Abstract
Background/purpose
Implant-abutment connection is the component responsible for the transmitting of occlusal force from the crown down to the implant fixture. Different connection geometric structure will lead to different mechanical performance. The purpose of this study was to compare the stability of internal hex Implant -abutment connection with internal hex with Morse taper implant-abutment connection by testing their compressive strength.
Materials and methods
This was an in vitro study. The test group and the control group had 8 specimens separately. The test group was internal hex combined with Morse taper implant connection design, and the control group was internal hex connection design. Static force was applied to the specimens at a 30° angle until failure. The testing protocol was designed according to ISO14801 regulations. We compared the compressive strength of both groups.
Results
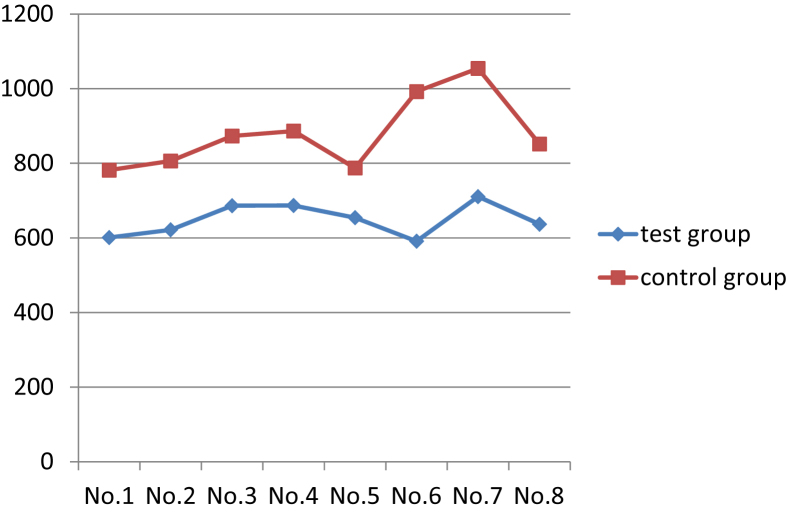
The control group showed significantly higher compressive strength than the test group (p < 0.0001).
Conclusions
For the compressive strength of implant abutment complex, incorporating Morse taper design into internal hex connection failed to enhance its mechanical performance. According to this study, internal hex connection has higher compressive strength than internal hex connection combined with Morse taper design.
Keywords: Compressive strength, Implant connection, Implant abutment complex, Morse taper, Internal hex
Introduction
Implant-abutment connection is the component responsible for transmitting of occlusal force from the crown down to the implant fixture. The implant-abutment connection designs could be categorized into external connection, which means the connecting part is above the implant platform, and internal connection, which means the connecting part is submerged into implant fixture. Unstable implant-abutment complex will cause leakage at the implant–abutment interface and the corresponding bacterial contamination will lead to crestal bone loss or peri-implantitis.1, 2, 3, 4
Complications of implant treatment could be generally divided into six categories including surgical, implant loss, bone loss, peri-implant soft tissue, mechanical, and esthetics/phonetics.5, 6, 7 When it comes to mechanical complications, the cumulative incidence of connection-related complications (screw loosening or fracture) was 7.3% which was second to 14% for suprastructure-related complications (veneer and framework fracture) in systematic review conducted by Pjetursson.8
The purpose of this study was to compare the stability of internal hex implant-abutment connection with internal hex with Morse taper implant-abutment connection by testing their compressive strength.
Materials and methods
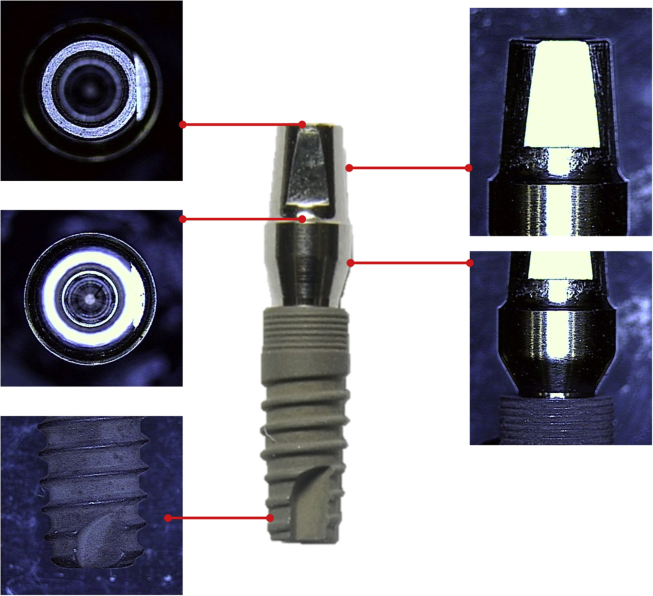
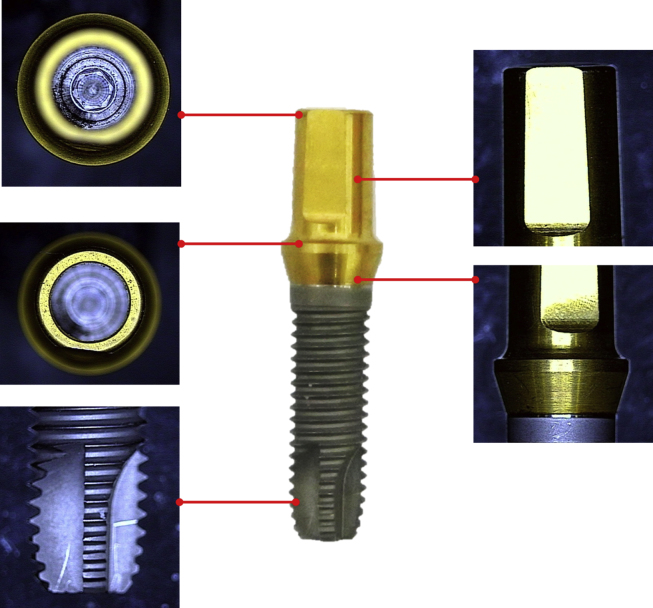
The following implant systems were included and divided into test group (Fig. 1) and control group (Fig. 2). Test group: cementable abutment with internal hex combined with Morse taper connection design, 4 mm in diameter (ComMed series dental implant system, Chang Gung medical technology Co., Ltd, Taiwan). Control group: Gingihue abutment with internal hex connection design, 4 mm in diameter (Certain implant system, Biomet 3i, Palm Beach Gardens, USA).
Figure 1.
Cementable abutment with internal hex combined with morse taper connection design (ComMed series dental implant system, Chang Gung medical technology Co., Ltd, Taiwan).
Figure 2.
Gingihue abutment with internal hex connection design (Certain implant system, Biomet 3i, Palm Beach Gardens, USA).
Each group had 8 specimens. All the implant abutments were connected to the implant fixtures according to the manufacturers' instructions. A torque wrench was used to apply 20-Ncm torque for tightening of the fastening screws on all the specimens. The torque value was also suggested by the manufacturers.
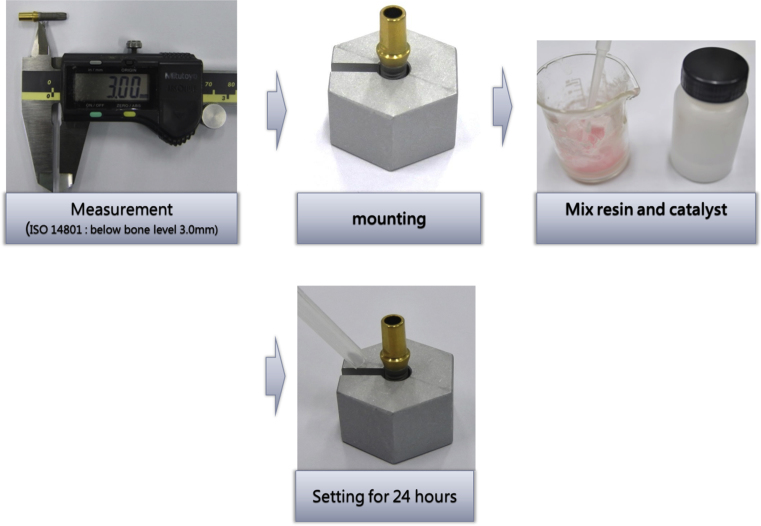
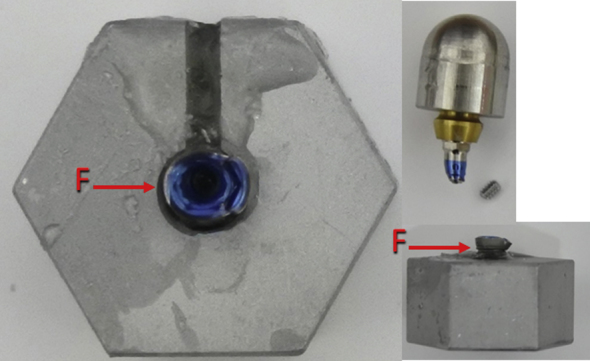
The hollow hexagonal stainless steel specimen holder was fabricated to mount the test specimens. The specimen was temporarily fixed in the hollow hexagonal stainless steel specimen holder by clay. And the epoxy resin was poured to fill the hollow hexagonal stainless steel specimen holder and the resin was allowed to set for 24 h at 24 °C. According to ISO14801 protocol, the module of elasticity of the resin was higher than 3 × 109N/M2 to simulate the module of elasticity of the surrounding bone.
The level of epoxy resin was below the implant platform 3.0 mm ± 0.5 mm according to ISO14801 protocol. For many endosseous dental implants, it is known that the marginal bone level can move apically following implantation to a relatively steady-state level. The distance of 3.0 mm was chosen to provide a representative case with respect to bone loss. Fig. 3 shows step by step mounting procedures.
Figure 3.
Step by step mounting procedures.
The custom made deformation-resistant loading member with a hemispherical contact surface for load transfer was fabricated. The loading force of the testing machine was applied through the deformation-resistant loading member with a hemispherical contact surface for load transfer, attached to the implant abutment. The center of the hemisphere was on the central longitudinal axis of the dental implant. The long axis of the specimens makes a 30° ± 2° angle with loading direction of the testing machine (Fig. 4).
Figure 4.
The long axis of the specimens makes a 30° ± 2° angle with the loading direction of the testing machine.
Instron E3000 with axial load cell (Instron, Canton, MA, USA) was applied for the testing (Fig. 5). Its static force capacity is ±2100N and its load accuracy is within ±5%. The compression load was applied to the specimens until failure, which was defined as fracture of implant-abutment connection or permanent deformation of the implant-abutment connection occurred. The maximum single impact loading to failure was recorded by computer.
Figure 5.

Instron E3000 with axial load cell (Instron, Canton, MA, USA).
The outcome variable was compressive strength and the dependent variable was the connection designs. SPSS 15.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Two sample t test was used to compare the 2 groups and the level of statistical significance was set at 5% (α = 0.05).
Results
The internal hex design implant-abutment connection design demonstrated higher compressive strength then internal hex combined with Morse taper design. Internal hex design group showed mean compressive strength 879.1N which is significantly higher than internal hex combined with Morse taper group (648.6N).
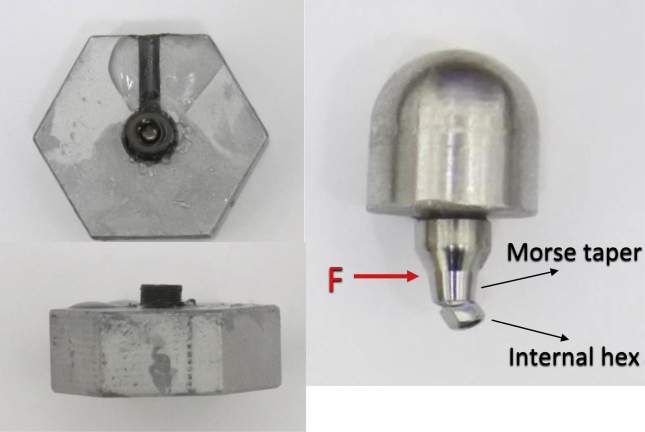
In control group, six specimens out of eight showed abutment screw fracture with deformation over fixture platform area (Fig. 7). Two other specimens showed deformation over fixture abutment interface with gap formation (Fig. 8). In test group, half of the specimens showed abutment screw fracture and evident deformation over interface between internal hex and Morse taper (Fig. 9). Another half showed deformation over fixture abutment interface without screw fracture (Fig. 10).
Figure 7.
3i internal hex implant system after loading. Abutment screw fractured with deformation over fixture platform area was noted.
Figure 8.

3i internal hex implant system after loading. Gap formation over fixture abutment interface was noted.
Figure 9.
Commed internal hex with Morse taper implant system after loading. Abutment screw fracture was noted. Severe deformation occurred over interface between internal hex and Morse taper.
Figure 10.

Commed internal hex with Morse taper implant system after loading. Deformation over fixture abutment interface was noted.
The two tailed P value is less than 0.0001. Table 1 and Fig. 6 show the compressive strength of individual specimens.
Table 1.
Descriptive statistics for compressive strength (N) at implant failures.
| Group | N | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| Test group | 8 | 591.15 | 710.78 | 648.61 | 43.46 |
| Control group | 8 | 781.73 | 1054.27 | 879.19 | 98.23 |
Figure 6.
Comparison of compressive strength (N) between test group and control group.
Discussion
Coppede, A. R. et al. conducted an in vitro study comparing the compressive strength of the internal hex connection and the internal cone (Morse taper) connection.9 The results showed that maximum deformation force for internal cone implant (905.8 ± 67.2 N) was statistically higher than that for internal hex implants (837.3 ± 49.4N) (P = 0.0182), which means Morse taper connection design could provide better stability comparing to internal hex design. However, comparing to Morse taper connection, internal hex connection could provide limited path of insertion which make it easier for prosthetic procedures when using multiple units or angled abutments. Furthermore, dental implants with Morse taper connection or internal hex connection showed similar failure rate.10 Since these two types of connection designs have their own advantages and disadvantages, recently, manufacturers combined these two types of connection designs and came up with internal hex combined with Morse taper design.11,12 Hopefully, this new design can combine the benefits of internal hex and Morse taper designs.
Villarinho, E. A. et al. compared the removal torque value of Morse taper connection and internal hex combined Morse taper connection after fatigue loading test.13 The removal torque value showed that the presence of a positioning index might negatively affect the biomechanical stability of the tapered abutment screws. Comparison between both groups indicated that internal hex connection combined with Morse taper design had higher preload loss of 56.65% while morse taper connection design exhibited lower preload loss of 13.84% (P < 0.001) after mechanical loading. The result showed that the mechanical performance of Morse taper connection design deteriorated after incorporating hex design with it. Consequently, the question will be whether the mechanical performance of internal hex connection design could be enhanced by incorporating Morse taper design with it or not?
In our study, the mean compressive strength of internal hex connection group was 879.1N which was similar to the result of the study done by Coppede (837.3N).9 Unfortunately, the compressive strength was not enhanced by incorporating Morse taper design with internal hex design. The mean compressive strength of internal hex combined with Morse taper design was 648.6N, which was significant lower than internal hex group (P < 0.0001).
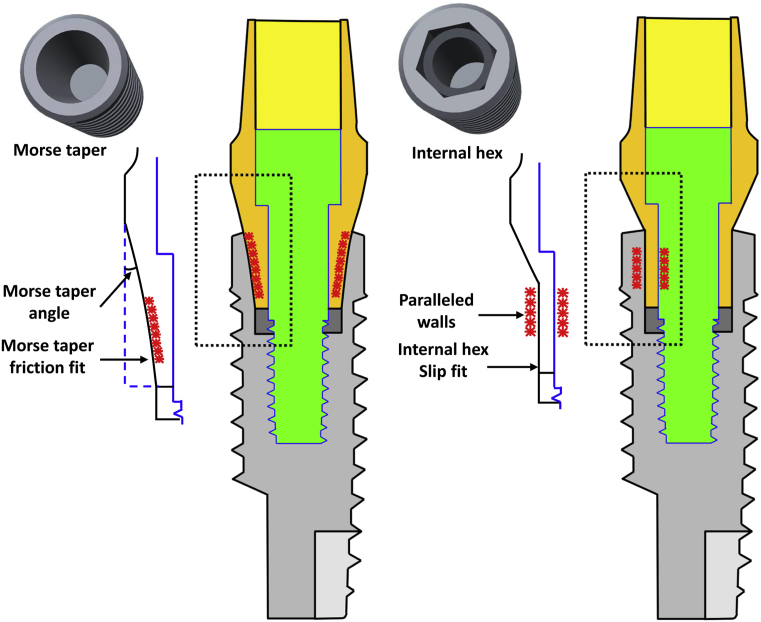
According to Binon's classification, implant-abutment connection design could be classified into slip-fit joint or friction-fit joint (Fig. 11).14 A Slip-fit joint had a slight space existing between the mating parts, and the connection is passive for the convenience of clinical adaptation and fitting of the abutments. Internal hex connection is a kind of slip-fit connection. The stability of this kind of connection comes not only from the precision of manufacturing but also the vertical length of the connection. Incorporating Morse taper design into internal hex connection would decrease the vertical length of the internal hex part which might lead to the decrease of the stability. A friction-fit joint design leaves no space between the fixture and the abutment. They are literally forced together and its stability is related to the surface area of two metallic contact surfaces.15,16 Morse taper connection is one kind of friction-fit joint design. The reduction of surface area of Morse taper connection design caused by incorporating internal hex design with it might also lead to the reduction of its cold welding effect.13,17 That is the possible reason why the result of this study showed lower compressive strength after combining these two connection designs. In the test group, the specimens showed severe deformation over interface between internal hex and Morse taper (Fig. 8) suggesting that it is a weak point. Because of the geometric discontinuity over the transition zone from Morse taper to internal hex, intensity of local stress field increased. This also explained why test group showed lower compressive strength.
Figure 11.
A Slip-fit joint had a slight space existing between the mating parts, and the connection is passive between the mating parts. A friction-fit joint design leaves no space between the fixture and the abutment. They are literally forced together.
In our study we set the test methods based on ISO14801 protocol. This International Standard is most useful for comparing endosseous dental implants of different designs or sizes.18,19 Several previous studies compared different implant designs applying this protocol in terms of stress and strain distribution,20,21 torque evaluation,13,22 and bending moment.23, 24, 25 By using the same protocol, comparing between different studies could be possible.
According to Umesh, they conducted the in vivo dynamic measurement of the biting force generated by individual tooth using a Fiber Bragg Grating Bite Force Recorder (FBGBFR).26 The result showed that maximum biting force for incisors was 320N, and for premolars and molars were 464N and 744N respectively. So in clinical application, for incisors and premolars, it is safe to use both internal hex design and internal hex combined with Morse taper design. However, when it comes to molar area, it should be prudent to use internal hex combined with Morse taper design because its compressive strength in this study is 648N which is lower than the maximum biting force recorded by Umesh. Internal hex connection could be more capable of withstanding occlusal force in molar area.
The limitation of the current study was that it couldn't simulate the dynamic force system, humidity, and thermal cycle of the intraoral environment. In the future study, we might consider incorporating fatigue testing, artificial saliva bath, and thermal cycling to further simulate intraoral environment.
Conflicts of interest
None declared.
References
- 1.Persson L.G., Lekholm U., Leonhardt A., Dahlen G., Lindhe J. Bacterial colonization on internal surfaces of Branemark system implant components. Clin Oral Implants Res. 1996;7:90–95. doi: 10.1034/j.1600-0501.1996.070201.x. [DOI] [PubMed] [Google Scholar]
- 2.Tsuruta K., Ayukawa Y., Matsuzaki T., Kihara M., Koyano K. The influence of implant-abutment connection on the screw loosening and microleakage. Int J Implant Dent. 2018;4:11. doi: 10.1186/s40729-018-0121-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tallarico M., Canullo L., Caneva M., Ozcan M. Microbial colonization at the implant-abutment interface and its possible influence on periimplantitis: a systematic review and meta-analysis. J Prosthodont Res. 2017;61:233–241. doi: 10.1016/j.jpor.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Liu Y., Wang J. Influences of microgap and micromotion of implant-abutment interface on marginal bone loss around implant neck. Arch Oral Biol. 2017;83:153–160. doi: 10.1016/j.archoralbio.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 5.Goodacre C.J., Bernal G., Rungcharassaeng K., Kan J.Y. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- 6.Liaw K., Delfini R.H., Abrahams J.J. Dental implant complications. Semin Ultrasound CT MR. 2015;36:427–433. doi: 10.1053/j.sult.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Wittneben J.G., Buser D., Salvi G.E., Burgin W., Hicklin S., Bragger U. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: a 10-year retrospective study. Clin Implant Dent Relat Res. 2014;16:356–364. doi: 10.1111/cid.12066. [DOI] [PubMed] [Google Scholar]
- 8.Pjetursson B.E., Tan K., Lang N.P., Brägger U., Egger M., Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15:625–642. doi: 10.1111/j.1600-0501.2004.01117.x. [DOI] [PubMed] [Google Scholar]
- 9.Coppede A.R., Bersani E., de Mattos Mda G., Rodrigues R.C., Sartori I.A., Ribeiro R.F. Fracture resistance of the implant-abutment connection in implants with internal hex and internal conical connections under oblique compressive loading: an in vitro study. Int J Prosthodont. 2009;22:283–286. [PubMed] [Google Scholar]
- 10.Cannata M., Grandi T., Samarani R., Svezia L., Grandi G. A comparison of two implants with conical vs internal hex connections: 1-year post-loading results from a multicentre, randomised controlled trial. Eur J Oral Implantol. 2017;10:161–168. [PubMed] [Google Scholar]
- 11.de Oliveira Silva T.S., Mendes Alencar S.M., da Silva Valente V., de Moura C. Effect of internal hexagonal index on removal torque and tensile removal force of different Morse taper connection abutments. J Prosthet Dent. 2017;117:621–627. doi: 10.1016/j.prosdent.2016.07.024. [DOI] [PubMed] [Google Scholar]
- 12.Cerutti-Kopplin D., Rodrigues Neto D.J., Lins do Valle A., Pereira J.R. Influence of reverse torque values in abutments with or without internal hexagon indexes. J Prosthet Dent. 2014;112:824–827. doi: 10.1016/j.prosdent.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Villarinho E.A., Cervieri A., Shinkai R.S., Grossi M.L., Teixeira E.R. The effect of a positioning index on the biomechanical stability of tapered implant-abutment connections. J Oral Implantol. 2015;41:139–143. doi: 10.1563/AAID-JOI-D-12-00245. [DOI] [PubMed] [Google Scholar]
- 14.Binon P.P. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants. 2000;15:76–94. [PubMed] [Google Scholar]
- 15.Merz B.R., Hunenbart S., Belser U.C. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000;15:519–526. [PubMed] [Google Scholar]
- 16.Ricciardi Coppede A., de Mattos Mda G., Rodrigues R.C., Ribeiro R.F. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: an in vitro study. Clin Oral Implants Res. 2009;20:624–632. doi: 10.1111/j.1600-0501.2008.01690.x. [DOI] [PubMed] [Google Scholar]
- 17.Schmitt C.M., Nogueira-Filho G., Tenenbaum H.C. Performance of conical abutment (Morse Taper) connection implants: a systematic review. J Biomed Mater Res A. 2014;102:552–574. doi: 10.1002/jbm.a.34709. [DOI] [PubMed] [Google Scholar]
- 18.Marchetti E., Ratta S., Mummolo S. Mechanical reliability evaluation of an oral implant-abutment system According to UNI EN ISO 14801 fatigue test protocol. Implant Dent. 2016;25:613–618. doi: 10.1097/ID.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 19.Marchetti E., Ratta S., Mummolo S. Evaluation of an endosseous oral implant system according to UNI EN ISO 14801 fatigue test protocol. Implant Dent. 2014;23:665–671. doi: 10.1097/ID.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 20.Covani U., Ricci M., Tonelli P., Barone A. An evaluation of new designs in implant-abutment connections: a finite element method assessment. Implant Dent. 2013;22:263–267. doi: 10.1097/ID.0b013e318292625f. [DOI] [PubMed] [Google Scholar]
- 21.Geringer A., Diebels S., Nothdurft F.P. Influence of superstructure geometry on the mechanical behavior of zirconia implant abutments: a finite element analysis. Biomed Tech (Berl) 2014;59:501–506. doi: 10.1515/bmt-2013-0088. [DOI] [PubMed] [Google Scholar]
- 22.Park J.K., Choi J.U., Jeon Y.C., Choi K.S., Jeong C.M. Effects of abutment screw coating on implant preload. J Prosthodont. 2010;19:458–464. doi: 10.1111/j.1532-849X.2010.00595.x. [DOI] [PubMed] [Google Scholar]
- 23.Truninger T.C., Stawarczyk B., Leutert C.R., Sailer T.R., Hammerle C.H., Sailer I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation. Clin Oral Implants Res. 2012;23:12–18. doi: 10.1111/j.1600-0501.2010.02141.x. [DOI] [PubMed] [Google Scholar]
- 24.Leutert C.R., Stawarczyk B., Truninger T.C., Hammerle C.H., Sailer I. Bending moments and types of failure of zirconia and titanium abutments with internal implant-abutment connections: a laboratory study. Int J Oral Maxillofac Implants. 2012;27:505–512. [PubMed] [Google Scholar]
- 25.Muhlemann S., Truninger T.C., Stawarczyk B., Hammerle C.H., Sailer I. Bending moments of zirconia and titanium implant abutments supporting all-ceramic crowns after aging. Clin Oral Implants Res. 2014;25:74–81. doi: 10.1111/clr.12192. [DOI] [PubMed] [Google Scholar]
- 26.Umesh S., Padma S., Asokan S., Srinivas T. Fiber Bragg Grating based bite force measurement. J Biomech. 2016;49:2877–2881. doi: 10.1016/j.jbiomech.2016.06.036. [DOI] [PubMed] [Google Scholar]