Abstract
Objective: To analyze the clinical results of simultaneously combined anterior and posterior surgery for severe thoracolumbar fracture dislocations, and to clarify the surgical indications for these high‐energy injuries.
Methods: Thirty‐four patients with severe thoracolumbar fracture dislocations were managed with simultaneously combined anterior and posterior surgery. The injured segments included the following: T11 (2 patients), T12 (5), L1 (1), L2 (8), L3 (5), L4 (2) and L4 and L5 (1). When classified according to the Magerl Classification, the breakdown was as follows: 12 A3 injuries, 2 B1, 2 B2, 12 C1 injuries, 4 C2, and 2 C3. Clinical data, including operative procedures, neurological changes, postoperative CT scans and sequential radiographs, was collected and analyzed. Thirty‐two patients were followed up for an average of 13 months (range, 6–60).
Results: Operative time ranged from 180 to 320 min with a mean of 230 min. Intraoperative blood loss ranged from 900 to 2400 ml with a mean of 1200 ml. According to the classification of the American Spinal Injury Association (ASIA), neurological status improved at least 1 grade in all of the 24 patients who had an incomplete paralysis preoperatively. Satisfactory decompressions, reductions and reconstructions were obtained and well maintained in all patients at all intervals of follow‐up.
Conclusion: For severe thoracolumbar fracture dislocations that cannot be effectively treated with either an anterior or posterior approach alone, simultaneously combined anterior and posterior surgery is a reliable method that can achieve a sufficient decompression, reduction and reconstruction.
Keywords: Dislocations, Internal fixators, Lumbar vertebrae, Thoracic vertebrae
Introduction
Thoracolumbar fractures are common injuries in trauma settings. These injuries have become more complex as a result of increasing industrialization in our society. In addition to flexion compression and axial compression forces, thoracolumbar fractures frequently result from torsional and/or tangential impact forces. When these occur, they may result in subluxation and/or dislocation 1 , 2 . Although the indications for the surgical treatment of thoracolumbar fractures remains controversial, most thoracolumbar fractures can be effectively treated with either an anterior or posterior approach. However, due to the complexities of injury, there are some cases of severe fracture dislocations that cannot be effectively treated with an anterior or posterior approach alone 3 . Beginning in October 1998, simultaneously combined anterior and posterior surgery was adopted in our department to manage these severe thoracolumbar fracture dislocations. A retrospective analysis of 34 cases is presented.
Materials and methods
Patients
From October 1998 to September 2005, a total of 192 patients with thoracolumbar fractures with or without dislocations were surgically treated by our department. Among them, 34 severe fracture dislocations were treated with simultaneously combined anterior and posterior surgery. Twenty‐five men and nine women were included with an age range of 18 to 56 years (mean 34.2 years). Twenty‐two of these injuries resulted from traffic accidents, eight from a fall from a height, and four from blows by heavy objects. The affected levels were T11 (n= 2), T12 (n= 5), L1 (n= 11), L2 (n= 8), L3 (n= 5), L4 (n= 2), and L4/5 (n= 1). The mechanisms of injury included flexion compression, axial compression, lateral flexion or distraction, all with an associated torsional or tangential impact. On admission, fourteen patients were in traumatic shock, and nine had associated fractures of the pelvis or limbs, which also required treatment.
Initial physical examination included assessment of any limitation of movement, paresthesia, deformity, and local tenderness. Neurological status was evaluated according to the classification of the American Spinal Injury Association (ASIA), with ASIA A in seven cases, B in ten, C in eight, D in six, E in three, and finally three cases presented with isolated symptoms of nerve root injury. Dysuria occurred in 20 patients including all seven ASIA A patients. For the 15 patients with complete paralysis who were admitted within 8 hours of injury, high dose methylprednisolone was administered intravenously, according to the National Acute Spinal Cord Injury Study (NASCIS II): 30 mg/kg bolus followed by 23 h of continuous infusion of 5.4 mg/kg/h.
All patients were examined with plain radiographs, computed tomography (CT) and magnetic resonance image scans (MRI). Severe three‐column injuries and traumatic canal stenosis were present in all patients. According to the Magerl classification 4 , 12 patients were classified as having Magerl A3 injuries with severe burst fractures, comminuted lamina fractures intruding into the canal, and the cord or dural sac being compressed both anteriorly and posteriorly. Four patients presented as having Magerl B injuries, (two of B1 and two of B2 subtype), which presented as severe flexion and distraction injuries. Eighteen patients with Magerl C injuries were also treated, with twelve C1, four C2 and two C3, including a severe burst fracture accompanied by subluxation in 17 cases, and total dislocation in one case. Anterior or posterior surgery alone was thought to be insufficient for the treatment of these injuries due to the presence of one of the following: spinal cord or dural sac severely compressed both anteriorly and posteriorly; severely comminuted vertebral body fracture in conjunction with distraction‐type posterior fracture or ligamentous rupture; severely comminuted vertebral body fracture with subluxation and a jumped or fractured facet necessitating both anterior and posterior decompression and reduction; or a total dislocation.
Surgical technique
Surgery was performed within 10 days of the injury for all patients. Following the induction of general anesthesia, the patients were positioned on the operating table in the lateral decubitus position, with the most severely occluded canal side placed on the upside, while equivalent occlusion was managed with the left side up (Fig. 1). Posterior surgery was carried out initially, with the operative table tilted anteriorly about 30 degrees. A routine posterior midline incision was made and the posterior elements of the injured vertebrae and adjacent levels were exposed subperiosteally. Four pedicle screws were implanted in the upper and lower adjacent vertebrae under fluoroscopic guidance. Then the fractured lamina and the jumped or fractured facets were excised in order to decompress the dural sac and/or nerve roots. If detected, lacerations of the dural sac were sutured. Following posterior decompression, two contoured rods were connected to the pedicle screws, and a careful reduction was attempted. Then instrumentation was temporarily fixed, and the posterior field was covered in a sterile fashion.
Figure 1.

The patient remains in the lateral decubitus position during the operation, note the mark of incision.
Anterior surgery was carried out with the patients remaining in the same position, while the operating table was flattened. A smaller anterior incision about 15 cm in length, centered at the injured level, was made. Based on the level of injury, either a thoracotomy, retroperitoneal approach, or a combined approach was used to expose the fractured vertebral body and adjacent discs. The upper and lower adjacent discs were excised, followed by subtotal corpectomy. Intracanal fragments of fragmented vertebral body or disrupted disc were also carefully removed. For the patient who presented a total L4,5 dislocation, only the L4‐5 disc was excised due to the integrity of the vertebral bodies. After decompression, the upper and lower adjacent endplates were prepared.
After the posterior field had been decompressed, distractive force was applied using the pedicle instrumentation, while simultaneously anterior reduction force was applied to the displaced vertebral body, and the prepared anterior strut graft inserted to serve as a lever. Thus, coordinated reduction forces opposite to the mechanism of injury were performed simultaneously with the spinal cord under direct visualization. As a result, in all cases a satisfactory reduction was achieved, while the anterior strut graft was simultaneously placed. After that, a compression load was applied to the posterior instrumentation in order to secure the anterior strut graft, and all instruments underwent final tightening.
We experienced more difficulty during reduction in the patient with a total dislocation of L4/5 than with the other fracture patterns. In order to reduce the dislocated L4 vertebral body, a simultaneous anterior and posterior coordinated reduction force was required. Following anterior interbody cage fusion and posterior fixation, anterior screw rod fixation was applied to the vertebral body in order to increase the stability (Fig. 2).
Figure 2.
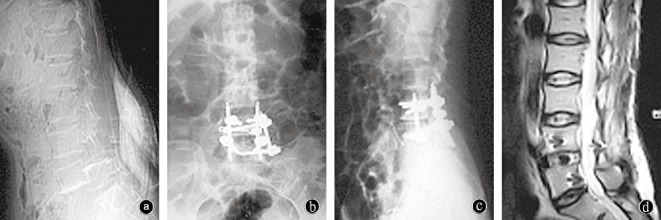
Woman, 48 years old, with L4/5 total dislocation resulting from tangential impact of a truck on her back while she was squatting. Preoperative radiograph (a) shows total L4/5 dislocation accompanied by rotation. Radiographs (b, c) and MRI (d) 6 months after surgery show satisfactory reduction, decompression and reconstruction. She recovered the ability to walk 2 months postop.
Posterolateral grafting was performed with the excised cancellous bone or a harvested iliac crest bone graft. Two drains were placed in the anterior and posterior fields, respectively, and then the incisions were closed routinely.
Short‐segments pedicle instrumentation (Tenor TM, Medtronic Sofamor Danek, Memphis, TN, USA) was used for all patients. Anterior strut graft included tricortical iliac strut grafts in four patients, titanium mesh cages (Medtronic Sofamor Danek) filled with excised cancellous bone in 29 patients, and intervertebral cages (Intromed Medizintechnik GmbH, Wildau, Germany) in the patient with a total L4/5 dislocation.
Operative time ranged from 180 to 320 min, with a mean of 230 min. Intraoperative blood loss ranged from 900 to 2400 ml, with a mean of 1200 ml.
Postoperative care
Rehabilitation of the lower limbs began the day after the operation, while exercise of the lumbar muscles began at approximately 10–14 days postoperative. Finally, activities that involved getting out of bed such as walking or the use of a wheelchair were initiated within 3 weeks of surgery while wearing a corset.
Follow‐up and evaluation
Thirty‐two patients were followed for 6 to 60 months, with an average of 13 months. Two patients were lost at the third month of follow‐up due to a change in address. Neurological status was assessed according to the ASIA classification. Postoperative CT scans and sequential radiographs were collected to evaluate the results including the extent of decompression, adequacy and maintenance of the reduction, and placement of the instrumentation and graft.
Results
The procedure was deemed technically successful, without neurological deterioration, in all 34 patients. During follow‐up, neurological status improved by at least one ASIA grade in 24 patients who had preoperative incomplete paralysis, while no obvious neurological recovery was noted for the seven patients with preoperative complete paralysis. Pain relief and recovery of motor function were also seen in the three patients with nerve root injury. Of the 20 patients with preoperative dysuria, nine recovered complete sphincter function and four experienced a partial improvement, however, no recovery was seen in the seven patients with complete paralysis. Moreover, intercostal nerve pain or local paralyses, which may have resulted from incitation or injury of intercostal nerves during anterior incision, were noted in six patients, and all resolved after physical therapy.
On postoperative CT scans and radiographs, satisfactory decompression and reduction were observed in all patients who experienced recovery of their physical curvature (Fig. 3). For most of the 32 patients followed from 6 to 60 months, continuous rehabilitation was performed. In these patients, reduction and reconstruction were well maintained, and there was no evidence of pseudoarthrosis, obvious loss of correction, or instrument failure on sequential radiographs.
Figure 3.
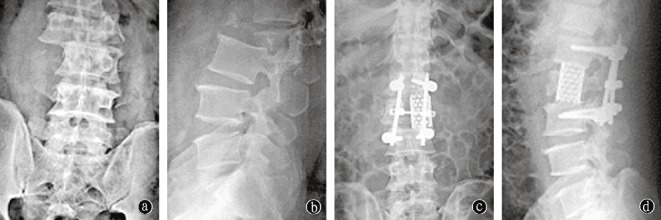
Man, 40 years old, with L2 fracture accompanied with L2/3 rotating dislocation. Preoperative radiographs (a, b) show a severe L2 fracture and dislocation with obvious canal occlusion. Postoperative X‐rays (c, d) show satisfactory reduction, decompression and reconstruction.
Discussion
Thoracolumbar fractures remain the most common spinal injuries in a trauma setting. They commonly result from flexion compression or axial compression forces, but lateral flexion, distraction, torsion and tangential forces can also contribute. In our experience, injury mechanisms have become more complex with the development of industry. Advanced radiography such as reconstructive computer tomography or MRI, can reveal the injury in more detail 5 .
There is significant controversy regarding the optimal surgical approach for thoracolumbar fractures. Most of them can be efficiently treated with either an anterior or a posterior approach, however, a subset of these injuries consist of severe fracture/dislocations that cannot be effectively managed with either approach. For example, fractures with severe comminution and collapse of the vertebral body, or those with canal encroachment, constitute a clear indication for at least an anterior approach. Such injuries may be accompanied by lamina or facet fractures entering the canal, resulting in the spinal cord or dural sac being compressed both anteriorly and posteriorly. This situation can not be managed through one approach. This is particularly true for fractures above the L1 level due to the termination of the cord at that level. At times, large flexion compression forces can result in severe burst fractures with simultaneous failure of the posterior elements, in which case, a posterior reconstruction is also necessary. Although rare, severe burst fractures can also coexist with jumped or fractured facets that will necessitate posterior surgery in order to reduce the subluxated or dislocated joint 3 , 6 . Of the 192 cases of thoracolumbar fractures that have been surgically treated at our institution in recent years, 34 patients with severe fracture dislocations could not be effectively treated with an anterior or posterior approach alone.
The posterior approach is advantageous for treatment of injuries to the posterior elements; including lamina fractures that protrude into the canal, dural lacerations, nerve root injuries and, most commonly, jumped or fractured facets that are irreducible by closed means. Pedicle instrumentation can be useful in obtaining an open reduction and can provide strong fixation by crossing all three vertebral columns 7 , 8 . However, with certain injuries posterior approaches are limited in their ability to decompress the spinal canal, such as when severe vertebral body comminution or collapse exists in association with large fracture fragments extending into the canal. Injuries above the L1 level represent another example because of the danger that exists due to the proximity to the spinal cord. Another limitation of the posterior approach is that it provides insufficient anterior support following a posterior distractive reduction for severe collapsed vertebral body, well known as an ‘egg shell’ deformity, which may result in loss of correction or implant failure 1 , 7 .
An anterior approach is advantageous for direct decompression as less manipulation of the injured cord and/or nerve roots required. In addition, fragmented disc fragments can be completely excised and, from a biomechanical standpoint, strut grafting of the anterior and middle columns is more favorable for obtaining a stable reconstruction and successful fusion 1 , 8 , 9 . However, with the anterior approach it is difficult to address simultaneous posterior injuries, including lamina fractures intruding into the canal, and irreducible jumped or fractured facets. Furthermore, if the posterior elements have completely failed due to distraction forces, such as certain posterior column fractures or ligamentous disruptions that imitate ‘chance fractures’, anterior reconstruction alone cannot restore enough stability 1 , 3 , 10 .
Combined surgery performed as a staged procedure to treat such severe injuries has also been reported, and it is effective in most cases without severe dislocation 6 , 11 . Obviously, a coordinated reduction cannot be performed with staged surgery; moreover, a complete reduction may not be obtainable at subsequent surgeries because of the existing fixation. In addition, with staged procedures the recovery time will likely be prolonged.
However, simultaneously combined anterior and posterior surgery can be performed with the patients remaining in the lateral decubitus position for all these cases. Initially, posterior surgery is performed with implantation of the pedicle screws, followed by laminectomy and/or resection of the jumped or fractured facets in order to release the neural structures. Reduction can then be attempted by utilizing the pedicle instrumentation, followed by temporary fixation of the posterior instrumentation. Anterior surgery is then performed with the patient remaining in the lateral position. A smaller incision can be adopted due to the sparing of anterior fixation at adjacent vertebral bodies. After the posterior release, anterior direct decompression of the intracanal fragments can be performed more safely. Fragmented discs can also be completely excised, followed by removal of cartilage from the adjacent endplates. Following this maneuver, no direct obstruction exists to resist reduction. Coordination of the anterior and posterior reductive forces to counter the injury mechanism can be executed simultaneously, and the anterior strut graft inserted at the same time. Satisfactory reduction can be achieved with successful implantation of the anterior strut graft, while lateral displacement or rotation is reduced simultaneously. This coordinated simultaneous reduction was essential for the case with a total L4/5 dislocation, which did not respond to either an isolated anterior or posterior reduction maneuver. With a thorough decompression, the spinal cord can be inspected directly during the reduction. After the reduction, a compressive load can be applied through the posterior instrumentation in order to secure the anterior graft.
Simultaneously combined surgery is helpful to achieve a complete reduction due to the coordination of anterior and posterior reductive forces, especially in cases of total dislocation. The spinal cord can be more adequately and safely decompressed through combined posterior and anterior approaches. The combination of anterior strut grafting and posterior short‐segment pedicle fixation can restore enough stability, sparing anterior fixation at adjacent bodies and reducing the number of motion segments that require posterior fixation. Single‐stage surgery is also advantageous to shorten recovery time, which helps to minimize postoperative complications.
However, simultaneously combined surgery is more traumatic to the patient than single‐sided surgery, with higher rates of blood loss and longer operative time 3 , 6 , 11 . Also, the lateral decubitus position makes the posterior portion of the surgical procedure technically challenging, especially for pedicle screw insertion. In our series, we applied this dual‐approach only to cases of severe fracture dislocation, which cannot be treated sufficiently with either an anterior or posterior approach alone. Based on our results of the 34 cases that we treated, we believe it to be an effective method of treatment for these severe injuries.
Acknowledgments
We would like to thank Peter G. Passias, MD, from the Department of Orthopaedic Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, MA, USA and Shaobai Wang, PhD, from Massachusetts Institute of Technology, Cambridge, MA, USA for helping to review this article.
References
- 1. Weidenbaux M, Farcy JPC. Surgical management of thoracic and lumbar burst fractures In: Bridwell KH, Dewald RL, eds. The Text Book of Spinal Surgery, 2nd edn. Philadelphia, PA: Lippincott‐Raven Publishers, 1997; 1839–1880. [Google Scholar]
- 2. Langrana NA, Harten RD, Lin DC, et al. Acute thoracolumbar burst fractures: a new view of loading mechanisms. Spine, 2002, 27: 498–508. [DOI] [PubMed] [Google Scholar]
- 3. Xia Q, Xu BS, Zhang JD, et al. The choice and evaluation of anterior, posterior or combined surgery for thoracolumbar burst fractures (Chin). Zhonghua Gu Ke Za Zhi, 2004, 24: 718–722. [Google Scholar]
- 4. Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J, 1994, 3: 184–201. [DOI] [PubMed] [Google Scholar]
- 5. Haba H, Taneichi H, Kotani Y, et al. Diagnostic accuracy of magnetic resonance imaging for detecting posterior ligamentous complex injury associated with thoracic and lumbar fractures. J Neurosurg, 2003, 99: 20–26. [DOI] [PubMed] [Google Scholar]
- 6. Ramani PS, Singhania BK, Merthy G. Combined anterior and posterior decompression and short segment fixation for unstable burst fractures in the dorso lumbar region. Neurol India, 2002, 50: 272–278. [PubMed] [Google Scholar]
- 7. Xu BS, Tang TS, Yang HL. The long‐term results of thoracolumbar burst fractures treated with short‐segment pedicle instrumentation (Chin). Zhonghua Gu Ke Za Zhi, 2002, 22: 641–647. [Google Scholar]
- 8. Sasso RC, Renkens K, Hanson D, et al. Unstable thoracolumbar burst fractures, anterior‐only versus short‐segment posterior fixation. J Spinal Disord Tech, 2006, 19: 242–248. [DOI] [PubMed] [Google Scholar]
- 9. Mariotti AJ, Diwan AD. Current concepts in anterior surgery for thoracolumbar trauma. Orthop Clin North Am, 2002, 33: 403–412. [DOI] [PubMed] [Google Scholar]
- 10. Wilke HJ, Kemmerich V, Claes LE, et al. Combined anteroposterior spinal fixation provides superior stabilisation to a single anterior or posterior procedure. J Bone Joint Surg Br, 2001, 83: 609–617. [DOI] [PubMed] [Google Scholar]
- 11. Renshaw TS, Newington CT. Anterior/posterior spine surgery done as one‐stage versus two‐stage procedures. In: Annual Meeting of American Academy of Orthopaedic Surgeons, 1992.


