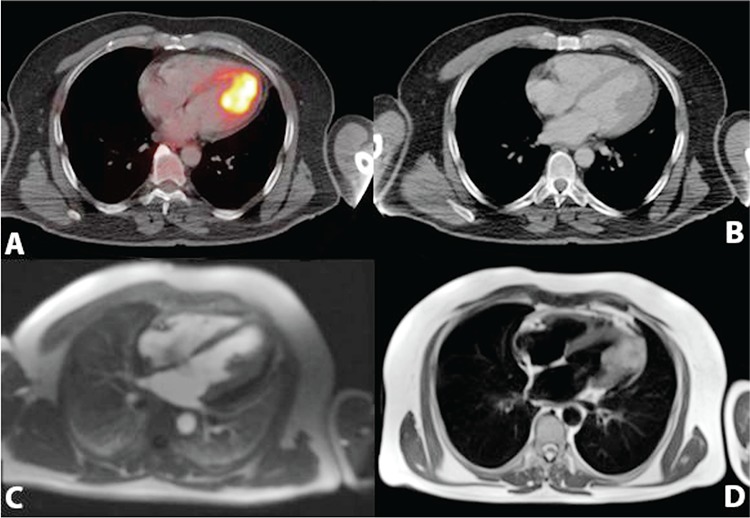
Figure 1.
A 58-year old patient with a history of malign melanoma was referred to our PET/CT department for re-staging. Patient was initially diagnosed with excisional biopsy from the nail bed of his first left toe 4 years ago. Inguinal lymph node biopsy revealed negative for metastases at the time of diagnosis. Metastatic lymph nodes were detected in left inguinal region which was confirmed with biopsy 3 years later. Patient was under immunotherapy and had no symptoms either in the control or in the day of scan.
PET/CT scan demonstrated increased cardiac (18F-FDG) 18-fluoro-deoxy-glucose uptake in left ventricule (A). CT images revealed filling defect of the intravenous contrast in left ventricular cavity which was suggestive of a lesion or a benign pathology like papillary muscle hypertrophy (B). MRI scan showed T1 hyperintensity with gadolinium enhancement in late phase of contrast giving process, 4x3 cm sized T2 hypointensity compatible with melanoma metastasis starting from papillary muscle in apical region, infiltrating through myocardium and extending to pericardium (C, D). Biopsy could not be performed from cardiac mass due to high mortality risk of the patient.
Cardiac masses are mostly originated from metastatic spread. Lung cancer, breast cancer and non-hodgkin lymphoma are the most common origins for cardiac metastases (1,2). Malign melanoma has also high potential to metastasize especially to lungs, liver and bones. However, cardiac metastases from melanoma are oftenly detected in autopsy series rather than detected with clinical presentation (3).18F-FDG uptake could vary in cardiac tissue and it is usually shown to be helpful in differentiating benign lesions from malignancy (4). In addition to this high uptake in myocardium and the left ventricule can be observed physiologically in 18F-FDG PET images (5). Papillary muscle hypertrophy or trombus in ventriculary cavity could show increased 18F-FDG uptake in PET images (6,7). As seen in our case, cardiac uptake should be checked carefully to differentiate physiological uptake which could be normally seen in cardiac tissue. Diversely, intravenous contrast is not routinely used in every PET/CT scan protocol. It has been proven to be helpful in identifying pathologic changes in organs with normal findings in unenhanced CT (8). Our images also demonstrated the usage of intravenous contrast with the filling defect seen in left ventricular cavity.
