Abstract
Background:
CT is commonly used in the emergency department (ED) to evaluate patients with abdominal pain, but exposes them to ionizing radiation, a possible carcinogen. MR does not utlize ionizing radiation and may be an alternative.
Purpose:
To compare the sensitivity of MR and CT for acute abdominopelvic ED diagnoses.
Study Type:
Prospective, observational cohort
Population:
ED Patients ≥12 years old and undergoing CT for possible appendicitis.
Field Strength/Sequence:
1.5T MR, including T1-weighted, T2-weighted, and diffusion-weighted imaging sequences
Assessment:
Three radiologists independently interpreted each MR and CT image set separately and blindly, using a standard case report form. Assessments included likelihood of appendicitis, presence of an alternative diagnosis, and likelihood that the alternative diagnosis was causing the patient’s symptoms. An expert panel utilized chart review and follow-up phone interviews to determine all final diagnoses. Times to complete image acquisition and image interpretation were also calculated.
Statistical Tests:
Sensitivity was calculated for each radiologist and by consensus (≥2 radiologists in agreement) and are reported as point estimates with 95% confidence intervals. Two-sided hypothesis tests comparing the sensitivities of the three image types were conducted using the Pearson’s Chi-squared test with the traditional significance level of p=0.05.
Results:
There were 15 different acute diagnoses identified on the CT/MR images of 113 patients. Using individual radiologist interpretations, the sensitivities of non-contrast enhanced MR (NCE-MR), contrast-enhanced MR (CE-MR), and CT for any acute diagnosis were 77.0% (72.6%−81.4%), 84.2% (80.4%−88.0%), and 88.7% (85.5%−92.1%). Sensitivity of consensus reads was 82.0% (74.9%−88.9%), 87.1% (81.0%−93.2%), 92.2% (87.3%−97.1%), respectively. There was no difference in sensitivities between CE-MR and CT by individual (p=0.096) or consensus interpretations (p=0.281), though NCE-MR was inferior to CT in both modes of analysis (p<0.001, p=0.031, respectively).
Conclusion:
The sensitivity of CE-MR was similar to CT when diagnosing acute, non-traumatic abdominopelvic pathology in our cohort.
Keywords: abdominal pain, emergency medicine, magnetic resonance imaging, multidetector computed tomography
Introduction
CT is a near ubiquitous component of the evaluation of unexplained acute and chronic abdominal pathology due to its widespread availability, high efficiency, and high overall diagnostic accuracy. Abdominal imaging is particularly relevant to the ED setting, where abdominal pain constitutes the most frequent presenting symptom (1). Hence, one of the most common uses of emergent CT is to evaluate for the presence or absence of appendicitis, particularly in those patients with right lower quadrant pain (2).
While the advent of CT has tremendously benefited the diagnostic evaluation of patients with abdominal pain, there are some theoretical risks. In particular, exposure to ionizing radiation is inherent to CT and it is well accepted that high doses of ionizing radiation are a risk factor for development of malignancy. While the risk attributable to a single CT scan remains uncertain and projections based on epidemiologic data are controversial (3), the perception of risk exists regardless of the actual risk.
Therefore, the judicious use of CT imaging is a sensible goal, especially among younger patients, and investigation into alternative imaging modalities that avoid ionizing radiation is advocated by medical societies (4). Ultrasound has been proposed as one such alternative, but its use is hindered by a relatively high degree of operator dependence, a limitation reflected in the American College of Radiology’s Appropriateness Criteria for Right Lower Quadrant Pain, which reserves recommendation for ultrasound to pediatric or pregnant patients (5). Emerging research has demonstrated encouraging results for the use of MR imaging to evaluate for appendicitis; two recent systematic reviews and meta-analyses found pooled sensitivity and specificity of MR in the evaluation of appendicitis to be approximately 96% (6, 7).
Beyond evaluating for appendicitis, however, CT imaging also has a demonstrated ability to detect alternative causes of abdominal pain. In fact, only about one-quarter of CTs requested for the detection of appendicitis will actually be positive for the disease, while about 32% will have an alternative diagnosis found and about 45% will have no specific pathology identified (8). While previous work has demonstrated good performance of MR for appendicitis (9), a barrier to implementation of MR as a first-line test for the evaluation of patients with possible appendicitis is the legitimate concern over whether MR will reveal alternative etiologies that explain a patient’s symptoms with acceptable diagnostic performance.
Thus, the purpose of this study was to estimate and compare the sensitivity of MR and CT for the detection of any acute diagnosis in patients presenting with signs and symptoms concerning for appendicitis.
Materials and Methods
Study Design and Setting
This is a HIPAA-compliant and IRB-approved prospective study of a convenience sample of patients presenting with abdominal pain concerning for possible acute appendicitis. The study took place at the ED of an academic medical center that saw approximately 50,000 annual visits at the time of the study (February 2012-August 2014). Written informed consent was obtained for all enrollees.
Patient Selection
Patients were eligible for inclusion if they had a CT requested to evaluate for possible appendicitis. Exclusion criteria were age <12 years old (selected to minimize need for sedation during MR image acquisition), inability to provide informed consent or assent, contraindication to intravenous gadolinium contrast, or contraindication to undergoing MR (e.g. pregnancy, ferromagnetic implants, etc.). Patients meeting eligbility criteria were approached for enrollment by either the ED treatment team or a research assistant during study hours. Subjects were included in the current analysis if they satisfied two criteria as determined by an expert panel: 1) there was an acute diagnosis that could explain the patient’s abdominal pain and 2) the diagnosis was correctly identified by at least one of the three radiologists on either the research CT or MR image interpretations.
CT Protocol
CT exams of the abdomen and pelvis were performed using a 64 × 0.625mm detector configuration scanner, (GE Healthcare, Waukesha, WI) following oral contrast (Gastrografin, Bracco Diagnostics, Princeton, NJ) and intravenous iohexol (Omnipaque-300, GE Healthcare, Waukesha, WI) administration with imaging in the portal venous phase (SmartPrep with automated scan initiation). Size-specific protocols for small, medium, and large body habitus range from 100–140 kVp with modulated mAs (Smart mA with mA range = 30–600 and noise index 15–21). Images were reconstructed with 5-mm slice thickness at 3-mm intervals using an iterative image reconstruction protocol (40% ASIR blend with standard FBP) in the axial, sagittal, and coronal planes.
MR protocol
MR was performed on 1.5T scanners (Signa HDxt CRM or TwinSpeed, Discovery MR450w) using an 8-channel body phased array coil and included NCE-MR with diffusion-weighted imaging (DWI) and CE-MR. Details of the MR protocol have been previously reported (10). In brief, it included multiple orthogonal planes of T2-weighted single-shot fast spin-echo, pre- and post-contrast T1-weighted 3D spoiled gradient echo, and DWI. For contrast-enhanced T1-weighted imaging, 0.1mmol/kg of gadobenate dimeglumine (Multihance, Bracco Diagnostics, Princeton, NJ) was administered intravenously at 2ml/s, followed by a 20ml saline flush injected at the same rate.
Data Acquisition
All MR and CT images were anonymized and placed in a random reading order for each research radiologist. These three fellowship-trained abdominal radiologists (DRK, JBR, TJZ), each with 1–4 years of post-fellowship experience at the time of the study, independently interpreted all CT and MR images, completing a standardized case report form that inquired about several findings potentially indicative of appendicitis and a question regarding the presence or absence of an alternative diagnosis that may explain the patient’s lower abdominal pain. These radiologists were blinded to all clinical information except that a CT was ordered for a suspicion for appendicitis. Patient follow-up consisted of a chart review at one month for any subsequent visits within our health system. Surgical and pathology reports were collected on those patients who underwent surgery and all others had a follow-up phone interview in conjunction with chart review.
A single research assistant (JBH), blinded to the study hypothesis and trained in chart review methods, followed a standard protocol to conduct the one month chart review and follow-up phone interview. In addition, an expert panel of three senior researchers (two radiologists and an emergency physician; PJP, SBR, MDR) determined the final diagnoses of all patients utilizing the integration of all follow-up data, assigning the most weight to surgical and pathological data, then information from subsequent clinic visits, and finally follow-up phone interview.
Outcomes and Analysis
The primary outcome of this study was the sensitivity of MR and CT in the diagnosis of all acute causes of abdominal pain in patients presenting with signs and symptoms suggestive of appendicitis. This was calculated for each imaging type: NCE-MR with DWI, CE-MR, and CT. The results are presented for individual radiologist reads as well as a consensus read for each case (i.e. – at least 2 radiologists agreed on the diagnosis). Data are reported as point estimates with 95% confidence intervals. Two-sided hypothesis tests comparing the sensitivities of the three image types were conducted using the McNemar test with the traditional significance level of p=0.05. For individual reads, because each case was read by three radiologists, we used robust variance estimates to account for the within-case correlation in the construction of confidence intervals and hypothesis tests. Our approach is based on the case-specific influence function of the target statistic and is analogous to the sandwich variance estimator in the generalized estimating equations.(11) Lastly, after excluding cases with a diagnosis of appendicitis, we also determined the sensitivity of each modality for the detection of alternative diagnoses. All statistical analyses were performed using R (R Foundation, Vienna, Austria. http://www.R-project.org/).
Results
Characteristics of Study Subjects
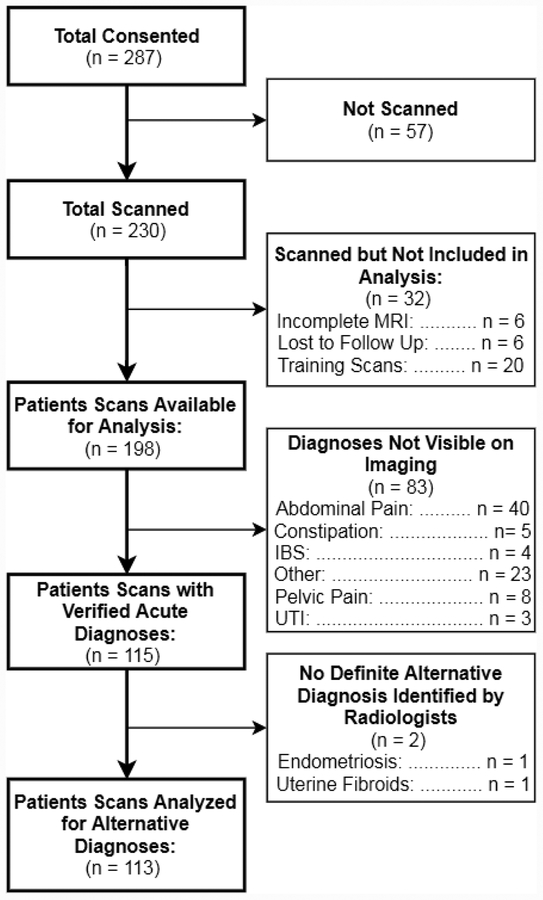
In the parent study, 230 patients were enrolled from February 2012 to August 2014. Images from the first 20 patients were used as a training set for the study radiologists, and thus were excluded from analysis. An additional 12 patients were excluded from analysis; six patients were lost to follow-up (did not have any subsequent clinic visits in our system and were unreachable for follow-up phone interview) and another six did not complete MR imaging for various reasons (e.g. – claustrophobia/anxiety, change in clinical condition, or technical failure in contrast administration). Thus, 198 patients comprised the study cohort for the current study. Of these, 113 had an acute diagnosis identifiable by imaging that was reported by at least one of the study radiologists. Figure 1 illustrates the flow of patients through the study. In our study cohort of 198 patients, the mean age was 33 years (SD 15) years and 55% were women.
Figure 1: Patient Flow Diagram.
UTI = urinary tract infection, IBS = irritable bowel syndrome.
Among the 113 patients with identifiable acute diagnoses, 15 unique acute diagnoses were reported. The most common diagnoses were: appendicitis (n=62), symptomatic ovarian cyst (n=19), diverticulitis (n=7), colitis (n=4), enteritis (n=4), and ureterolithiasis (n=4) (Figures 2 and 3). Of note, three study subjects each had two independent acute diagnoses; they were analyzed as separate instances within the relevant diagnosis categories, resulting in the total number of cases summing to 116.
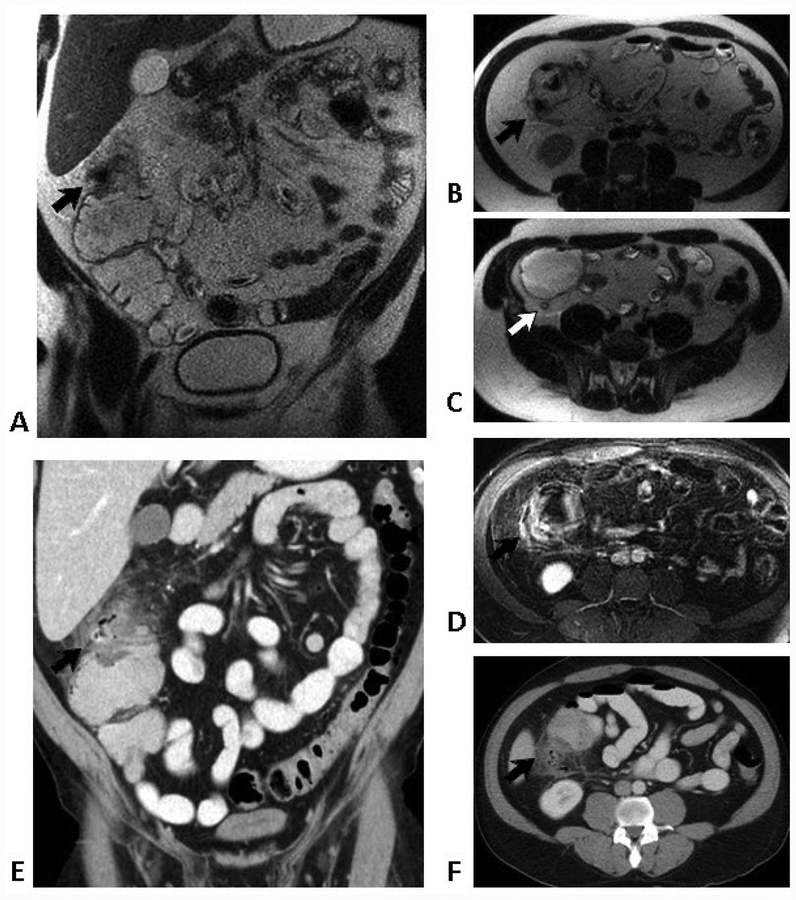
Figure 2.
52-year-old man with acute right-sided abdominal pain.
Coronal (A) and transverse (B & C) T2-weighted SSFSE images show a hypointense focus of gas and surrounding inflammatory changes involving the ascending colon (black arrows), compatible with acute diverticulitis. Note normal appendix (white arrow). Pericolonic inflammation is even more apparent on the fat-suppressed post-contrast T1-weighted images (D). Similar findings are present on the contrast-enhanced coronal (E) and transverse (F) CT images (arrows).
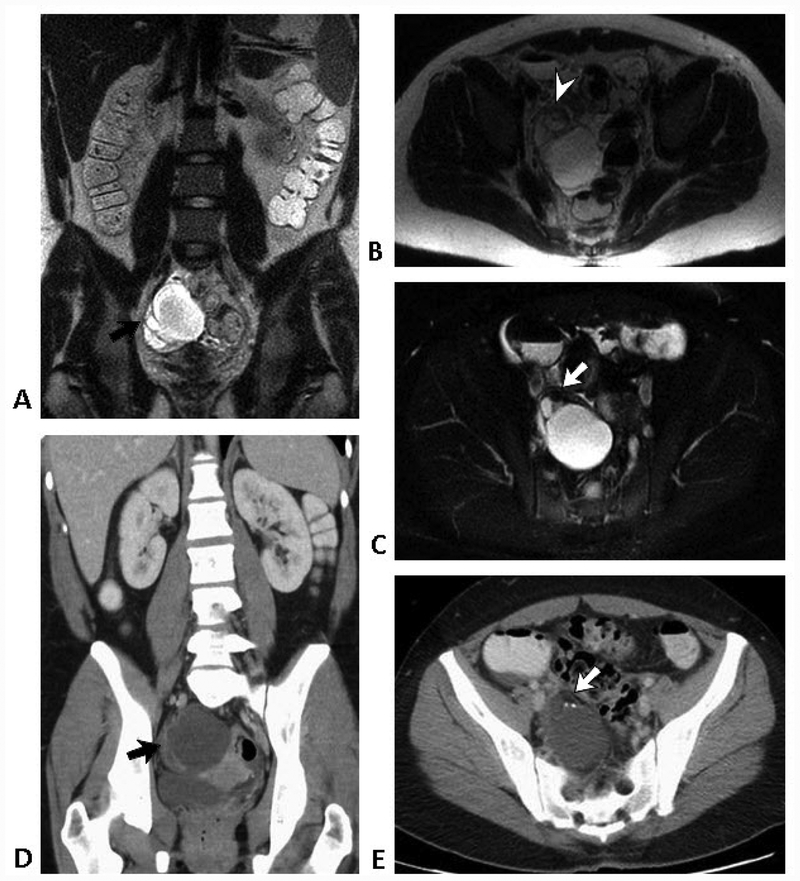
Figure 3.
25-year-old woman with acute right lower quadrant pain.
Coronal (A) and transverse (B) T2-weighted SSFSE images show a complex cystic right adnexal mass (arrow), with a whorled appearance in the periphery (arrowhead) suggesting torsion. Fat-suppressed T2-weighted image (C) demonstrates a small focus of fat (arrow), diagnostic of mature teratoma. Contrast-enhanced coronal (D) and transverse (E) CT images show the torsed cystic adnexal mass (black arrow) with foci of fat and calcium (white arrow). Teratoma with partial torsion was confirmed at subsequent laparoscopy.
When considering all individual radiologist interpretations, the sensitivity (95% confidence intervals) of NCE-MR, CE-MR, and CT for any acute diagnosis was 77.0% (72.6%−81.4%), 84.2% (80.4%−88.0%), and 88.7% (85.5%−92.1%). See Table 1 for details by diagnosis. When considering the consensus interpretation for each case (i.e. – agreement between two or more radiologists for a given case) the sensitivity of NCE-MR, CE-MR, and CE-CT was 82.0% (74.9%−88.9%), 87.1% (81.0%−93.2%), and 92.2% (87.3%−97.1%), respectively. See Table 2 for details organized by diagnosis. For individual radiologist interpretations, the differences in sensitivity comparing NCE-MR vs CT (p<0.001) and NCE-MR vs CE-MR (p=0.021) were both statistically significant. However, no statistically significant difference was found when comparing CE-MR to CT using individual radiologist interpretions (p=0.096). For consensus interpretations, the difference between NCE-MR vs CT was statistically significant (p=0.031) while those comparing CE-MR vs CT (p=0.281) and NCE-MR vs CE-MR (p=0.364) were not.
Table 1. Sensitivity of NCE-MR, CE-MR, and CT; Individual Interpretations.
This table illustrates the sensitivities of each modality for each of the 15 diagnoses in our cohort. The proportion that answered yes to the question, “did the post-contrast images help or add to the diagnosis in any way?,” are presented along with the response rate. Total cases sum to 116 as three patients each had two independent diagnoses.
| Diagnosis | Count | Individual Sensitivities | |||
|---|---|---|---|---|---|
| NCE-MR | CE-MR | Did Contrast Help? (response rate) | CT | ||
| Appendicitis | 62 | 89.8% (85.4 – 94.1%) |
96.2% (93.5 – 99%) |
43% (47%) |
96.8% (94.2 – 99.3%) |
| Ovarian cyst | 19 | 77.2% (66.3 – 88.1%) |
78.9% (68.4 – 89.5%) |
47% (86%) |
70.2% (58.3 – 82.1%) |
| Diverticulitis | 7 | 38.1% | 57.1% | 71% (81%) |
90.5% |
| Colitis | 4 | 66.7% | 75.0% | 36% (92%) |
100% |
| Enteritis | 4 | 100% | 100% | 45% (92%) |
83.3% |
| Ureterolithiasis | 4 | 91.7% | 91.7% | 36% (92%) |
100% |
| Epiploic Appendagitis | 3 | 22.2% | 33.3% | 63% (89%) |
77.8% |
| Cholecystitis | 2 | 33.3% | 50% | 33% (83%) |
83.3% |
| Cholelithiasis | 2 | 0% | 0% | 33% (83%) |
66.7% |
| Meckel’s Diverticulitis | 2 | 33.3% | 33.3% | 100% (67%) |
100% |
| Pyelonephritis | 2 | 33.3% | 100% | 100% (100%) |
83.3% |
| Torsion | 2 | 50% | 50% | 60% (80%) |
83.3% |
| Abscess | 1 | 66.7% | 66.7% | 100% (67%) |
33.3% |
| Degenerating fibroid | 1 | 100% | 100% | 100% (100%) |
100% |
| Ovarian Cancer | 1 | 66.7% | 100% | 67% (100%) |
0% |
| All Acute Diagnoses | 116 | 77% (72.6 – 81.4%) |
84.2% (80.4 – 88%) |
50% (67%) |
88.7% (85.5 – 92.1%) |
| Non-Appendicitis Diagnoses | 54 | 62.3% (54.9 – 70%) |
70.4% (63.3 – 77.4%) |
55% (86%) |
79.6% (73.4 – 85.8%) |
Table 2. Sensitivity of NCE-MR, CE-MR, and CT; Consensus Interpretations.
This table illustrates the sensitivities of each modality for each of the 15 diagnoses when considering consensus interpretations (at least two of three radiologists identified the pathology).
| Diagnosis | Count | Consensus Sensitivities | ||
|---|---|---|---|---|
| NCE-MR | CE-MR | CT | ||
| Appendicitis | 62 | 93.5% (87.4 – 99.7%) |
96.8% (92.4 – 100%) |
98.4% (95.3 – 100%) |
| Ovarian cyst | 19 | 84.2% (67.8 – 100%) |
89.5% (75.7 – 100.0%) |
73.7% (53.9 – 93.5%) |
| Diverticulitis | 7 | 28.6% | 57.1% | 100% |
| Colitis | 4 | 75% | 75% | 100% |
| Enteritis | 4 | 100% | 100% | 75% |
| Ureterolithiasis | 4 | 100% | 100% | 100% |
| Epiploic Appendagitis | 3 | 33.3% | 33.3% | 100% |
| Cholecystitis | 2 | 50% | 50% | 100% |
| Cholelithiasis | 2 | 0% | 0% | 100% |
| Meckel’s Diverticulitis | 2 | 50% | 50% | 100% |
| Pyelonephritis | 2 | 50% | 100% | 100% |
| Torsion | 2 | 50% | 50% | 100% |
| Abscess | 1 | 100% | 100% | 0.0% |
| Degenerating fibroid | 1 | 100% | 100% | 100% |
| Ovarian Cancer | 1 | 100% | 100% | 0% |
| All Acute Diagnoses | 116 | 82% (74.9 – 88.9%) |
87.1% (81.0 – 93.2%) |
92.2% (87.3 – 97.1%) |
| Non-Appendicitis Diagnoses | 54 | 67.9% (55.4 – 80.5%) |
67.9% (55.4 – 80.5%) |
84.9% (75.3 – 94.5%) |
Secondary Findings
When considering individual interpretations for only acute, non-appendicitis diagnoses, sensitivities (95% confidence intervals) of NCE-MR, CE-MR, and CT were 62.3% (54.9%−70.9%), 70.4% (63.3%−77.4%), and 79.2% (73.4%−85.8%), respectively. For consensus interpretations of these same diagnoses, sensitivities of NCE-MR, CE-MR, and CT were 67.9% (55.4%−80.5%), 67.9% (55.4%−80.5%), and 84.9% (75.3%−94.5%), respectively. For individual reads, the difference in sensitivity comparing NCE-MR vs CT was significant (p<0.001) while that between CE-MR vs CT and NCE-MR vs CE-MR were not (p=0.072 and p=0.158, respectively). For consensus reads, the differences comparing NCE-MR vs CT, CE-MR vs CT, and NCE-MR vs CE-MR were all non-significant (p=0.068, 0.331, and 0.519, respectively).
The most acutely serious non-appendicitis diagnoses identified in our cohort were ovarian torsion, pyelonephritis, and abscess. On consensus reads, torsion was identified in one of two cases on CE-MR and in both cases on CT (Figure 3). Pyelonephritis was accurately characterized in both cases by both modalities. The single case of a pelvic abscess was identified on CE-MR, but not on CT. The most common alternative diagnoses to appendicitis were symptomatic ovarian cysts and diverticulitis. In the 19 cases of ovarian cysts, consensus reads of CE-MR identified 17, NCE-MR identified 16, while CT identified 14 of these. For seven cases of diverticulitis, consensus reads of CT identified all 7 while CE-MR identified 4 (Figure 2). A single patient presenting with symptoms related to previously unknown ovarian cancer was correctly identified on CE-MR by all three study radiologists, but not on CT.
For consensus reads of all acute diagnoses, the addition of intravenous contrast increased the sensitivity of MRI from 82.0% to 87.1%, though this was not statistically significant. Both modalities identified all cases of ureterolithiasis, pyelonephritis, and uterine fibroids. CT also identified all cases of colitis, epiploic appendagitis, cholecystitis, cholelithiasis, and Meckel’s diverticulitis. Conversely, CE-MR identified all cases of enteritis, pelvic abscess, and ovarian neoplasm. Both performed well in the diagnosis of appendicitis; CE-MR identified 60 (96.8%) of 62 cases and CT identified 61 (98.4%) cases.
Discussion
Several recent publications have reported the accuracy of MR specifically for the diagnosis of appendicitis (9, 12–14). However, because non-appendiceal pathologies have a higher prevalence than appendicitis among patients undergoing CT for possible appendicitis (8), understanding the performance of MR as it pertains to these alternative diagnoses is imperative. In this study, we present the sensitivity of both NCE-MR and CE-MR for alternative diagnoses observed in those patents undergoing imaging due to clinical suspicion of appendicitis. We found that the sensitivity of CE-MR was comparable to that of CT; whether analyzing data by the individual or consensus interpretation, we found no statistically significant difference. These findings remained true when cases of acute appendicitis were excluded from analysis and only alternative diagnoses were evaluated, again whether analyzed by individual radiologist reads or by consensus. However, this study was not specifically powered to prove the non-inferiority of MR relative to CT. Therefore, while the results of this study are promising and may reflect that MR is an appropriate first-line imaging test for patients being evaluated for possible appendicitis in the ED setting, further study is needed to confirm our findings.
With only a small number of cases for each individual pathology, making definitive statements regarding the comparative effectiveness of these imaging modalities for each diagnosis type would be inappropriate. When all alternatives are considered together, however, one trend seemed clear: NCE-MR performed worse than either CE-MR or CT. This finding is noteworthy since nearly all comparisons of MR versus CT for the evaluation of acute abdominal pathology have used NCE-MR. To our knowledge, our study is the first of its kind to systematically compare NCE-MR (with DWI) to CE-MR as well as CT. The difference in sensitivity observed in our study suggests one of two conclusions. Either intravenous contrast enhancement does improve the sensitivity of MR for these diagnoses or additional training is required for those radiologists interested in using NCE-MR for the detection of these acute, non-appendicitis pathologies. Given that our study radiologists were primarily trained to detect appendicitis on our research MR images, the difference in sensitivity may simply reflect a deficit in training. Though all of our radiologists were fellowship-trained in abdominal imaging, they were mostly experienced in CT of the acute abdomen and had limited training in MR to evaluate for acute abdominal pain. Previous work suggests that training may indeed be the key: radiologist interpretations with regard to the diagnosis of acute appendicitis became more accurate with increasing experience (15). While this constitutes a hurdle to the implementation of NCE-MR for the evaluation of acute, non-traumatic abdominal pain, it is also an opportunity for further study to fully understand the reason for the difference observed. A recently published pictorial review may serve as a reference for such endeavors (16).
Our study has a number of limitations. First and foremost, the radiologists were asked about the possibility of an alternative diagnosis only after many other questions specific to the possibility of appendicitis. For both CT and MR, it is very likely that they were focused more on the evaluation of appendicitis than identifying alternative diagnoses, which could explain why sensitivities for appendicitis were higher than those for non-appendicitis diagnoses. Further, the training of these radiologists to interpret these MR sequences was focused on appendicitis, not on identifying any etiology of abdominal pain. This too may have influenced our findings, as discussed above. Second, the parent study was designed and powered to compare the test characteristics of MR versus CT imaging in the diagnosis of appendicitis. As such, to draw firm conclusions about their comparative performance in the evaluation of each alternative diagnosis, a much larger study would be required. Third, the study was conducted at a single academic center with three fellowship-trained abdominal radiologists, potentially limiting generalizability. Finally, participants were recruited as a convenience sample, potentially introducing selection bias. However, the prevalence of appendicitis observed in this study was similar to that previously reported for CT at our center (17).
Our results serve as a ‘proof of concept’ that MR is capable of identifying many of the most common clinical mimics of acute appendicitis. Further research that is specifically designed and adequately powered to answer the question of the diagnostic accuracy of MR for alternative diagnoses to appendicitis is warranted. Our findings also highlight the critical importance of physician understanding of the diagnostic tools at their disposal. After a negative result on a CT looking for appendicitis, we can be relatively confident that diverticulitis would have been identified, if present. However, if clinical suspicion for ovarian pathology remains high, further workup should be undertaken. Likewise, imperfection in the sensitivity of MR for some alternative diagnoses should not be cause to disregard it entirely, but instead be met with an understanding of which possible entities may warrant further workup.
In conclusion, we found that the sensitivity of CE-MR was similar to CT for the diagnosis of acute, non-traumatic abdominal pain in our cohort. However we did observe a statistically significant difference in the sensitivity of CT when compared against NCE-MR. Further studies into the use of MR for non-traumatic acute abdominal pain are warranted.
Grant Support:
Research reported in this manuscript was supported by the National Institutes of Health National Center for Advancing Translational Sciences under awards UL1 TR000427 and KL2 TR000428 as well as the National Institute for Diabetes and Digestive and Kidney Diseases under awards K24 DK102595 and K08 DK111234. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The University of Wisconsin - Madison Department of Radiology also receives research support from GE Healthcare and Bracco Diagnostics.
References
- 1.Pitts SR, Niska RW, Xu J, Burt CW: National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Rep 2008:1–38. [PubMed] [Google Scholar]
- 2.Repplinger MD, Weber AC, Pickhardt PJ, et al. : Trends in the Use of Medical Imaging to Diagnose Appendicitis at an Academic Medical Center. J Am Coll Radiol JACR 2016; 13:1050–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon AK, Dendy P: Spiral CT: how much does radiation dose matter? Lancet 1998; 352:1082–1083. [DOI] [PubMed] [Google Scholar]
- 4.Moore CL, Broder J, Gunn ML, et al. : Comparative Effectiveness Research: Alternatives to “Traditional” Computed Tomography Use in the Acute Care Setting. Acad Emerg Med Off J Soc Acad Emerg Med 2015; 22:1465–1473. [DOI] [PubMed] [Google Scholar]
- 5.Smith MP, Katz DS, Lalani T, et al. : ACR Appropriateness Criteria® Right Lower Quadrant Pain--Suspected Appendicitis. Ultrasound Q 2015; 31:85–91. [DOI] [PubMed] [Google Scholar]
- 6.Repplinger MD, Levy JF, Peethumnongsin E, et al. : Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging JMRI 2016; 43:1346–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duke E, Kalb B, Arif-Tiwari H, et al. : A Systematic Review and Meta-Analysis of Diagnostic Performance of MRI for Evaluation of Acute Appendicitis. Am J Roentgenol 2016; 206:508–517. [DOI] [PubMed] [Google Scholar]
- 8.Pooler BD, Lawrence EM, Pickhardt PJ: Alternative diagnoses to suspected appendicitis at CT. Radiology 2012; 265:733–742. [DOI] [PubMed] [Google Scholar]
- 9.Repplinger MD, Pickhardt PJ, Robbins JB, et al. : Prospective Comparison of the Diagnostic Accuracy of MR Imaging versus CT for Acute Appendicitis. Radiology 2018:171838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kinner S, Repplinger MD, Pickhardt PJ, Reeder SB: Contrast-Enhanced Abdominal MRI for Suspected Appendicitis: How We Do It. Am J Roentgenol 2016; 207:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziegler A: Generalized Estimating Equations New York: Springer-Verlag; 2011. [Lecture Notes in Statistics] [Google Scholar]
- 12.Leeuwenburgh MMN, Wiezer MJ, Wiarda BM, et al. : Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simple from perforated appendicitis. Br J Surg 2014; 101:e147–155. [DOI] [PubMed] [Google Scholar]
- 13.Cobben L, Groot I, Kingma L, Coerkamp E, Puylaert J, Blickman J: A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol 2009; 19:1175–1183. [DOI] [PubMed] [Google Scholar]
- 14.Kinner S, Pickhardt PJ, Riedesel EL, et al. : Diagnostic Accuracy of MRI Versus CT for the Evaluation of Acute Appendicitis in Children and Young Adults. AJR Am J Roentgenol 2017; 209:911–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leeuwenburgh MMN, Wiarda BM, Bipat S, et al. : Acute appendicitis on abdominal MR images: training readers to improve diagnostic accuracy. Radiology 2012; 264:455–463. [DOI] [PubMed] [Google Scholar]
- 16.Pooler BD, Repplinger MD, Reeder SB, Pickhardt PJ: MRI of the Nontraumatic Acute Abdomen: Description of Findings and Multimodality Correlation. Gastroenterol Clin North Am 2018; 47:667–690. [DOI] [PubMed] [Google Scholar]
- 17.Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ: Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med 2011; 154:789–796, W-291. [DOI] [PubMed] [Google Scholar]