Abstract
Background
To determine whether telemedicine improves access to outpatient neurology care for underserved patients, we compared appointment completion between urban, in-person clinics and telemedicine clinics held in rural and underserved communities where neurology consultations are provided remotely.
Methods
In this retrospective study, we identified patients scheduled for outpatient care from UCDH pediatric neurologists between January 1, 2009, and July 31, 2017, in person and by telemedicine. Demographic and clinical variables were abstracted from electronic medical records. We evaluated the association between consultation modality and visit completion in overall and matched samples using hierarchical multivariable logistic regression.
Results
We analyzed 13,311 in-person appointments by 3,831 patients and 1,158 telemedicine appointments by 381 patients. The average travel time to the site of care was 45.8 ± 52.1 minutes for the in-person cohort and 22.3 ± 22.7 minutes for the telemedicine cohort. Telemedicine sites were located at an average travel time of 217.1 ± 114.8 minutes from UCDH. Telemedicine patients were more likely to have nonprivate insurance, lower education, and lower household income. They had different diagnoses and fewer complex chronic conditions. Telemedicine visits were more likely to be completed than either “cancelled” or missed (“no show”) compared with in-person visits (OR 1.57, 95% CI: 1.34–1.83; OR 1.66, 95% CI: 1.31–2.10 matched on travel time to the site of care; OR 2.22, 95% CI: 1.66–2.98 matched on travel time to UCDH).
Conclusions
The use of telemedicine for outpatient pediatric neurology visits has high odds of completion and can serve as an equal adjunct to in-person clinic visits.
Among all medical specialties, neurology has one of the highest shortages of specialists.1 A recent study estimated that an additional 10% of adult neurologists and 20% of pediatric neurologists are needed to fully meet current clinical needs.1 This shortage is projected to persist or worsen in the coming decade.1 For children living in rural communities, access is even more difficult, given the regionalization of pediatric subspecialty care to urban areas.2–5 As a result, rural children with neurologic disorders and their families frequently travel long distances to obtain needed subspecialty care. Hardships associated with travel—including missed work, missed school, and high transportation costs—often result in patients failing to complete their scheduled medical appointments.5–8 Inconsistent subspecialty care, in turn, can result in poorer health outcomes and extra visits to the emergency department (ED) or preventable hospitalizations.9–12
Real-time telemedicine consultations reduce the time and financial burden of subspecialty visits for rural families and may thereby improve visit completion rates and pediatric neurologist access in underserved communities.6,13 UC Davis Hospital (UCDH) has been providing pediatric neurology services through telemedicine to medically underserved communities in California since 2009. To better understand the effect of this program on access to pediatric neurology care, we compared visit completion between the remote telemedicine clinics and the on-site, in-person clinics. We hypothesized that patients would be equally or more likely to complete appointments scheduled over telemedicine as compared to the appointments scheduled in the in-person clinics, after adjusting for clinical and demographic differences.
Methods
Telemedicine visits
Since 2009, the Division of Pediatric Neurology at UCDH has completed more than 1,200 visits with patients in underserved and rural communities over telemedicine. Telemedicine consultations are offered for new and follow-up appointments at 15 remote sites, primarily located in northern California (figure e-1, links.lww.com/CPJ/A92). Remote clinic staff and primary care providers collect each patient's vitals and history, perform and report a detailed physical examination, and discuss visit recommendations together with the patient and subspecialist. Laboratory test results (such as electroencephalography) and neurologic imaging (such as CT or MRI) are faxed, mailed, or shared over picture archiving and communication systems to the pediatric neurologist either before or during the appointment. Live videoconferencing is conducted over turnkey telemedicine codecs with full UCDH provider access to remote pan-tilt-zoom capabilities. The pediatric neurologist then documents the consultation note within UCDH's electronic health record (EHR) system, and this note is either electronically shared or faxed to the remote clinic site.
Study population
The study population consisted of patients aged 18 years and younger whose registered home addresses were within California and who completed at least 1 visit with a UCDH pediatric neurologist between January 1, 2009, and July 31, 2017, either in person or over telemedicine. Visits included in the analysis were those scheduled between January 1, 2009, and the date that the patient turned 19 years old or July 31, 2017, whichever occurred first. We did not include patients who were scheduled but never seen.
Data source and variables
We abstracted demographic variables (age, sex, and insurance status), patient and telemedicine clinic addresses, dates and completion status of scheduled appointments, and presenting encounter diagnoses from the UCDH EHR system. Sex, insurance status, and patient addresses were assumed to stay constant throughout the study period, and their values were designated as those recorded in the electronic medical record at the time of the data pull. Insurance status was dichotomized into private (commercial employer based) and nonprivate, which included public insurance (e.g., Medicaid and managed Medicaid), self-pay, and no insurance. Addresses were geocoded and mapped to US census tracts. Aggregate census tract information was used to assign patients' neighborhood median household income and education level (defined as the proportion of residents with a bachelor's degree or higher) using the 2016 American Community Survey's 5-year estimates.14 We categorized the median household income as <$35,000, $35,000–$45,000, $45,000–$60,000, and >$60,000. We categorized education level as <10%, 10%–15%, 15%–20%, and >20% college-educated residents. Both variables were categorized into quartiles, which were modified to ensure that the highest and lowest categories included a sufficient number of observations in both comparison groups for analysis. Geocoded addresses were also used to estimate patients' travel times to UCDH (i.e., the time needed to travel from the patient's home and UCDH) and patients' travel time to the site of care (i.e., the time needed to travel from the patient's home to the remote outpatient clinic for telemedicine visits and UCDH for the in-person visits). Travel times were estimated using a proprietary geolocation application programming interface to compute the travel distance and travel time between the 2 points defined by their geographical coordinates, assuming motor vehicle speeds under standard traffic conditions.15
ICD-9-CM codes for the primary presenting diagnosis were used to determine the presence of a pediatric complex chronic condition using a previously validated algorithm.16 We also combined the patients' presenting encounter diagnoses into broad clinical categories for comparison between the cohorts. For a missing diagnosis code—and corresponding diagnosis category and complex chronic condition status—resulting from a canceled or no-show visit, we used the nonmissing values from the patient's previous or following completed appointment, whichever was temporally closer. The primary dependent variable in our analysis was completion of scheduled visits, with cancellations and no shows considered to be uncompleted visits. The primary independent variable was whether the appointment was scheduled in a telemedicine or in-person clinic.
Statistical analysis
Simple descriptive statistics were used to characterize study variables. Univariable and bivariable comparisons were conducted using Student t tests, Pearson χ2 tests, and Wilcoxon rank-sum tests, as appropriate. The odds of visit completion for visits scheduled over telemedicine compared with those scheduled in person were estimated using logistic regression with random intercepts for patients to account for patient-level correlations between scheduled appointments. Multivariable logistic regression models were adjusted for various potential confounders including patient's age, travel time to the site of care, insurance status, median household income, education level, year of visit, and the presence of a complex chronic condition. The confounders were chosen for inclusion in the model based on associations observed in the descriptive analysis and a priori, based on our hypotheses. We also evaluated adjusted odds ratios for each presenting diagnosis category to determine whether visit completion by consultation modality varied by the patient's diagnosis.
To check the robustness of our findings, we evaluated visit completion in matched subsets of the study population. First, telemedicine and in-person cohorts were matched on travel time to the site of care using a caliper of 5 minutes in a 1:1 ratio (without replacement) to compare cohorts with similar, convenient access to pediatric neurologists. Second, we matched the cohorts on travel time to UCDH using the same methodology as above to compare visit completion among distant communities with and without telemedicine clinics. We then evaluated the adjusted odds of visit completion in both the time to site of care–matched and time to UCDH–matched samples. All analyses were performed using Stata/SE version 15.1 (College Station, TX). p Values <0.05 were considered to be statistically significant.
Standard protocol approvals, registrations, and patient consents
The Institutional Review Board at UCDH approved this study and granted a Health Insurance Portability and Accountability Act waiver of research participant's authorization.
Data availability
Any data not published within the article will be shared in a deidentified form by request from any qualified investigator.
Results
A total of 14,469 appointments scheduled with UCDH pediatric neurology between January 1, 2009, and July 31, 2017, were included in the study. Of these, 1,158 appointments were scheduled in the telemedicine clinics by 381 patients, and 13,311 appointments were scheduled in the in-person clinic by 3,831 patients. Thirty-nine patients scheduled appointments in both telemedicine and in-person clinics. Telemedicine consultation sites (figure e-1, links.lww.com/CPJ/A92) were located at an average travel time of 217.1 minutes (SD 114.8 minutes) from UCDH.
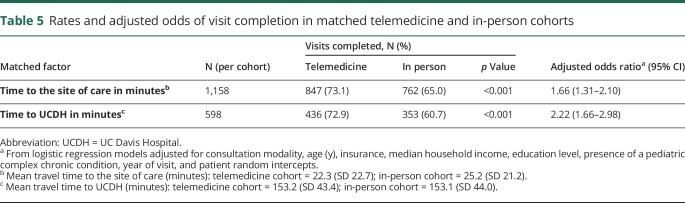
As shown in table 1, patient visits scheduled in the telemedicine and in-person clinics had comparable age and sex distributions. Patients in the telemedicine cohort, however, were less likely to have private insurance compared with patients in the in-person cohort (2.1% vs 34.5%, p < 0.001). The mean travel time to the site of care was 22.3 minutes (SD 22.7 minutes) for the telemedicine cohort and 45.8 minutes (SD 52.1 minutes) for the in-person cohort (p < 0.001). In contrast, the travel time to UCDH (location of the in-person clinic) was 157 minutes (SD 33.2 minutes) for the telemedicine cohort, assuming no change in the number of visits scheduled. Patients in the telemedicine cohort were more likely to live in census tracts with a lower median household income (90.4% vs 46.3% with income ≤ $60,000) and lower education level (69.2% vs 34.9% with ≤20% college graduates).
Table 1.
Baseline characteristics of the telemedicine and in-person cohorts
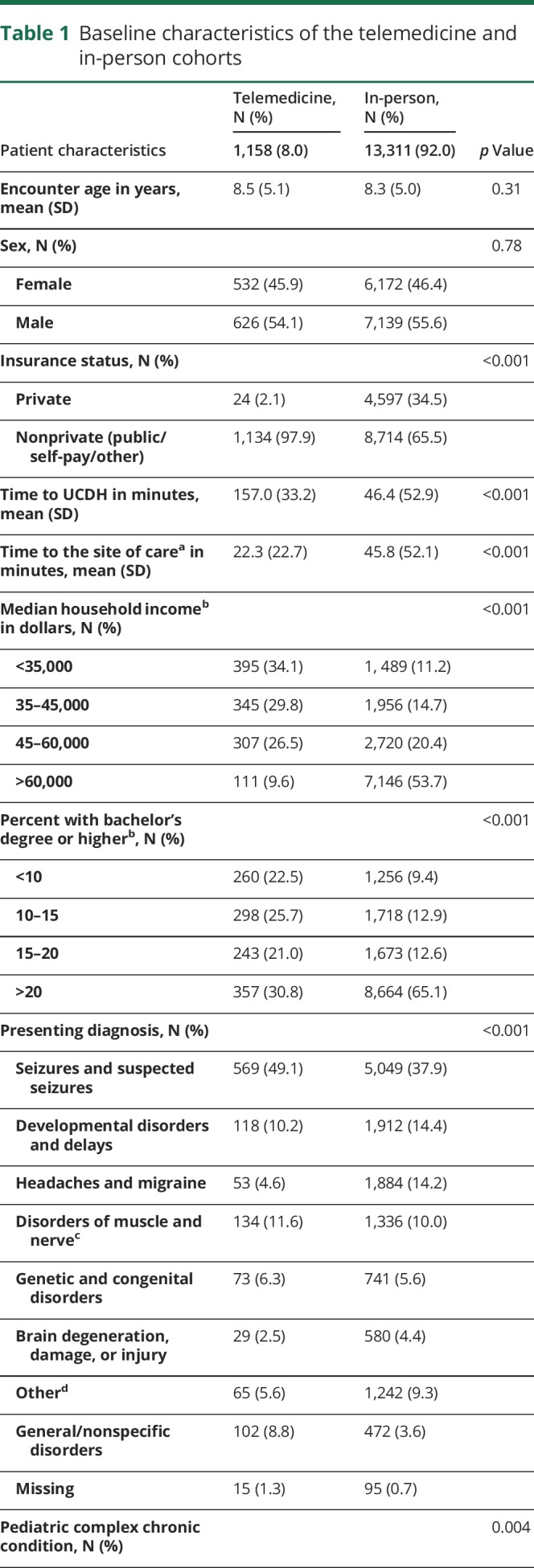
In terms of clinical characteristics, children scheduled in the telemedicine clinics were slightly less likely to have a complex chronic condition than those scheduled in the in-person clinics (11.5% vs 14.2%, p = 0.004, table 1). Seizure disorders and developmental delays were the most common primary presenting diagnoses in both clinics (table 1). Seventy-three percent of telemedicine appointments and 65.1% of in-person appointments were completed as scheduled (p < 0.001, table1). Comparison of patient-level characteristics is shown in table e-1 (links.lww.com/CPJ/A93).
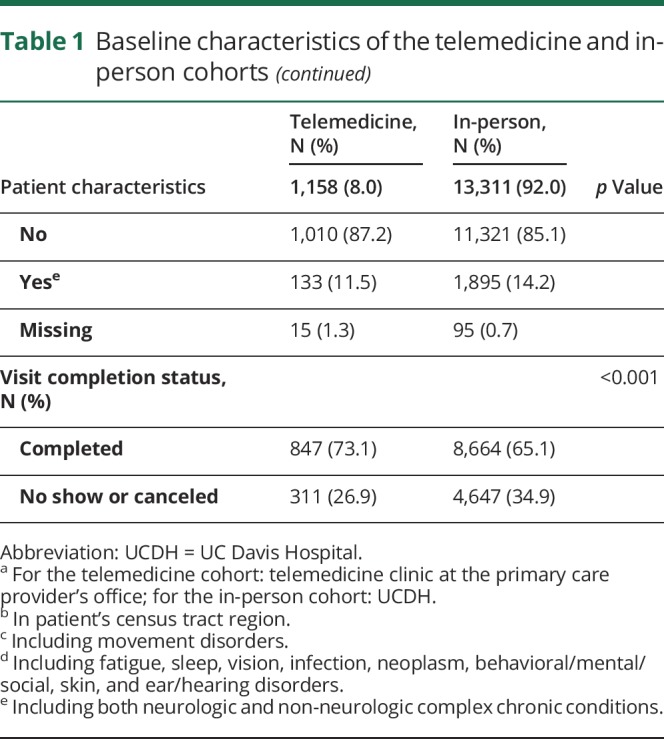
As shown in table 2, the bivariable odds of visit completion were higher for telemedicine compared with in-person visits (OR 1.46, 95% CI: 1.27–1.68). Visit completion odds decreased by 7% (95% CI: 3%–11%) with a 1-hour increase in travel time to the site of care. Patients from neighborhoods with higher education (≥15% college graduates) had higher odds of visit completion than patients from neighborhoods with lower education (<10% college graduates).
Table 2.
Bivariable/unadjusted odds of visit completion with patient random intercepts
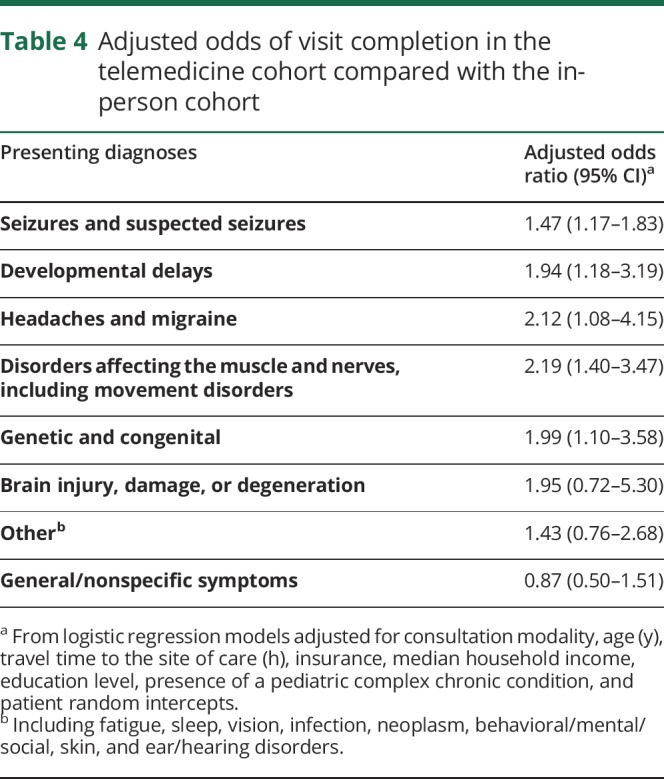
In the adjusted analysis (table 3), there were higher odds of visit completion in the telemedicine cohort compared with the in-person cohort (adjusted odds ratio, aOR: 1.57, 95% CI: 1.34–1.83). Visit completion was inversely associated with encounter age (2% lower odds for a 1-year increase in age, 95% CI: 1%–3%) and travel time to the site of care (6% lower odds for a 1-hour increase in travel time, 95% CI: 1%–10%). Adjusted visit completion odds were higher for patients residing in neighborhoods with 15%–20% college graduates compared with those with <10% college graduates (aOR: 1.22, 95% CI: 1.03–1.44). As shown in table 4, the adjusted odds of visit completion were significantly higher for the telemedicine cohort compared with the in-person cohort within all major presenting diagnosis categories.
Table 3.
Multivariable odds of visit completion with patient random intercepts
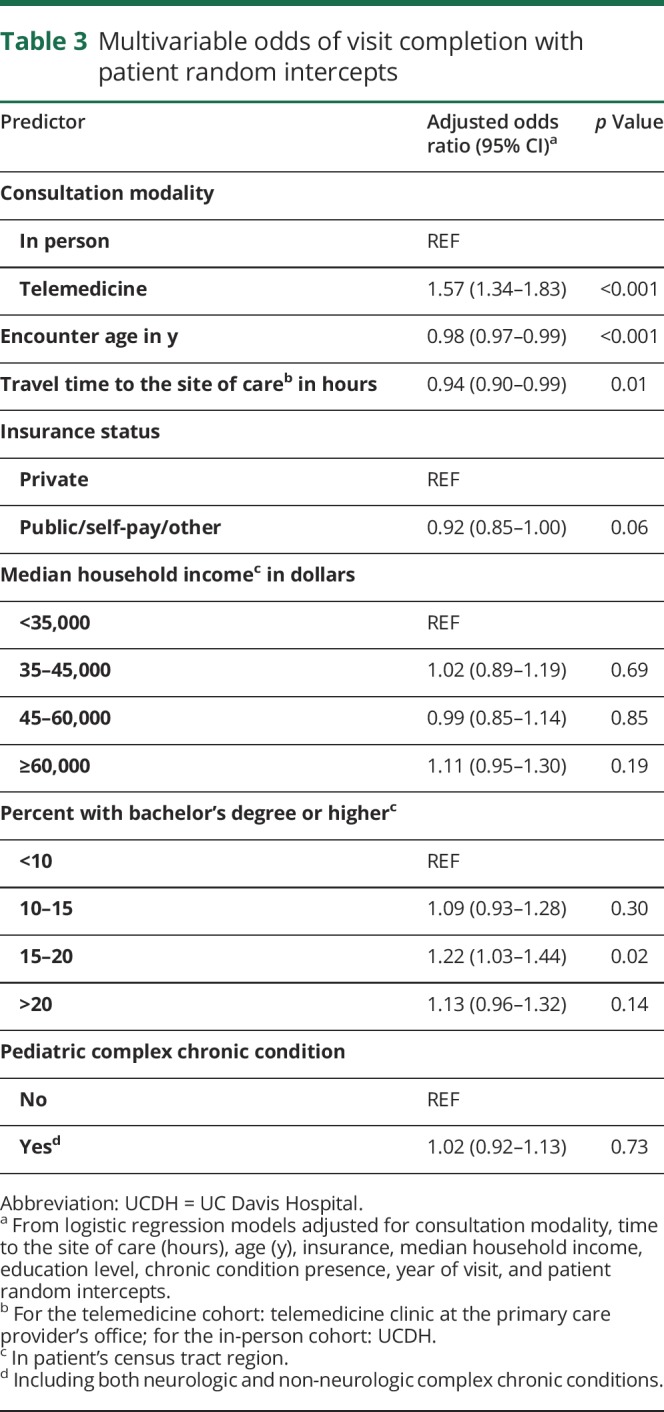
Table 4.
Adjusted odds of visit completion in the telemedicine cohort compared with the in-person cohort
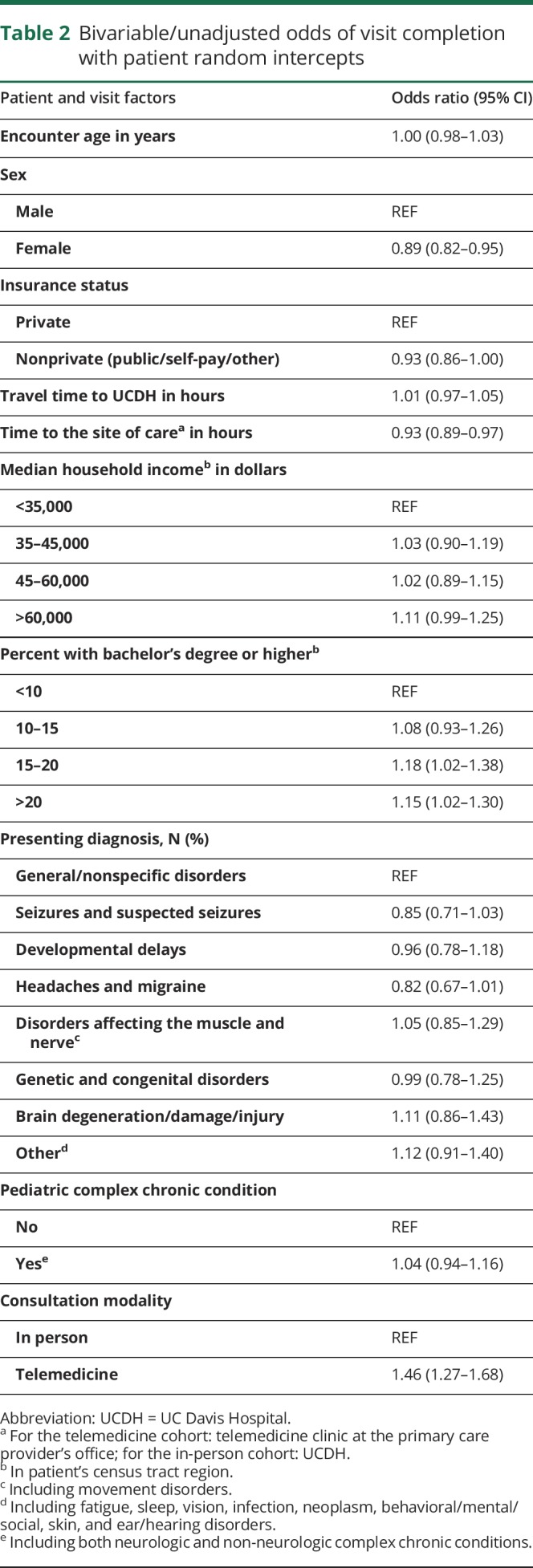
As shown in table 5, the time to site of care–matched sample comprised 1,158 visits in each cohort. Seventy-three percent of telemedicine visits and 65.0% of in-person visits were completed in this sample (p < 0.001), and the adjusted odds of visit completion were higher for the telemedicine cohort compared with the in-person cohort (aOR 1.66, 95% CI: 1.31–2.10). The time to UCDH-matched sample included 598 visits in each cohort. Seventy-three percent of telemedicine visits and 60.7% in-person visits were completed (p < 0.001). Similar to previous analysis, the adjusted odds of visit completion were higher for the telemedicine cohort (aOR 2.22, 95% CI: 1.66–2.98).
Table 5.
Rates and adjusted odds of visit completion in matched telemedicine and in-person cohorts
Discussion
In this retrospective analysis, we found that children completed 73% of their scheduled neurology appointments in the telemedicine clinics and 65% of their scheduled appointments in the traditional in-person clinics of a large, academic, tertiary care hospital. Even after adjusting for potential confounders including travel time to the site of care, we found the odds of visit completion to be 57% higher in the telemedicine clinics than the in-person clinics.
Of the 33 counties, which comprise UCDH's service area, 26 do not have a pediatric neurologist,17 and all 18 pediatric neurologists in this region practice in urban areas.18 Thus, outpatient pediatric neurology services are an unmet need in the rural and remote areas of this region. In addition, our study shows that compared with the patients served by in-person clinics, those served by the telemedicine clinics have lower education and household incomes. The combination of poor local access and socioeconomic factors might result in patients' inability to obtain needed neurology care in the traditional in-person clinics and lower their visit completion rates. In our study, we found that the adjusted odds of completion were higher among telemedicine compared with in-person visits, even in the time to UCDH-matched analysis. This shows that providing neurology consultations through telemedicine in distant communities may serve as an equal adjunct to in-person visits and may reduce disparities in visit completion.
Our results of higher visit completion in the telemedicine clinics concur with previous studies of outpatient telemedicine. One study reported that psychiatry patients were more likely to complete telemedicine visits than usual care visits.19 Another study showed that adult patients with Parkinson disease had a high completion rate of virtual house calls that supplemented usual care.20 A pilot study among children with nonacute headaches also found higher adherence in telemedicine clinics compared with in-person clinics.21
Improvement in visit completion by reducing patients' travel distance has also been demonstrated in community-based satellite clinics.8 In addition, the use of in-home telemedicine for providing care to children with medical complexity and adult patients with multiple sclerosis/neuroimmunologic conditions and Parkinson disease has been shown to be feasible, convenient, and effective.20,22–25 However, we found visit completion to be higher in the telemedicine cohort even after restricting the sample to patients with shorter travel times to the site of care. This finding shows that factors in addition to travel-related convenience contributed to the higher completion rates of telemedicine appointments. These may include patient- and family-centered factors such as familiarity with the remote clinic location, ease of scheduling neurology consultations with the primary care clinic, and/or greater accountability on the part of the child's caregivers due to some degree of integration between the primary care and subspecialist services. The need for care coordination tends to be higher for children with epilepsy and seizure disorders because they often have developmental and mental health comorbidities and functional limitations,26,27 making their treatment more appropriate for team-based care. In the model of care delivery through telemedicine, better care coordination between the child's primary care provider and neurologist facilitates exchange of important health information between the providers and parents, and broadens the primary care provider's knowledge about management of the patient's neurologic condition. Moving the system of care closer to a patient's “medical home” may increase parents' comfort and satisfaction with the care process, making them more adherent to their children's scheduled care regimen.28
Although this study did not evaluate the quality or outcomes of care provided by telemedicine, others find telemedicine to be suitable for providing neurologic specialty care.2,29 Several previously published studies have found comparable or higher patient and/or provider satisfaction with telemedicine visits for neurologic conditions compared with in-person care.21,30–35 Studies also suggest that the care provided using telemedicine is equivalent in terms of efficacy to in-person care3,20,21,24,27,30,32,36; however, the current evidence is not strong.37 In our experience, many neurologic conditions are amenable to medical consultation over telemedicine, especially when a trained clinician is available at the remote site to assist with examinations. The continued use of telemedicine by some of our sites since the program's inception illustrates that this model of care is agreeable to both patients and providers on a long-term basis.
This study has limitations. First, there are inherent differences between the cohorts because patients were not randomized to telemedicine or in-person visits. However, we attempted to address this limitation using a multivariable model to adjust for potential confounders. In addition to demographic differences, there were also clinical differences between the cohorts—such as distribution of primary diagnoses—that could potentially affect care-seeking behavior. However, the adjusted odds of visit completion were significantly higher in the telemedicine clinics for a majority of diagnostic categories including seizures disorders, headaches, developmental delays, disorders affecting the muscle and nerves, and genetic and congenital disorders. This demonstrates that the effect of telemedicine on visit completion is consistent across many diagnoses. Second, because of the use of structured data elements and the study's retrospective nature, we assumed no changes in insurance status, home address, and did not have information on confounders such as the availability of transportation or whether the child's symptoms persisted at the time of the appointment. In addition, there could be differences in important baseline characteristics, such as parents' overall health consciousness, which would affect visit completion. However, by incorporating patient-level random effects into our model, we have accounted for patients' and families' baseline propensity to complete scheduled appointments to some extent. Finally, this study evaluated a subspecialty telemedicine program at a large academic center, and these results may not be generalizable to other telemedicine programs, which might vary in delivery models (consultative vs direct care), populations served (adults vs children), clinical services offered (primary care vs subspecialty), and goal targeted (expanded access vs lower wait times). Last, we focused on completion of scheduled visits and thus excluded patients who were referred but not scheduled. We did not include patients who were scheduled to see pediatric neurologists but failed to successfully complete a single visit. Of note, there were no differences in the proportion of such patients between the cohorts and not including them did not change the difference in appointment adherence rates between the cohorts (tables e-2 and e-3, links.lww.com/CPJ/A93).
The study also has a number of strengths. First, our comparison groups were well balanced across age and sex. Second, the multivariable model includes many factors found predictive of appointment noncompletion in previous studies, such as travel time to the site of care and socioeconomic factors,7 and the results of this model appear robust with matched analyses. Last, this study comparing appointment completion rates in telemedicine and in-person pediatric neurology clinics adds to the limited but growing pool of studies evaluating the effectiveness of subspecialty telemedicine care for children.21,38–40
The low density and urban clustering of pediatric neurologists in UCDH's service area and nationwide have made it necessary to find ways by which providers can extend services within existing time and resource constraints. Telemedicine is one solution that can improve access by offering greater flexibility to patients and providers. By improving subspecialist availability and enhancing care coordination, telemedicine may reduce disparities in patients' receipt of necessary care and may improve the quality of life for patients and their caregivers in rural and underserved communities.
Appendix. Authors
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Dall TM, Storm MV, Chakrabarti R, et al. . Supply and demand analysis of the current and future US neurology workforce. Neurology 2013;81:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timpano F, Bonanno L, Bramanti A, et al. . Tele-Health and neurology: what is possible? Neurol Sci 2013;34:2263–2270. [DOI] [PubMed] [Google Scholar]
- 3.Davis LE, Coleman J, Harnar J, King MK. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health 2014;20:473–477. [DOI] [PubMed] [Google Scholar]
- 4.Kang PB, Bale JF Jr, Mintz M, et al. . The child neurology clinical workforce in 2015: report of the AAP/CNS Joint Taskforce. Neurology 2016;87:1384–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velasquez SE, Chaves-Carballo E, Nelson EL. Pediatric teleneurology: a model of epilepsy care for rural populations. Pediatr Neurol 2016;64:32–37. [DOI] [PubMed] [Google Scholar]
- 6.Bashiri M, Greenfield LJ Jr, Oliveto A. Telemedicine interest for routine follow-up care among neurology patients in Arkansas. Telemed J E Health 2016;22:514–518. [DOI] [PubMed] [Google Scholar]
- 7.Dantas LF, Fleck JL, Cyrino Oliveira FL, Hamacher S. No-shows in appointment scheduling—a systematic literature review. Health Policy 2018;122:412–421. [DOI] [PubMed] [Google Scholar]
- 8.McLeod H, Heath G, Cameron E, Debelle G, Cummins C. Introducing consultant outpatient clinics to community settings to improve access to paediatrics: an observational impact study. BMJ Qual Saf 2015;24:377–384. [DOI] [PubMed] [Google Scholar]
- 9.Patel AD. Variables associated with emergency department and/or unplanned hospital utilization for children with epilepsy. Epilepsy Behav 2014;31:172–175. [DOI] [PubMed] [Google Scholar]
- 10.Patel AD, Wood EG, Cohen DM. Reduced emergency department utilization by patients with epilepsy using QI methodology. Pediatrics 2017;139:e20152358. [DOI] [PubMed] [Google Scholar]
- 11.Patel AD, Terry D, Moore JP, et al. . Reduction of emergency department visits using an urgent clinic for children with established epilepsy. Neurol Clin Pract 2016;6:480–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nourazari S, Hoch DB, Capawanna S, Sipahi R, Benneyan JC. Can improved specialty access moderate emergency department overuse? Effect of neurology appointment delays on ED visits. Neurol Clin Pract 2016;6:498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams JL, George BP, Dorsey ER. Neurologic care … anytime? Neurol Clin Pract 2016;6:472–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American fact finder. In: series. American fact finder. Available at: factfinder.census.gov/faces/nav/jsf/pages/download_center.xhtml. Accessed August 21, 2017.
- 15.Weber S and Péclat M. A simple command to calculate travel distance and travel time. Stata Journal 2017;17:962–971. [Google Scholar]
- 16.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Health Workforce Mapper. In: series. Health workforce mapper. Available at: ama-assn.org/about-us/health-workforce-mapper. Accessed July 20, 2018.
- 18.California medical service study areas (MSSA) frontier, rural and urban defined areas. In: series. California medical service study areas (MSSA) frontier, rural and urban defined areas. Available at: oshpd.ca.gov/documents/HWDD/GIS/RuralMSSAv3.pdf. Accessed July 20, 2018.
- 19.Leigh H, Cruz H, Mallios R. Telepsychiatry appointments in a continuing care setting: kept, cancelled and no-shows. J Telemed Telecare 2009;15:286–289. [DOI] [PubMed] [Google Scholar]
- 20.Beck CA, Beran DB, Biglan KM, et al. . National randomized controlled trial of virtual house calls for Parkinson disease. Neurology 2017;89:1152–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vierhile A, Tuttle J, Adams H, tenHoopen C, Baylor E. Feasibility of providing pediatric neurology telemedicine care to youth with headache. J Pediatr Health Care 2018;32:500–506. [DOI] [PubMed] [Google Scholar]
- 22.Bove R, Garcha P, Bevan CJ, Crabtree-Hartman E, Green AJ, Gelfand JM. Clinic to in-home telemedicine reduces barriers to care for patients with MS or other neuroimmunologic conditions. Neurol Neuroimmunol Neuroinflamm 2018;5:e505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bove R, Bevan C, Crabtree E, et al. . Toward a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Mult Scler 2018. [DOI] [PubMed] [Google Scholar]
- 24.Dorsey ER, Venkataraman V, Grana MJ, et al. . Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol 2013;70:565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Notario PM, Gentile E, Amidon M, Angst D, Lefaiver C, Webster K. Home-based telemedicine for children with medical complexity. Telemed J E Health 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics 2012;129:256–264. [DOI] [PubMed] [Google Scholar]
- 27.Rasmusson KA, Hartshorn JC. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia 2005;46:767–770. [DOI] [PubMed] [Google Scholar]
- 28.Herendeen N, Deshpande P. Telemedicine and the patient-centered medical home. Pediatr Ann 2014;43:e28–e32. [DOI] [PubMed] [Google Scholar]
- 29.Joshi C. Telemedicine in pediatric neurology. Pediatr Neurol 2014;51:189–191. [DOI] [PubMed] [Google Scholar]
- 30.Duncan C, Dorrian C, Crowley P, Coleman R, Patterson V. Safety and effectiveness of telemedicine for neurology outpatients. Scott Med J 2010;55:3–5. [DOI] [PubMed] [Google Scholar]
- 31.Müller KI, Alstadhaug KB, Bekkelund SI. Headache patients' satisfaction with telemedicine: a 12-month follow-up randomized non-inferiority trial. Eur J Neurol 2017;24:807–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Müller KI, Alstadhaug KB, Bekkelund SI. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J Med Internet Res 2016;18:e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qubty W, Patniyot I, Gelfand A. Telemedicine in a pediatric headache clinic: a prospective survey. Neurology 2018;90:e1702–e1705. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed SN, Mann C, Sinclair DB, et al. . Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient's perspective. Epilepsia 2008;49:573–585. [DOI] [PubMed] [Google Scholar]
- 35.Davis LE, Harnar J, LaChey-Barbee LA, Richardson SP, Fraser A, King MK. Using teleneurology to deliver chronic neurologic care to rural veterans: analysis of the first 1,100 patient visits. Telemed J E Health 2018. [DOI] [PubMed] [Google Scholar]
- 36.Chua R, Craig J, Esmonde T, Wootton R, Patterson V. Telemedicine for new neurological outpatients: putting a randomized controlled trial in the context of everyday practice. J Telemed Telecare 2002;8:270–273. [DOI] [PubMed] [Google Scholar]
- 37.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol 2015;72:349–354. [DOI] [PubMed] [Google Scholar]
- 38.Dayal P, Hojman NM, Kissee JL, et al. . Impact of telemedicine on severity of illness and outcomes among children transferred from referring emergency departments to a children's hospital PICU. Pediatr Crit Care Med 2016;17:516–521. [DOI] [PubMed] [Google Scholar]
- 39.Sauers-Ford HS, Marcin JP, Underwood MA, et al. . The use of telemedicine to address disparities in access to specialist care for neonates. Telemed J E Health 2018. [DOI] [PubMed] [Google Scholar]
- 40.Wood CL, Clements SA, McFann K, Slover R, Thomas JF, Wadwa RP. Use of telemedicine to improve adherence to American diabetes association standards in pediatric type 1 diabetes. Diabetes Technol Ther 2016;18:7–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Any data not published within the article will be shared in a deidentified form by request from any qualified investigator.