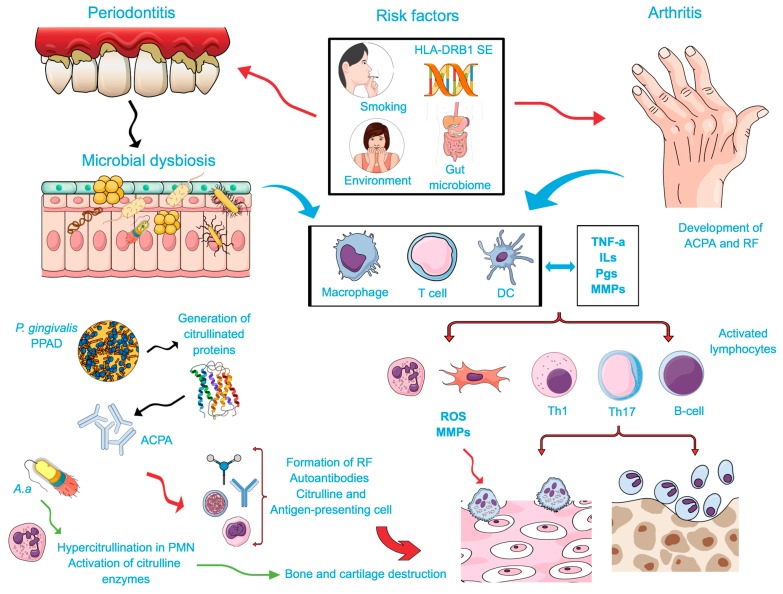
Figure 1.
Possible biological intersections between rheumatoid arthritis (RA) and periodontal disease (PD): Common risk/predisposing factors and reciprocal biological influences. The exposure to certain environmental factors, e.g., smoking, genetic background (HLA-DRB1-SE), gut microbiome, infection with P. gingivalis and more recently with A. actinomycetemcomitans (microbial dysbiosis) leads to local protein alteration by citrullination. In combination with an inflammatory process stimulated by macrophages, dendritic cells, and T cells, a host response to citrullinated proteins in predisposed patients will occur. Immune cells will produce proinflammatory mediators (Interleukins (ILs), Prostaglandins (PGs), Tumor Necrosis Factor (TNF), and metalloproteinases (MMPs), which also contribute to the aggravation of the immune response. IL-17, an important cytokine of the Th17 induces the production of CXC chemokines, MMPs, and reactive oxygen species (ROS), as well as the osteoblast expression of the receptor activator of the factor nuclear kappa B ligand (RANK-L) that stimulate osteoclast activation. Stimulated lymphocytes (B and T cells, specifically Th1 and Th17) play an important function during bone resorption by means of the RANKL-dependent mechanism in both conditions. P. gingivalis infection lead to the activation of proteases and peptidylarginine deiminase (PPADs) that generates citrullinated proteins and triggers the synthesis of anti-citrullinated proteins antibodies (ACPAs). A resultant signal against citrullinated epitopes in the joints resulting in enhanced expression of the rheumatoid factor (RF) and ACPAs, assisting in the formation of immune complexes. A. actinomycetemcomitans lead to the hypercitrullination of neutrophils and result in the activation of citrulline enzymes, which are also involved in the breakdown of the immune tolerance to the host molecules. These immune complexes enhance the host inflammatory development, which may aggravate RA. In addition, the autoantibodies produced during this process might contribute to the inflammatory process by directly activating osteoclast and resulting in the bone and cartilage damage. Thus, citrullination may represent a biological mechanism bridging reciprocal influences between RA and PD.