ABSTRACT
Eruptive xanthoma is characterized by yellowish skin papules encircled by an erythematous halo and associated with severe hypertriglyceridemia above 2,000 mg/dl. Hypertriglyceridemia can be caused by primary genetic mutations, secondary causes, such as uncontrolled diabetes, obesity, alcohol overuse, or combinations of both. Eruptive xanthoma can serve as an important clinical indicator of underlying systemic conditions (e.g. hypertriglyceridemia and uncontrolled diabetes mellitus). It is important for clinicians to recognize it to prevent further complications such as pancreatitis and cardiovascular disease.
KEYWORDS: Eruptive xanthoma, hypertriglyceridemia, type 1 diabetes mellitus, pancreatitis, cardiovascular disease, Apo B/A1 ratio, fenofibrate, life style modification
1. Introduction
Dermatologic manifestations can be an early warning sign of underlying systemic conditions. Early recognition of the cutaneious lesions of medical conditions can prevent severe complications with timely work up and treatment. Eruptive xanthoma is characterized by an eruption of yellowish skin papules, encircled by an erythematous halo, most commonly arising over the extensor surfaces of the extremities, on the buttocks and shoulders. Eruptive xanthoma is caused by an increased local extravasation of lipids through the vascular wall to the interstitial space of connective tissues [1–3]. We present a patient with a longstanding history of type I diabetes mellitus who developed multiple pruritic yellowish, erythematous papules on the extensor surfaces of the extremities consistent with eruptive xanthoma.
2. Case description
An 18-year-old Hispanic female with a history of poorly controlled type I diabetes mellitus for 7 years was brought to the emergency department, complaining of nausea, dizziness, and skin lesions. The patient stopped taking insulin for a few months because she thought her skin lesions were getting worse due to insulin. Vital signs were within normal limits. On physical exam, the lesions were pruritic, non-tender, erythematous papules with yellow-colored centers on her both elbows and knees (Figure 1, 2).
Figure 1.

Eruptive xanthoma in left lower extremity extensor.
Figure 2.

Eruptive xanthoma in bilateral lower extremities extensors.
Initially, the glucose level was 454 mg/dL with bicarbonate 10 mmol/L, anion gap of 21. Urine analysis revealed 3+ ketones and 3+ glucose. Patient’s HbA1C level was 12.1%. The patient was admitted for diabetic ketoacidosis and treated with insulin. Lipid panel revealed total cholesterol level 429 mg/dl, high density lipoprotein 14 mg/dl, low density lipoprotein 68 mg/dl and total triglyceride (TG) 2,243 mg/dl. Further blood tests revealed apolipoprotein (apo) E genotype of E3/E4, elevated Apo B of 327 mg/dL, and normal level Apo A1 of 118 mg/dL, indicating elevated apo B/A1 ratio of 2.77.
She was started on fenofibrate for severe hypertriglyceridemia, in addition to diet and life style modification and was discharged home. On a follow up office visit exam after two months, her triglyceride level was markedly decreased to 328 mg/dL and her skin lesions showed significantly decreased papule size which was estimated around 70% reduction (Figure 3). She continues to be evaluated for routine follow-up care.
Figure 3.
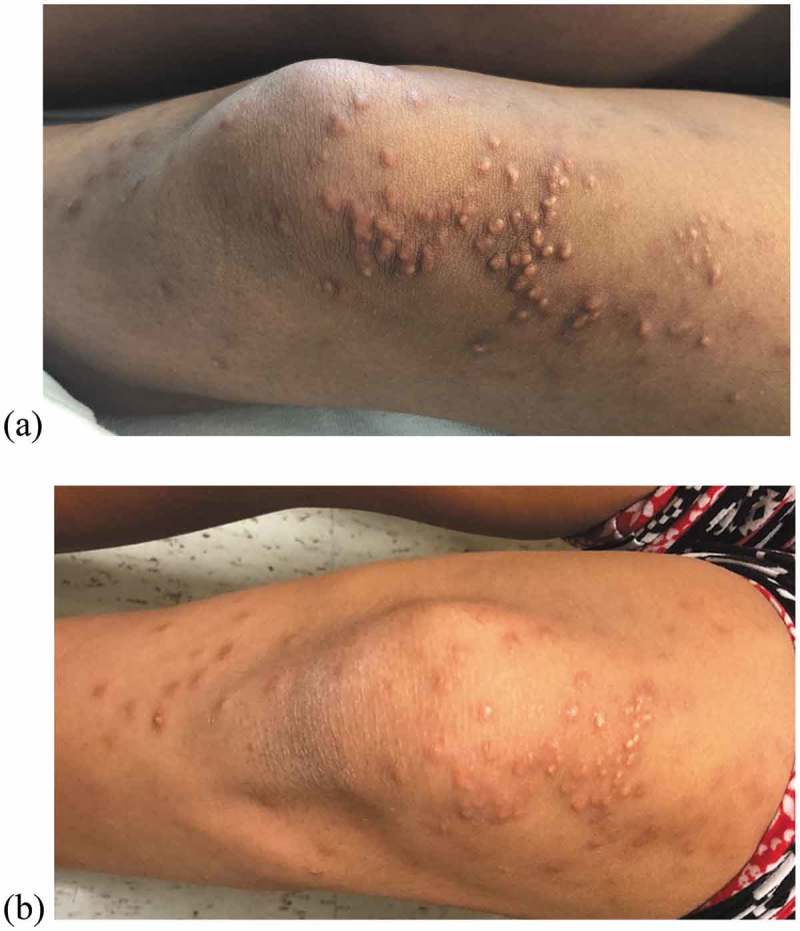
(a) Before treatment, (b) 2 months after treatments.
3. Discussion
Xanthomas are disorders of lipoprotein metabolism and formed by an accumulation of cholesterol-rich substance. Several types of xanthomas can be classified based on clinical manifestations. Xanthelasma is the most common form which showed 4.4% in the population with an even distribution between men and women in a recent prospective study [4]. Xanthelasma usually presents on or around the eyelids with bilateral and symmetric distribution and the lesions are soft, yellow, small, nontender, nonpruritic papules around the eyelids. Xanthelasma can occur without hyperlipidemia, particularly in older patients, but is often associated with familial dyslipidemias when seen in a younger patient. Tuberous xanthomas are primarily located over joints and present as firm, painless, red-yellow nodules that often merge into forming multi-lobated tumor-like lesions. They can be associated with severe hypercholesterolemia and elevated LDL levels and some of the secondary hyperlipidemia (e.g. nephrotic syndrome, hypothyroidisom). Tendinous xanthomas are slowly enlarging subcutaneous nodules in association with the tendons or the ligaments. The usual locations include the extensor tendons of the hands, the feet and the Achilles tendons. The tendinous xanthomas associated with severe hypercholesterolemia and elevated LDL levels, particularly in familial hypercholesterolemia [3,4].
Eruptive xanthomas commonly arise over the extensor surfaces of the extremities, the buttocks and the shoulders. The lesions erupt as small, red-yellow papules with erythematous base. Pruritus is common and lesions may become tender. Eruptive xanthomas often indicate severe hypertriglyceridemia and uncontrolled diabetes mellitus [2]. Eruptive xanthoma is retrospectively reported in about 10% of patients with severe hypertriglyceridemia [3].
The diagnosis of xanthomas is usually based on the clinical evaluation. When diagnosis is unclear in clinical bases, skin biopsy for histopathological confirmation is indicated [3]. Histologically, xanthomas show an accumulation of lipids in large foamy cells (lipid-laden macrophages).
Recognizing eruptive xanthomas as a clinical sign for underlying systemic diseases is an important step to evaluate and manage these conditions. In short term, one major reason to treat hypertriglyceridemia is to prevent acute pancreatitis, which has been intimately associated with severe hypertriglyceridemia. Another potential important risk associated with hypertriglyceridemia is a cardiovascular disease. The relationship between triglycerides and cardiovascular disease is less clear. Therefore, additional lab tests can further help to identify patients with a higher risk to develop cardiovascular disease. As noted in our patient, apo E genotype of E3/E4 has been associated with greater risk of developing heart disease, high LDL cholesterol and triglyceride level. Patents with the E3/E4 genotype are known to respond poorly to statins, but well on a low-fat diet [5]. The elevated Apo B/A1 ratio in our patient is another indicator to support a greater risk of cardiovascular disease. As shown in the global INTERHEART study, ApoB/A1 ratio is the most important risk factor for myocardial infarction in all geographic regions [6].
The management of hypertriglyceridemia include both pharmacologic therapy as well as life style modification especially the patient like ours with E3/E4 genotype. Fibrates are the first-line treatment to significantly reduce the risk of pancreatitis with a triglyceride-lowering effect [2]. Nicotinic acid, omega-3 fatty acids, and bile acid sequestrants are also effective as well. The clinical signs of hypertriglyceridemia, eruptive xanthoma typically resolved with treatment [7,8].
4. Conclusion
Eruptive xanthoma should be recognized as an indicator of underlying systemic conditions such as hypertriglyceridemia and uncontrolled diabetes mellitus to prevent pancreatitis and cardiovascular disease. Additional work-up for apolipoproteins can provide valuable risk stratification and more individualized management plans for future cardiovascular disease.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Durrington P. Dyslipidaemia. Lancet. 2003;362:717–731. [DOI] [PubMed] [Google Scholar]
- [2].Hegele RA, Ginsberg HN, Chapman MJ, et al. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2:655–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Zak A, Zeman M, Slaby A, et al. Xanthomas: clinical and pathophysiological relations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158:181–188. [DOI] [PubMed] [Google Scholar]
- [4].Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ. 2011;343:d5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Griffin BA, Walker CG, Jebb SA, et al. APOE4 Genotype Exerts Greater Benefit in Lowering Plasma Cholesterol and Apolipoprotein Bthan Wild Type (E3/E3), after Replacement of Dietary Saturated Fats with Low Glycaemic Index Carbohydrates. Nutrients. 2018 Oct 17;10(10). pii: E1524. doi: 10.3390/nu10101524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- [7].Vangara SS, Klingbeil KD, Fertig RM, et al. Severe hypertriglyceridemia presenting as eruptive xanthomatosis. J Family Med Prim Care. 2018;7:267–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Abdelghany M, Massoud S. Eruptive xanthoma. Cleve Clin J Med. 2015;82:209–210. [DOI] [PubMed] [Google Scholar]


