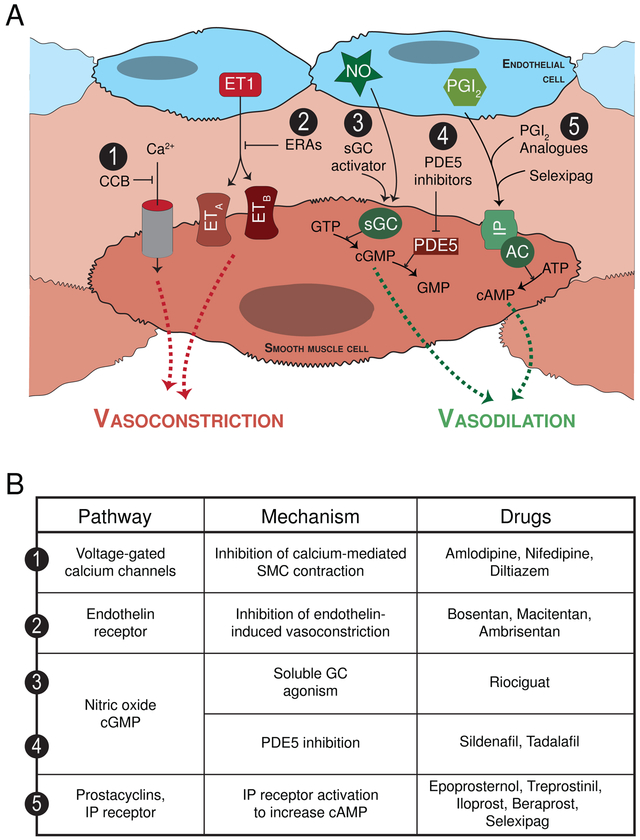
Figure 1.
(A) Current PAH-specific therapies target four molecular pathways all of which are directed at vasodilating the pulmonary vasculature. (1) Calcium channel blockers: The calcium channel blockers amlodipine, nifedipine and diltiazem all block calcium entry into vascular smooth muscle cells (SMC) thereby preventing SMC contraction and pulmonary vasoconstriction. Unfortunately, this class of medications is only effective in <10% of PAH patients, and long-term responses often limited. (2) Endothelin pathway: Endothelin acts through its endothelin A and B receptors (ETA and ETB, respectively) to cause vasoconstriction as well as SMC proliferation. Bosentan and macitentan are both dual endothelin receptor anatagonists (ERA), while ambrisentan is a selective endothelin receptor A antagonist. (3) Nitric oxide pathway: Nitric oxide (NO) is a vasodilator that signals through soluble guanylate cyclase (sGC), which generates cyclic guanosine monophosphate (cGMP) and causes pulmonary artery SMC relaxation. The cGMP is subsequently degraded by phosphodiesterases (PDE). Accordingly, the (3) direct sGC stimulator riociguat and the (4) PDE5 inhibitors sildenafil and tadalafil drive the NO pathway to enhance vasodilation. The use of inhaled nitric oxide is currently reserved for the intraoperative and intensive care unit acute management of pulmonary hypertension treatment. (5) Prostacyclin pathway: Prostacyclin and prostanoids bind the IP receptor to stimulate cyclic adenosine monophosphate, which in turn causes pulmonary vasodilation. Various preparations of prostanoids are available and can be administered via different routes including continuous infusion intravenously or subcutaneously, by inhalation, and orally. The prostanoids include epoprosternol, treprostinil, iloprost and beraprost. Selexipag, in contrast, is the first non-prostanoid IP receptor activator. (B) Currently approved PAH-specific medications with their respective pathway target and mechanism of action.