A 21-year-old man with atopic diathesis presented with multiple pin-head-sized erythematous to light brown-colored, non-scaly, keratotic follicular papules, closely clustered over the anterior aspect of thighs [Figure 1] and outer arms for past 6–7 years, associated with occasional itching. His sibling had similar lesions. There was no evidence of facial/truncal acne, seborrheic dermatitis, or spiny papules over the knees or elbows. Palms, soles, nails, and mucosae were unremarkable. A differential diagnosis of keratosis pilaris (KP), follicular psoriasis, phrynoderma, and pityrosporum folliculitis was considered.
Figure 1.

Multiple pin-head-sized erythematous to light brown-colored, non-scaly, keratotic follicular papules, closely clustered over the anterior aspect of the thigh
Polarized dermoscopy from thigh lesions revealed a faint reddish-light brown background with scattered vascular ectasias, twisted hairs forming loops and irregular coils, and vellus hairs [Figure 2a]. Dermoscopy from the outer arm additionally revealed perifollicular papular erythema, hairs emerging in groups of 2–3, focal peripilar casts, and scattered pigmented globules [Figure 2b]. Basket weave and lamellated orthokeratosis, follicular infundibular dilatation and plugging with focal peri-infundibular parakeratosis, perifollicular lymphocytic infiltrate, and absence of yeast cells on histopathology [Figure 3] confirmed the clinicodermoscopic diagnosis of KP.
Figure 2.
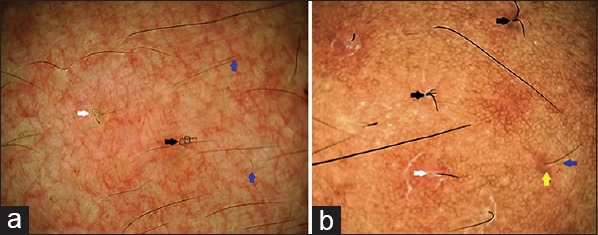
Dermoscopic features from lesions of keratosis pilaris: (a) from the thigh revealing faint reddish-light brown background with scattered vascular ectasias, twisted hairs forming loops (white arrow) and irregular coils (black arrow), and presence of vellus hairs (blue arrows); and (b) from the outer arm showing scattered vellus hairs (blue arrow), perifollicular papular erythema (yellow arrow), hairs emerging in groups of 2–3 (black arrow), and focal peri-pilar cast (white arrow). Appreciate the additional presence of scattered pigmented brown-colored globules. (E-scope videodermoscope, polarized mode, ×20)
Figure 3.
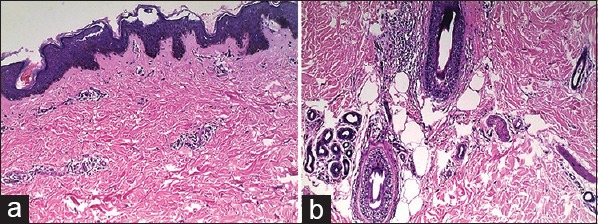
Histopathology from thigh lesion revealing (a) basket weave and lamellated orthokeratosis, and (b) follicular infundibular dilatation and plugging with focal peri-infundibular parakeratosis, and perifollicular lymphocytic infiltrate confirming the diagnosis of active keratosis pilaris (hematoxylin and eosin, ×100 and ×400)
KP, characterized by clustered 1 mm-sized, folliculo-centric keratotic papules with surrounding erythema, typically involving the extensor aspect of forearms and thighs is a common autosomal dominant dermatosis.[1,2] Common differentials include phrynoderma, follicular psoriasis, seborrheids, truncal acne, and folliculitis. Although skin biopsy is diagnostic, dermoscopy facilitates instant non-invasive diagnosis of this benign condition.
The exact pathogenesis of KP remains unclear. The likelihood of KP being a disorder of keratinization has been challenged by Thomas and Khopkar, based on their dermoscopic findings.[3] They have suggested the coiled hair shaft to be central to its histogenesis that ruptures the follicular epithelium leading to inflammation and abnormal follicular keratinization.
Dermoscopic features of KP include presence of vellus hairs that are frequently coiled, semi-circular or looped, peri-follicular erythema, and peri-pilar casts.[3,4] Hairs may emerge in groups of 2 or 3. Vascular ectasias have been described.[5] Although never described earlier, dyschromic changes (pigmented globules) seen in this case have been observed in older healing lesions in majority of Indian patients, suggesting postinflammatory hyperpigmentation. This may represent the quintessential difference between dermoscopic features of cutaneous conditions in darker versus lighter skin types.[6] Table 1 details the dermoscopic differentiation of KP from its close clinical simulators.[3,4,7,8,9,10]
Table 1.
Dermoscopic features of keratosis pilaris and important conditions with similar clinical morphology
| Name of the condition | Dermoscopic features |
|---|---|
| Keratosis pilaris | Presence of vellus hairs that are frequently coiled, semi-circular, or looped |
| Peri-follicular erythema and peri-pilar casts | |
| Hairs emerging in groups of 2 or 3. | |
| Vascular ectasias | |
| Pigmented structures in healed/late lesions (documented for the first time in this report) | |
| Follicular psoriasis | White-brown background |
| Morphologically normal looking terminal hairs | |
| Perifollicular scales | |
| Multiple red dots/dotted vessels, red globules, twisted red loops, and glomerular vessels | |
| Hypovitaminosis-A associated phrynoderma | Follicular papules with translucent spines |
| Perilesional “floret-like” structures | |
| Perforating folliculitis | Bright white clods centered in a structureless grey area surrounded by reticular brown lines |
| Pityriasis rubra pilaris | White keratotic plugs |
| Yellow peripheral keratotic ring | |
| Perifollicular erythema | |
| Linear vessels | |
| Pityrosporum folliculitis | Perifollicular papules and pustules with surrounding erythema and dirty-white scaling |
| Keratosis pilaris-like coiled/looped hair follicles with perifollicular erythema and scaling may be seen in around 50% cases | |
| Hypopigmentation of the involved hair shaft |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Baden HP, Byers HR. Clinical findings, cutaneous pathology and response to therapy in 21 patients with keratosis pilaris atrophicans. Arch Dermatol. 1994;130:469–75. [PubMed] [Google Scholar]
- 2.Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711–3. doi: 10.1111/j.1365-2133.1994.tb03406.x. [DOI] [PubMed] [Google Scholar]
- 3.Thomas M, Khopkar US. Keratosis pilaris revisited: Is it more than just a follicular keratosis? Int J Trichology. 2012;4:255–8. doi: 10.4103/0974-7753.111215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panchaprateep R, Tanus A, Tosti A. Clinical, dermoscopic, and histopathologic features of body hair disorders. J Am Acad Dermatol. 2015;72:890–900. doi: 10.1016/j.jaad.2015.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Sallakachart P, Nakjang Y. Keratosis pilaris: A clinico-histopathologic study. J Med Assoc Thai. 1987;70:386–9. [PubMed] [Google Scholar]
- 6.Sonthalia S, Jha AK, Sarkar R, Ankad BS. Disorders of pigmentation. In: Lallas A, Errichetti E, Ioannides D, editors. Dermoscopy in General Dermatology. Boca Raton, FL: CRC Press; 2018. pp. 282–94. [Google Scholar]
- 7.Behera B, Gochhait D, Remya R, Resmi MR, Kumari R, Thappa DM. Follicular psoriasis – dermoscopic features at a glance. Indian J Dermatol Venereol Leprol. 2017;83:702–4. doi: 10.4103/ijdvl.IJDVL_12_17. [DOI] [PubMed] [Google Scholar]
- 8.Ramirez-Fort MK, Khan F, Rosendahl CO, Mercer SE, Shim-Chang H, Levitt JO. Acquired perforating dermatosis: A clinical and dermatoscopic correlation. Dermatol Online J. 2013;19:18958. [PubMed] [Google Scholar]
- 9.López-Gómez A, Vera-Casaño Á, Gómez-Moyano E, Salas-García T, Dorado-Fernández M, Hernández-Gil-Sánchez J, et al. Dermoscopy of circumscribed juvenile pityriasis rubra pilaris. J Am Acad Dermatol. 2015;72(Suppl 1):S58–9. doi: 10.1016/j.jaad.2014.07.053. [DOI] [PubMed] [Google Scholar]
- 10.Jakhar D, Kaur I, Chaudhary R. Dermoscopy of pityrosporum folliculitis. J Am Acad Dermatol. 2018 doi: 10.1016/j.jaad.2018.08.057. doi: 10.1016/j.jaad.2018.08.057. [DOI] [PubMed] [Google Scholar]


