Abstract
Introduction
There is a long history of pre-deployment PTSD prevention efforts in the military and effective pre-deployment strategies to prevent post-deployment PTSD are still needed.
Materials and Methods
This randomized controlled trial included three arms: heart rate variability biofeedback (HRVB), cognitive bias modification for interpretation (CBM-I), and control. The hypothesis was that pre-deployment resilience training would result in lower post-deployment PTSD symptoms compared with control. Army National Guard soldiers (n = 342) were enrolled in the Warriors Achieving Resilience (WAR) study and analyzed. The outcome was PTSD symptom severity using the PTSD Checklist – Military version (PCL) measured at pre-deployment, 3- and 12-month post-deployment. Due to the repeated measures for each participant and cluster randomization at the company level, generalized linear mixed models were used for the analysis. This study was approved by the Army Human Research Protection Office, Central Arkansas Veterans Healthcare System Institutional Review Board (IRB), and Southeast Louisiana Veterans Health Care System IRB.
Results
Overall, there was no significant intervention effect. However, there were significant intervention effects for subgroups of soldiers. For example, at 3-months post-deployment, the HRVB arm had significantly lower PCL scores than the control arm for soldiers with no previous combat zone exposure who were age 30 and older and for soldiers with previous combat zone exposure who were 45 and older (unadjusted effect size −0.97 and −1.03, respectively). A significant difference between the CBM-I and control arms was found for soldiers without previous combat zone exposure between ages 23 and 42 (unadjusted effect size −0.41). Similarly, at 12-months post-deployment, the HRVB arm had significantly lower PCL scores in older soldiers.
Conclusion
Pre-deployment resilience training was acceptable and feasible and resulted in lower post-deployment PTSD symptom scores in subgroups of older soldiers compared with controls. Strengths of the study included cluster randomization at the company level, use of iPod device to deliver the resilience intervention throughout the deployment cycle, and minimal disruption of pre-deployment training by using self-paced resilience training. Weaknesses included self-report app use, study personnel not able to contact soldiers during deployment, and in general a low level of PTSD symptom severity throughout the study. In future studies, it would important for the study team and/or military personnel implementing the resilience training to be in frequent contact with participants to ensure proper use of the resilience training apps.
Keywords: Post-traumatic stress disorder (PTSD), military, resilience, combat stress, prevention, heart rate variability biofeedback, cognitive bias modification
INTRODUCTION
In a meta-analysis of recent post-deployment post-traumatic stress disorder (PTSD), rates varied from 5.5% to 13.2% indicating the need for effective pre-deployment strategies to prevent post-deployment PTSD.1 Historical pre-deployment PTSD prevention efforts for military personnel have included: recruit screening and selection procedures, assignment of vulnerable individuals to less stressful jobs, stress-inoculation using realistic training, positive leadership, efforts to maintain morale, and operational-stress training.2,3 More recently, the Army implemented a large scale primary prevention program for all soldiers known now as Comprehensive Soldier and Family Fitness (CSF), which includes elements of the Battlemind mental health training program. However, according to a 2014 Institute of Medicine report, the evidence to support current Department of Defense (DoD) primary prevention strategies (including CSF) was low.4
Heart rate variability biofeedback (HRVB) and cognitive bias modification for interpretation (CBM-I) training may be good candidate mechanisms upon which resilience interventions could be developed. There is increasing empirical and theoretical evidence to support the use of HRVB in the treatment of emotional disorders.5 A recent multidimensional model proposed high-frequency HRV (HF) as a transdiagnostic biomarker of self-regulation and cognitive control.6 Lower HRV has been reported in veterans diagnosed with PTSD7 and is associated with psychological distress.8 Higher HRV is associated with positive social interactions.9 Psychological resilience and autonomic flexibility; therefore, enhancing an individual’s capacity to adapt to changing social or environmental demands (situational awareness) and performance on executive-functioning tasks.10,11 HRV also can be improved with biofeedback training12 which is typically achieved by slowing the respiration rate.13 Therefore, HRVB provides a pathway to regulate the stress response and potentially prevent PTSD symptoms.
A growing body of research similarly suggests that CBM training can be used as a resilience-building intervention. While there are varying methods used in CBM training, all techniques seek to modify either attentional or interpretative processes that are causally associated with the development of emotional disorders. Recent investigations have shown that CBM training administered before a stressful event can serve as a “cognitive vaccine,” minimizing negative emotional responses to subsequent stressors.14–16 This research suggests that modification of interpretive style prior to exposure to a traumatic event could decrease negative appraisals of a traumatic event’s meaning and of one’s reaction to traumatic events – which are established causal factors in post-trauma psychopathology – and thus attenuate the development of PTSD.17–19
The primary aim of the present study was to test two novel resilience training interventions, one based on HRVB and one based on CBM-I training among Army National Guard soldiers preparing for deployment to Operation Iraqi Freedom (OIF) combat zones. Briefly, the HRVB intervention identified a breathing frequency that maximized an individual soldier’s HRV and then set a breath-pacing app to that frequency. The CBM-I intervention shifted a soldier’s interpretive style by presenting an increasing proportion of neutral or non-negative interpretations of an ambiguous deployment-related scenario. These interventions were meant to improve physiological and cognitive resilience to the stress of deployment and result in lower levels of post-deployment PTSD symptoms compared with a control group.
METHODS AND MATERIALS
Design
The results reported here are from the Warriors Achieving Resilience (WAR) study that included pre-deployment, 3- and 12-months post-deployment assessments. The resilience interventions included pre-deployment HRVB and CBM-I training and subsequent practice using the respective iPod app with the goal of lower post-deployment PTSD symptom severity compared with controls. A cluster randomization was used where soldiers were randomized at the company level to minimize app sharing across intervention arms. This study was approved by the Army Human Research Protection Office, Central Arkansas Veterans Healthcare System IRB, and Southeast Louisiana Veterans Health Care System IRB.
Participants
Army National Guard soldiers from an Aviation Battalion and an Infantry Battalion preparing to deploy to Iraq in 2011 served as the recruitment pool. The Aviation Battalion deployed in early May 2011 and returned in early December 2011 and the Infantry Battalion deployed in late July 2011 and returned mid-December 2011. The withdrawal of American military forces from Iraq was completed by December 2011.
Inclusion/Exclusion Criteria
Army National Guard soldiers were eligible for the study if they were scheduled to deploy for OIF/OEF operations within the next 12 months, age 18–60, willing to provide the name and phone number of at least one person to help locate the soldier for the follow-up assessments if necessary, and were not taking beta blockers or daytime benzodiazepines. Soldiers were not excluded for taking the following medications: antidepressant (N = 2), stimulant (N = 3), antihypertensive (mostly angiotensin-converting enzyme inhibitor, N = 16). No soldiers reported taking prazosin.
Recruitment and Data Collection Procedures
The study was presented to 1,112 soldiers during a pre-deployment soldier readiness processing (SRP) drill weekend. During the SRP, each soldier was then required to meet privately with a member of the research team who explained the study. Those interested in participating completed a written informed consent process and eligibility screening. The Chain of Command was not informed about whether a soldier was participating in the study. This type of recruitment procedure has also been used to recruit active duty Army soldiers.20 No financial incentives were offered for study participation.
Per the research protocol, 600 soldiers were recruited and consented to participate in this research study during the SRP. Therefore, 54% (600/1,112) of potentially eligible National Guard soldiers completed the consent process. Sample size was determined in terms of a linear regression model predicting PTSD symptom severity and a range of partial correlations for varying number of predictors. With a partial correlation of 0.2, 20 predictors, and alpha = 0.05, a sample size of 500 would result in 78% power.
During the subsequent pre-deployment training, 426/600 (71.0%) completed the pre-deployment assessment (see participant flow diagram in Supplementary material). Of the 426 soldiers, 15 did not deploy and 3 deployed with a different company leaving 408 soldiers eligible for analysis. Sixty-five of these soldiers did not participate in the 3- and 12-month follow-up and 1 was missing PCL scores at both follow-ups and these participants were excluded from further analysis. The final analysis sample size was 342 and included 247/342 (72.2% of analysis sample) soldiers from a Calvary Battalion and 95/342 (27.8% of analysis sample) soldiers from an Aviation Battalion. The 3-month post-deployment follow-up rate was 75.2% (307/408) and 12-month follow-up rate was 57.3% (234/408). Soldiers who completed 3-month follow-up assessment were more likely Caucasian (p = 0.004) and more likely to have some formal education beyond high school (p = 0.004). Soldiers who completed 12-month follow-up were more likely to be higher military rank (p = 0.0003). On average, 3-month post-deployment data were collected at 101 days post-deployment (range = 64–268, SD = 55.0) and 12-month data were collected at 434 days post-deployment (range = 389–638, SD = 47.0).
Resilience Training Interventions
The resilience training interventions included self-paced HRVB or CBM-I training sessions on laptop computers (up to 15 soldiers at a time) followed by a brief individual practice session using the relevant app downloaded onto an iPod Touch device (up to 1-hour total training time). Descriptions of the resilience training interventions and the HRV and Cognitive Bias Recognition Test assessments are available in Supplementary material. Additional app practice was suggested at least three times per week even if only for a few minutes a day and before or after stressful events (e.g., before or after going on patrol or convoy).
The HRVB training used an Institute of HeartMath emWave earlobe sensor device and software to detect heart rhythm and calculate HRV and inform game-based HRV training where a series of progressively more challenging games were controlled by the user’s HRV. The sampling rate for the earlobe sensor was 370 Hz and used an infrared pulse plethysmograph to detect the pulse wave. The game-based training was designed to increase engagement and utilization of resilience-building skills. The iPod app was BreathPacer by Larva Labs Ltd. The BreathPacer app was available on iTunes and was modified for this study by adding a date/time stamp to record when the app was opened and closed. The breathing frequency that maximized a participant’s HRV was identified during the laptop training and then used as the target breathing frequency for the BreathPacer app.
The CBM-I training developed for this study was based on established procedures that have been shown to modify interpretations about ambiguous events.21 Briefly, participants in the CBM-I arm received self-paced laptop-based training using iMAT (Mental Armor Training) software which presented a series of deployment-related scenarios (2–3 sentences) which were ambiguous with regard to their emotional meaning until the last word. Each scenario presented the last word as a word fragment. The participant was asked to complete the word fragment which over time increased the proportion of neutral or non-negative interpretations of the scenario. Note that this intervention was not designed to modify attention to prospective combat threats. Rather, the aims of the intervention were to promote less negative appraisal of post-event retrospections. A similar iMAT app was loaded onto an iPod. Participants were encouraged to use the iMAT app at least three times per week.
Control Arm
Soldiers randomized to the control arm did not receive any additional resilience training. Soldiers in the control arm did receive an iPod but none of the resilience training apps described above were loaded on the control iPods.
Measures
Pre-and post-deployment data collection included: sociodemographics, military demographics, current tobacco use, mental health symptoms, heart rate variability, and negative cognitive bias. Sociodemographic variables included age, gender, race/ethnicity, education, and marital status. Race/ethnicity was self-reported according to the following categories: American Indian or Alaskan Native; Asian/Oriental or Pacific Islander; Black/African American; White/Caucasian, not of Hispanic origin; Hispanic, or Other. This variable was dichotomized due to the majority being White/Caucasian. Childhood abuse was defined as childhood physical or sexual abuse using the Pre-Deployment Life Events scale from the Deployment Risk and Resilience Inventory (DRRI).22 Military variables included rank, years of active service, years of total service, number of deployments, deployment to combat zone, deployment-related traumatic brain injury (TBI) prior to or during most recent deployment, and combat experiences during the most recent deployment. Pre- and post-deployment TBI were assessed using the DoD Post-Deployment Health Assessment TBI screen. Combat experiences were assessed using the sum of the 15-item Combat Experiences Survey adapted for OEF/OIF veterans.23 Continuous PTSD symptom severity was defined as the total sum score from the 17-item PTSD Checklist – Military version (PCL-M).24
Resting HRV was measured for 10 minutes at the start of data collection and is described in more detail elsewhere.25 Briefly, a 12-channel J&J Engineering I-330-C2 Plus instrument with 3 M Red Dot ECG electrodes was used to determine the inter-beat-intervals (or R–R intervals) measured in milliseconds and calculate the standard deviation of R–R intervals (SDNN) and high-frequency (HF, 0.15–0.4 Hz) power (ms2). HF is the most strongly associated with vagally mediated parasympathetic activity and SDNN reflects sympathetic and parasympathetic activity. HF was natural log transformed before analysis because of the wide range and highly skewed distribution of raw HF values.
A Cognitive Bias Recognition Test was used to assess the level of negative cognitive bias present prior to the training. This produces a single, interpretive bias score that is calculated from responses to 10 randomly presented, deployment-related scenarios that are ambiguous with regard to the meaning of the scenario. This measure has been previously validated and was used because earlier work has shown it to be sensitive to changes in interpretive style occurring after CBM-I training.21,26
App use was measured by date/time stamps built into the iPod apps and by self-report. Unfortunately, very few soldiers brought their iPod to the post-deployment assessments so the date/time stamp information was collected for a very small number of participants (N = 6). Instead, self-reported app use data were reported on a scale ranging from 1 = not at all to 7 = more than seven times per week during four time periods: before arriving in Iraq, while in Iraq, between return home and 3-month post-deployment follow-up, and between 3- and 12-month follow-up.
Statistical Analysis
Statistical analyses were conducted using SAS 9.4. Multiple imputations27 were performed for the sample using SAS MI procedure because 17.5% (60/342) of soldiers were missing a combination of pre-deployment combat zone exposure, TBI, childhood abuse, most recent deployment combat exposure, and pre-deployment HRV data. Five imputed datasets were generated to account for the uncertain nature of missing data. Analyses were repeated for each of five imputed datasets and then results were combined using the SAS MIANALYZE procedure.
Due to the repeated measures for each participant and cluster randomization at the company level, generalized linear mixed models (GLMM) were fit with a random intercept specified to account for the correlations within the same companies and a random intercept specified for the participant effect. Given the positive skew for the continuous total PCL score, gamma distribution and log link were specified for this model.
Covariates were included in the model because of the cluster randomization and chosen based on bivariate associations with study arm and PCL score using Chi-square independent test for categorical data and nonparametric Kruskal–Wallis test for continuous data (p ≤ 0.2). The covariates identified included age, gender, race, marital status, tobacco use, childhood abuse, previous combat zone exposure, TBI, number of most recent deployment combat experiences, pre-deployment negative cognitive bias score, and pre-deployment HRV (HF in main analysis and SDNN in separate models). Age and age-squared were included because a quadratic relationship was suggested between age and PCL score. Similar to the model building approach used in the HRV prediction paper, interaction terms between the predictor of interest (study arm) and the covariates were examined and included in the model if significant at p < 0.05.25 Predicted means (LSMEANS) were compared between the intervention and control arms with significance level of p = 0.025 to avoid inflated type-I error. The GLMM equations identified significant resilience intervention effects for subgroups of participants. Effect sizes for these subgroups used the PCL change scores (post-deployment minus pre-deployment) and were calculated as the mean difference of each intervention group minus control group divided by the standard deviation of the difference. When the variances in the two groups were equal, pooled standard deviation was used in the denominator. Otherwise, the standard deviation was calculated as the square root of the sum of the two variances. Effect sizes were calculated this way because there is not a commonly recommended method for calculating effect sizes from GLMM equations and effect sizes on the change scores are analogous to adjusting both observed and unobserved covariates as in the fixed effect model. We did not examine the intervention effect on the dichotomized PCL ≥ 50 (commonly recommended screening cutoff score for PTSD) because there were too few soldiers with post-deployment PTSD symptom severity at or above this threshold (16 soldiers at 3-months post-deployment across three study arms and 6 soldiers at 12-months post-deployment, see Supplemental material for more details). Two sample t-tests were used to compare app use and skill use between HRVB and CMB-I arms. Pearson correlation was used to examine the relationship between app use, age, and previous combat zone exposure.
RESULTS
The demographic and clinical characteristics of participants in each study arm are detailed in Supplementary material. In general, soldiers in this sample were young, Caucasian, enlisted males, who had low levels of pre-deployment PTSD symptoms. If they had deployed previously, nearly all had deployed to an Internal Revenue Service recognized combat zone. There were no significant differences between participants in each study arm except that the HRVB arm included more women (15.7%) than the control arm (4.2%), CBM-I arm had fewer combat experiences during the most recent deployment than the control arm, and the HRVB arm had more days to 12-month follow-up.
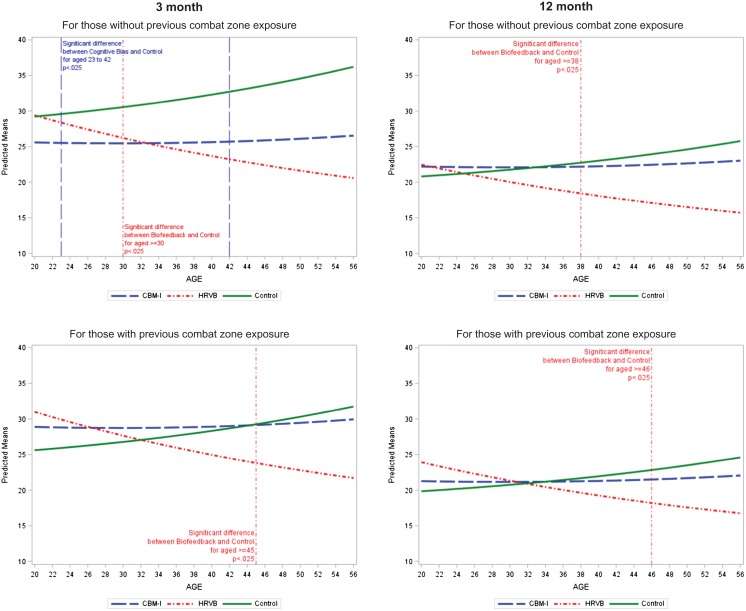
There was no significant overall effect of the interventions on post-deployment PCL, however, there was a significant two-way interaction between study arm and age and a significant three-way interaction between study arm, previous combat zone exposure, and time (Table I). Results were similar when replacing HF with SDNN (see Supplementary material for details). The significant interaction terms indicated that the effect of intervention arms depended on age, having previous combat zone exposure or not, and time since pre-deployment interview. To assist in the interpretation of the significant interaction terms, the predicted means of PCL for the three study arms by age and by time (3- and 12-month post-deployment) are presented in Figure 1 stratified by previous combat zone exposure.
TABLE I.
GLMM for Associations Between Study Arms and Continuous Total PCL Score
| Variable | Parameter Estimate (SE) | p-Value |
|---|---|---|
| Study arm (CBM-I) | 0.17 (0.19) | 0.38 |
| Study arm (HRVB) | 0.50 (0.18)** | 0.007 |
| Time (3-month PCL versus 12-month) | 0.25 (0.09)** | 0.005 |
| Pre-deployment PCL | 0.01 (0.00)** | <0.0001 |
| Age | 0.002 (0.02) | 0.92 |
| Age-squared | 0.0001 (0.00) | 0.80 |
| Gender (Male) | 0.01 (0.06) | 0.92 |
| Race (Caucasian) | −0.04 (0.04) | 0.26 |
| Married/cohabitating (Yes) | −0.001 (0.04) | 0.98 |
| Tobacco use (Yes) | −0.01 (0.03) | 0.72 |
| Childhood abuse (Yes) | 0.07 (0.04) | 0.13 |
| Previous combat zone exposure (No) | 0.05 (0.07) | 0.50 |
| TBI (deployment-related prior to or during most recent deployment) | 0.28 (0.06)** | <0.0001 |
| Number of combat experiences during most recent deployment | 0.04 (0.01)** | <0.0001 |
| Pre-deployment negative cognitive bias | 0.004 (0.00) | 0.13 |
| Pre-deployment ln(HF) | −0.01 (0.01) | 0.30 |
| Days to follow-ups | 0.001 (0.00)** | 0.02 |
| CBM-I study arm × time | 0.05 (0.07) | 0.49 |
| HRVB study arm × time | 0.004 (0.07) | 0.95 |
| CBM-I study arm × age | −0.005 (0.01) | 0.33 |
| HRVB study arm × age | −0.02 (0.01)** | 0.002 |
| Previous combat zone exposure × time | 0.08 (0.06) | 0.15 |
| CBM-I study arm × previous combat zone exposure | −0.004 (0.11) | 0.97 |
| HRVB study arm × previous combat zone exposure | −0.11 (0.10) | 0.28 |
| CBM-I study arm × time × previous combat zone exposure | −0.25 (0.10)** | 0.01 |
| HRVB study arm × time × previous combat zone exposure | −0.07 (0.09) | 0.41 |
**p < 0.025.
CBM-I is cognitive bias modification for interpretation training; HRVB is heart rate variability biofeedback training, HF is heart rate variability frequency domain measure.
FIGURE 1.
Predicted mean for 3- and 12-month post-deployment total PCL score by age and by previous combat zone exposure.
At 3-month post-deployment, the HRVB arm had significantly lower post-deployment total PCL scores compared with the control arm for soldiers without previous combat zone exposure and age 30 and older (unadjusted effect size −0.97 and −1.03, respectively) and for soldiers with previous combat zone exposure and age 45 and older (unadjusted effect size −1.03) (Figure 1). There was also a significant difference between the CBM-I and control arm for soldiers without previous combat zone exposure and age 23–42 years (unadjusted effect size −0.41).
At 12-months post-deployment, there was no significant difference between CBM-I and the control arms. However, older soldiers in the HRVB arm (age 38 and older without previous combat exposure (unadjusted effect size −1.14) and 46 and older with previous combat zone exposure, unadjusted effect size −0.87) had significantly lower post-deployment total PCL scores than the control arm. Other significant predictors in the model predicting total post-deployment PCL scores included: pre-deployment total PCL score, history of deployment-related TBI prior to or during most recent deployment, number of combat experiences during the most recent deployment, and days to follow-ups (see Table I).
Self-reported app use of the BreathPacer (HRVB arm) and iMAT (CBM-I arm) apps was similar during each of the time periods assessed (Table II). However, the use of breath-pacing skills without the app was significantly greater than the use of the cognitive bias modification skills without the app across all time periods. There was no significant correlation between app use or skill use and previous combat zone exposure or age. Self-reported study app use by control arm participants was minimal, only one control arm soldier reported using a study app, suggesting that randomization by company minimized app sharing.
TABLE II.
Self-Report Resilience App Use and Skill Use at least 1–2 Times Per Week
| Breath Pacing App HRVB Arm (%) | Cognitive Bias App CBM-I Arm (%) | p-Value | |
|---|---|---|---|
| Before arrival in combat zone | |||
| App use | 35/91 (38.5) | 32/78 (41.0) | 0.75 |
| Skill use | 34/91 (37.4) | 7/77 (10.4) | 0.0002 |
| In combat zone | |||
| App use | 25/92 (27.5) | 19/78 (24.4) | 0.73 |
| Skill use | 44/91 (48.3) | 8/77 (10.4) | <0.0001 |
| After returning home | |||
| App use | 2/91 (2.2) | 1/78 (1.3) | 0.89 |
| Skill use | 22/90 (24.4) | 1/78 (1.3) | <0.0001 |
CBM-I is cognitive bias modification for interpretation training arm of the study; HRVB is heart rate variability biofeedback training arm of the study.
DISCUSSION
To our knowledge, this is one of the first studies to test resilience trainings associated with actionable physiological and behavioral biomarkers (HRV and cognitive bias) to prevent post-deployment PTSD. Pre-deployment resilience training was acceptable (i.e., attractiveness of pre-deployment resilience training) based on 600 soldiers completing the consent process (the maximum number allowed in the research protocol). Assessment and resilience training during pre-deployment training was feasible (i.e., ability to carry out assessment and intervention activities during pre-deployment training) based on 426/600 (71%) completing the pre-deployment assessment and resilience trainings. Results demonstrated the hypothesized benefit of HRVB at 3-months post-deployment for older soldiers with and without previous combat zone exposure and for CBM-I for soldiers without previous combat zone exposure between 23 and 42 years of age. At 12-months post-deployment, the hypothesized benefit was demonstrated for HRVB only and this was for older soldiers with and without previous combat zone exposure. However, the 12-month HRVB results are tempered by the small number of soldiers in the older age groups who received the HRVB intervention (n = 4 without previous combat exposure and n = 5 with previous combat exposure (see Fig. 1).
The reason for the greater efficacy of the interventions among older National Guard soldiers is not clear. One possibility is that older soldiers reported higher levels of PTSD symptoms and therefore had more room to improve (see Control arm curves showing post-deployment PTSD symptoms increasing with age in Fig. 1). Older National Guard and Reserve component personnel may be at higher risk for post-deployment PTSD because they have more established civilian careers and families and may experience a more challenging transition from civilian to deployed soldier back to civilian.28 Even so, the correlation between app use or skill use and age was not significant and there was no evidence for a significant mediation effect when variables indicating the change in HRV and negative cognitive bias were added to the GLMM equation. However, there were trends consistent with the expected effect of the resilience trainings on their respective physiological and behavioral biomarkers. For example, from pre-deployment to 3-months post-deployment, there was greater improvement in resting HF in the HRVB arm compared with control (~2×) and negative cognitive bias increased for the control arm but did not change for the CBM-I arm. In addition, older soldiers (≥30 years of age) in the HRVB arm experienced more improvement in HRV than younger soldiers in the HRVB arm (SDNN increased 6.4 versus 4.4 and HF increased versus decreased, respectively). Older soldiers also experienced lower PTSD symptoms in the HRVB arm.
Even though the numbers were small, the HRVB intervention demonstrated benefit at 3- and 12-months post-deployment and the CBM-I intervention demonstrated benefit at 3-months only. The benefit of HRVB training is consistent with a recent meta-analysis which found an inverse relationship between PTSD symptom severity and HRV29 and with a recent HRVB literature review which reported support across several disorders including a small number of studies supporting the use of HRVB as an augmentation treatment for PTSD.12 Besides HRVB and breath pacing, there are other strategies that can increase resting levels of HRV including diet, weight loss, smoking cessation, exercise, medication, and meditation.30 There is also accumulating evidence for afferent (ascending) and efferent (descending) vagal pathways that associate HRV with attentional control, emotional regulation, and the integration of the central and autonomic nervous systems.5,11,31 Further, a recent meta-analysis demonstrated an association between HRV and cerebral blood flow to the ventro-medial prefrontal cortex and amygdala32 and these are some of the same brain regions associated with PTSD symptoms.33
The differential effectiveness of the CBM-I intervention in soldiers without previous combat exposure suggests that cognitive biases may be more malleable prior to combat trauma exposure. Cognitive theories of PTSD suggest that, following trauma exposure, cognitive biases crystallize into specific trauma-related beliefs (e.g., “I failed” or “I was weak.”).34,35 In fact, cognitive biases were found to be more strongly related to negative self-beliefs among soldiers with prior combat deployment than among those with no prior combat deployment in this sample.36 Negative trauma-related beliefs, once they have formed, typically require intensive interventions specifically targeting these interpretations (i.e., cognitive processing therapy) and thus may be refractory to a less intense, more indirect CBM-I app training.
Our findings parallel those by Wald who found that attention bias modification training administered prior to deployment moderated the association between combat exposure and PTSD symptoms.37 Notably, Wald and colleagues found that, at least in combat zones, increased attention to rather than away from threat-related stimuli reduced post-deployment PTSD. Taken together with the present results, this suggests that the optimal information-processing style for a combat zone is one that attends toward threat while maintaining a neutral interpretive style. Pre-deployment CBM-I training may thus work best by training soldiers to remain vigilant but without catastrophizing threat.
Other suggested primary PTSD prevention strategies include medications that can block the formation of long-term memory of a traumatic event. This strategy might work for civilian traumatic events but for military personnel, this strategy may be less desirable because recall of events can be critical for planning future military operations.38 The use of HRVB and/or CBM-I could complement other pre-deployment training and stress-inoculation efforts without compromising combat zone effectiveness.39,40 The difference in skill use between HRVB and CBM-I may be explained by the ease of using HRVB skills without the app and/or the familiarity of breath pacing which is used in other aspects of military training (e.g., shooting range). Future CBM-I should include attention to developing skills that can be used without app use.
There are several noteworthy limitations to this study. Very few soldiers brought their iPod to the post-deployment assessment; therefore, app use data were only available from self-report. Similarly, combat experiences during the most recent deployment were only available from self-report. During post-deployment interviews, soldiers reported multiple challenges associated with the use of an iPod app in a combat zone that were not anticipated by the study team. These challenges included: the loss of the study app after synching with an existing iTunes account, the loss or breakdown of the study iPod for multiple reasons, and the restricted use of an iPod during deployment. Although study participants assigned to the intervention arms were given contact information to obtain a replacement iPod if for any reason it was lost or non-functional, only 24 soldiers did so. The study design did not allow study personnel to contact soldiers during deployment; therefore, it is not known how many or when in the deployment cycle soldiers lost access to the intervention apps. The follow-up rate was low: 75.2% and 57.3% at 3- and 12-month post-deployment, respectively, which nonetheless compares favorably with the 62.0% follow-up rate at 4- to 6-months in the active duty Marine Resilience Study.41 There were also significant differences in the sociodemographic and military rank variables between those soldiers who completed post-deployment follow-up assessments and those who did not suggest that lower ranking soldiers may have had more difficulty taking the time to complete the follow-up interviews during drill weekend. However, there were no differences between follow-up completers and non-completers in pre-deployment PTSD symptoms, HRV, or negative cognitive bias. Finally, there was a generally low level of post-deployment PTSD symptom severity in this sample. Therefore, it is not known what the impact of these resilience trainings would be in a sample with higher levels of post-deployment PSTD.
Supplementary Material
Acknowledgements
The authors wish to acknowledge the research staff (Regina Stanley, Susan Jegley, Debbie Hodges, and Mitzi Mosier) and Army National Guard soldiers who made this study possible.
Conflict of interest
M.D. and B.K.W. receive salary support from Virtual Reality Medical Centers. R.M. and D.C. receive salary support from Institute of HeartMath. J.M.P., J.I.C., J.T.N., D.P.G., T.K., T.L.K., D.K.W., R.N.G., J.S., T.R.M. reported no biomedical financial interests or potential conflicts of interest. J.A.P. and X.H. reported no biomedical financial interests or potential conflicts of interest.
Previous presentations
Pyne JM. “Pre-deployment Heart Rate Variability Predicting and Preventing Post-deployment PTSD” Oral Presentation for Military Health System Research Symposium, Orlando, FL. August 2017.
Funding
This work was supported by research grants from the Department of Defense (grant number W81XWH-08-2-0031); VA South Central Mental Illness Research, Education, and Clinical Center (MIRECC); and National Institute of Health (grant number P30 GM110702).
REFERENCES
- 1. Kok BC, Herrell RK, Thomas JL, Hoge CW: Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling prevalence differences between studies. J Nerv Ment Dis 2012; 200(5): 444–50. [DOI] [PubMed] [Google Scholar]
- 2. Deahl M: Traumatic stress--is prevention better than cure? J R Soc Med 1998; 91(10): 531–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riggs DS, Sermanian D: Prevention and care of combat-related PTSD: directions for future explorations. Mil Med 2012; 177(8 Suppl): 14–20. [DOI] [PubMed] [Google Scholar]
- 4. Institute of Medicine : Preventing psychological disorders in service members and their families: an assessment of programs. Mil Med 2014; 179(11): 1173–5. [DOI] [PubMed] [Google Scholar]
- 5. Thayer JF, Lane RD: A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord 2000; 61(3): 201–16. [DOI] [PubMed] [Google Scholar]
- 6. Beauchaine TP, Thayer JF: Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol 2015; 98(2): 338–50. [DOI] [PubMed] [Google Scholar]
- 7. Ginsberg JP, Berry ME, Powell DA: Cardiac coherence and posttraumatic stress disorder in combat veterans. Altern Ther Health Med 2010; 16(4): 52–60. [PubMed] [Google Scholar]
- 8. Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH: Stress and heart rate variability: a meta-analysis and review of the literature. Psychiatry Investig 2018; 15(3): 235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Diamond LM, Hicks AM, Otter-Henderson KD: Individual differences in vagal regulation moderate associations between daily affect and daily couple interactions. Pers Soc Psychol Bull 2011; 37(6): 731–44. [DOI] [PubMed] [Google Scholar]
- 10. Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH: Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med 2009; 37(2): 141–53. [DOI] [PubMed] [Google Scholar]
- 11. McCraty R, Zayas MA: Cardiac coherence, self-regulation, autonomic stability, and psychosocial well-being. Front Psychol 2014; 5: 1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gevirtz R: The promise of heart rate variability biofeedback: evidence-based applications. Biofeedback 2015; 41(3): 110–20. [Google Scholar]
- 13. Lehrer PM, Gevirtz R: Heart rate variability biofeedback: how and why does it work? Front Psychol 2014; 5: 756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Browning M, Holmes EA, Charles M, Cowen PJ, Harmer CJ: Using attentional bias modification as a cognitive vaccine against depression. Biol Psychiatry 2012; 72: 572–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Telman MD, Holmes EA, Lau JY: Modifying adolescent interpretation biases through cognitive training: effects on negative affect and stress appraisals. Child Psychiatry Hum Dev 2013; 44: 602–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Woud ML, Postma P, Holmes EA, Mackintosh B: Reducing analogue trauma symptoms by computerized reappraisal training – considering a cognitive prophylaxis? J Behav Ther Exp Psychiatry 2013; 44: 312–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dunmore E, Clark DM, Ehlers A: A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behav Res Ther 2001; 39: 1063–84. [DOI] [PubMed] [Google Scholar]
- 18. Bryant RA, Guthrie RM: Maladaptive appraisals as a risk factor for posttraumatic stress: a study of trainee firefighters. Psychol Sci 2005; 16: 749–52. [DOI] [PubMed] [Google Scholar]
- 19. Elwood LS, Williams NL, Olatunji BO, Lohr JM: Interpretation biases in victims and non-victims of interpersonal trauma and their relation to symptom development. J Anxiety Disord 2007; 21(4): 554–67. [DOI] [PubMed] [Google Scholar]
- 20. Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF: Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA 2006; 296(5): 519–29. [DOI] [PubMed] [Google Scholar]
- 21. Peters KD, Constans JI, Mathews A: Experimental modification of attribution processes. J Abnorm Psychol 2011; 120(1): 168–73. [DOI] [PubMed] [Google Scholar]
- 22. Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ: Validation of scales from the deployment risk and resilience inventory in a sample of Operation Iraqi Freedom veterans. Assessment 2008; 15(4): 391–403. [DOI] [PubMed] [Google Scholar]
- 23. Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL: Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351(1): 13–22. [DOI] [PubMed] [Google Scholar]
- 24. Keen SM, Kutter CJ, Niles BL, Krinsley KE: Psychometric properties of PTSD Checklist in sample of male veterans. J Rehabil Res Dev 2008; 45(3): 465–74. [DOI] [PubMed] [Google Scholar]
- 25. Pyne JM, Constans JI, Wiederhold MD, et al. : Heart rate variability: Pre-deployment predictor of post-deployment PTSD symptoms. Biol Psychol 2016; 121(Pt A): 91–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mathews A, Mackintosh B: Induced emotional interpretation bias and anxiety. J Abnorm Psychol 2000; 109(4): 602–15. [PubMed] [Google Scholar]
- 27. Rubin DB: Inference and missing data. Biometrika 1976; 63(3): 581–92. [Google Scholar]
- 28. Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR: Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health 2009; 99(9): 1651–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chalmers JA, Quintana DS, Abbott MJ, Kemp AH: Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry 2014; 5: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Thayer JF, Yamamoto SS, Brosschot JF: The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol 2010; 141(2): 122–31. [DOI] [PubMed] [Google Scholar]
- 31. Huang C, Gevirtz RN, Onton J, Criado JR: Investigation of vagal afferent functioning using the heartbeat event related potential. Int J Psychophysiol 2017;pii: S0167-8760(17)30109-5. doi: 10.1016/j.ijpsycho.2017.06.007. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 32. Thayer JF, Ahs F, Fredrikson M, Sollers JJ III, Wager TD: A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev 2012; 36(2): 747–56. [DOI] [PubMed] [Google Scholar]
- 33. Etkin A, Wager TD: Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 2007; 164(10): 1476–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Resick PA, Schnicke MK: Cognitive processing therapy for sexual assault victims. J Consult Clin Psychol 1992; 60(5): 748–56. [DOI] [PubMed] [Google Scholar]
- 35. Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behav Res Ther 2000; 38(4): 319–45. [DOI] [PubMed] [Google Scholar]
- 36. Nanney JT, Constans JI, Kimbrell TA, Kramer TL, Pyne JM: Differentiating between appraisal process and product in cognitive theories of posttraumatic stress. Psychol Trauma 2015; 7(4): 372–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wald I, Bitton S, Levi O, et al. : Acute delivery of attention bias modification training (ABMT) moderates the association between combat exposure and posttraumatic symptoms: a feasibility study. Biol Psychol 2017; 122: 93–7. [DOI] [PubMed] [Google Scholar]
- 38. Burbiel JC: Primary prevention of posttraumatic stress disorder: drugs and implications. Mil Med Res 2015; 2: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stetz MC, Thomas ML, Russo MB, et al. : Stress, mental health, and cognition: a brief review of relationships and countermeasures. Aviat Space Environ Med 2007; 78(5 Suppl): B252–60. [PubMed] [Google Scholar]
- 40. Hourani LL, Council CL, Hubal RC, Strange LB: Approaches to the primary prevention of posttraumatic stress disorder in the military: a review of the stress control literature. Mil Med 2011; 176(7): 721–30. [DOI] [PubMed] [Google Scholar]
- 41. Minassian A, Maihofer AX, Baker DG, Nievergelt CM, Geyer MA, Risbrough VB: Association of predeployment heart rate variability with risk of postdeployment posttraumatic stress disorder in active-duty marines. JAMA Psychiatry 2015; 72(10): 979–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.