroid gland did not reveal any neoplasm.
Earlier studies shows that up to 3% of patients with head and neck cancer may also carry hidden metastatic papillary or follicular thyroid carcinoma[12]. Perie et al. re-evaluated the lymph nodes of patients who undergone neck dissection for their head and neck cancer and found 7.5 % patients with simultaneous head and neck SCC and thyroid carcinoma. They reported that seven of these patients had tongue and oral cavity SCC[13] In Vassilopulou-Sellin et al.’s research, the incidence of PTC metastasis was reported 0.3% in resected head and neck lymph nodes[14]. In their 5- year observation, they found that the cause of death in 50% of patients was the primary SCC of tongue rather than PTC. Therefore, they stated that in the absence of any clinical abnormality in thyroid gland, PTC would not require invasive treatment, though a careful follow-up is crucial[14].
Leon et al.[10] investigated the PTC coexistent with SCC of tongue, glottis, supraglottis, and piriform sinus in five men with age range of 48 to 69 years and reported an incidence of 1.5%. Moreover, Resta et al.[15] detected metastatic PTC in SCC of tongue, larynx, and pyriform sinus.
Sheahan et al.[16] found metastatic PTC in one patient with SCC of maxilla and thyroid follicle in three other patients among 10 cases with head and neck SCC. Interestingly, concurrency of chronic lymphocytic leukemia and non-Hodgkin’s lymphoma with primary SCC was detected in neck lymph nodes from some of the remaining patients[16].
Ansari-Lari et al.[5]reported metastatic PTC in six cases of head and neck SCC and four cases of basal cell carcinoma, melanoma, medullary thyroid carcinoma, and hyperparathyroidism. Additionally, they conveyed B-cell lymphoma as incidental findings in the lymph nodes of six patients with head and neck SCC[5]. Fliegelman et al.[17] reported PTC coinciding with mucoepidermoid carcinoma of tongue and arteriovenous malformation of cheek. Moreover, simultaneous PTC in patients with SCC of palatine tonsil, soft palate, and hypopharyx and larynx was also reported[18]. Ashraf et al.[7] found this coexistence in three patients of laryngeal SCC and recommended a preoperative, image-guided needle biopsy of any uncertain thyroidal gland lesion in cases that undergo laryngectomy.
Since the lateral neck lymph nodes are usually removed during surgical treatment of oral SCC and the most common site of drainage in the PTC is central cervical lymph nodes; therefore, the actual incidence can be expected to be more than what reports say[15].
Our patient was treated with total thyroidectomy and radionuclide therapy. Fliegelman et al.[17] suggested a total thyroidectomy in cases with metastatic lymph nodes when the prognosis of primary carcinoma is good. However, surgery should be avoided in primary carcinomas with poor prognosis. Furthermore, radiotherapy may be employed when the solid tumor is un-resectable or there is likelihood for recurrence after resection[8]. In case of association of PTC and head and neck SCC, the survival rate depends on the stage of SCC[4].
Conclusion
The present study reported a simultaneous PTC and gingival SCC in a female patient. Based on the reviewed literature, this is a rare phenomenon, which is more prevalent in males and elderly patients. PTC is not an invasive malignancy and requires different treatments regarding patient’s condition; hence, the prognosis of the disease depends on the prognosis of primary SCC.
Acknowledgement
The authors are grateful to vice- chancellery for research of school of dentistry, Shiraz University of Medical Sciences.
Conflict of Interest:The authors disclose no potential conflicts of interest.
References
- 1.Kapoor C, Vaidya S, Wadhwan V, Malik S. Lymph node metastasis: A bearing on prognosis in squamous cell carcinoma. Indian J Cancer. 2015; 52: 417–424. doi: 10.4103/0019-509X.176750. [DOI] [PubMed] [Google Scholar]
- 2.Kim JW, Lee CY, Oh SM, Yang BE, Kim JY, Song YJ, et al. Gingival Squamous Carcinoma with Metastatic Lymph Node Involvement of Papillary Thyroid Carcinoma. J Korean Assoc Maxillofac Plast Reconstr Surg. 2012; 34: 276–279. [Google Scholar]
- 3.Jones AS, Morar P, Phillips DE, Field JK, Husband D, Helliwell TR. Second primary tumors in patients with head and necksquamous cell carcinoma. Cancer. 1995; 75: 1343–1353. doi: 10.1002/1097-0142(19950315)75:6<1343::aid-cncr2820750617>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 4.Pitman KT, Johnson JT, Myers EN. Papillary thyroid carcinoma associated with squamous cell carcinoma of the head and neck: significance and treatment. Am J Otolaryngol. 1996; 17: 190–196. doi: 10.1016/s0196-0709(96)90059-9. [DOI] [PubMed] [Google Scholar]
- 5.Ansari-Lari MA, Westra WH. The prevalence and significance of clinically unsuspectedneoplasms in cervical lymph nodes. Head Neck. 2003; 25: 841–847. doi: 10.1002/hed.10304. [DOI] [PubMed] [Google Scholar]
- 6.Clark RL, Hickey RC, Butler JJ, Ibanez ML, Ballantyne AJ. Thyroid cancer discovered incidentally during treatment of an unrelated head and neck cancer: review of 16 cases. Ann Surg. 1966; 163: 665–671. doi: 10.1097/00000658-196605000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ashraf MJ, Alavi MS, Azarpira N, Khademi B. Simultaneous laryngeal squamous cell carcinoma and papillary thyroid carcinoma. Middle East Journal of Cancer. 2011; 2: 87–90. [Google Scholar]
- 8.Bishen KA, Singh A. A case of dual malignancy: Presenting the necessity for extensive sampling for pathologic examination. J Oral Maxillofac Pathol. 2011; 15: 306–310. doi: 10.4103/0973-029X.86698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verma RK, Tripathi N, Aggarwal P, Panda NK. Metastatic papillary carcinoma thyroid co-existing with oral cavity squamous cell carcinoma: A case report and review of literature. Egyptian Journal of Ear, Nose, Throat and Allied Sciences. 2014; 15:125–128. [Google Scholar]
- 10.León X, Sancho FJ, García J, Sañudo JR, Orús C, Quer M. Incidence and significance of clinically unsuspected thyroidtissue in lymph nodes found during neck dissection in head and neck carcinoma patients. Laryngoscope. 2005; 115: 470–474. doi: 10.1097/01.mlg.0000157841.63283.87. [DOI] [PubMed] [Google Scholar]
- 11.López-Escámez JA, López-Nevot A, Moreno-García MI, Gámiz MJ, Salinero J. Cervical metastasis of occult papillary thyroid carcinoma associated with epidermoid carcinoma of the larynx. ORL J Otorhinolaryngol Relat Spec. 1999; 61: 224–226. doi: 10.1159/000027676. [DOI] [PubMed] [Google Scholar]
- 12.Butler JJ, Tulinius H, Ibanez ML, Ballantyne AJ, Clark RL. Significance of thyroid tissue in lymph nodes associated with carcinoma of the head, neck or lung. Cancer. 1967; 20: 103–112. doi: 10.1002/1097-0142(1967)20:1<103::aid-cncr2820200116>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 13.Perie S, Torti F, Lefevre M, Chabbert-Buffet N, Jafari A, Lacau St Guily J. Incidental cervical metastases from thyroid carcinoma during neck dissection. European Annals of Otorhinolaryngology, Head and Neck diseases. 2016; 133: 383–386. doi: 10.1016/j.anorl.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Vassilopoulou-Sellin R, Weber RS. Metastatic thyroid cancer as an incidental finding during neck dissection: significance and management. Head Neck. 1992; 14: 459– 463. doi: 10.1002/hed.2880140606. [DOI] [PubMed] [Google Scholar]
- 15.Resta L, Piscitelli D, Fiore MG, Di Nicola V, Fiorella ML, Altavilla A, et al. Incidental metastases of well-differentiated thyroid carcinoma in lymph nodes of patients with squamous cell head and neckcancer: eight cases with a review of the literature. Eur Arch Otorhinolaryngol. 2004; 261: 473–478. doi: 10.1007/s00405-003-0722-8. [DOI] [PubMed] [Google Scholar]
- 16.Sheahan P, Hafidh M, Toner M, Timon C. Unexpected findings in neck dissection for squamous cellcarcinoma: incidence and implications. Head Neck. 2005; 27: 28–35. doi: 10.1002/hed.20110. [DOI] [PubMed] [Google Scholar]
- 17.Fliegelman LJ, Genden EM, Brandwein M, Mechanick J, Urken ML. Significance and management of thyroid lesions in lymph nodesas an incidental finding during neck dissection. Head Neck. 2001; 23: 885–891. doi: 10.1002/hed.1128. [DOI] [PubMed] [Google Scholar]
- 18.Altumbabic H, Salkic A. Incidental metastasis of papillary thyroid carcinoma in lymph nodes of patient with squamous cell carcinoma of the oral cavity: a case report. Acta Med Sal. 2010;32:104–106. [Google Scholar]