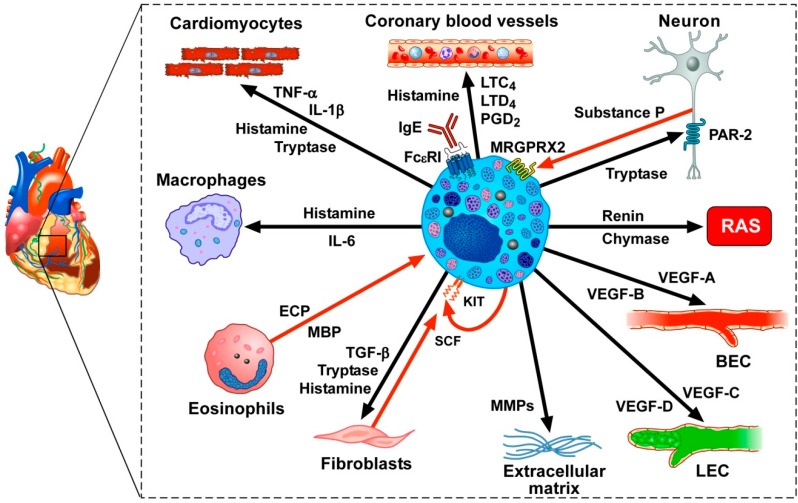
Figure 2.
In the human heart, mast cells are located in the myocardium, in atherosclerotic plaques, in close proximity to nerves and in the aortic valve. The density of myocardial mast cells is increased following myocardial infarction [219] and in patients with cardiomyopathies [204]. Several vasoactive mediators that can be released by activated cardiac mast cells (i.e., histamine, PGD2, LTC4, LTD4) exert profound hemodynamic effects on human coronary blood vessels [220,221,222]. Cardiac mast cells often are in close proximity to sensory nerve fibers. Tryptase can activate the PAR-2 receptor on sensory nerve fibers which can release the neuropeptide substance P [223], which, in turn, can activate the adventitial mast cells [206], presumably through the engagement of the Mas-related G-protein-coupled receptor member X2 (MRGPRX2). Human cardiac mast cells contain and release renin and chymase that cleave angiotensinogen and angiotensin I (ANG I), respectively to form ANG II, thus potentially participating in the homeostatic control of the cardiac renin-angiotensin system (RAS) [224,225]. Immunologically-activated human cardiac mast cells release angiogenic (VEGF-A and VEGF-B) and lymphangiogenic factors (VEGF-C) [66,226,227], which can act on blood endothelial cells (BECs) and lymphatic endothelial cells (LECs), respectively. Matrix metalloproteinases (MMPs) released from mast cells can contribute to extracellular matrix remodeling leading to cardiac fibrosis [228]. Tryptase, TGF-β, and histamine activate fibroblasts to produce collagen [228,229]. Fibroblasts also produce stem cell factor (SCF), the main growth and differentiating factor for mast cells that acts via the engagement of the KIT receptor [8]. Human myocardial mast cells contain and release SCF, which might represent an autocrine factor sustaining mast cell hyperplasia in cardiac disorders [204]. Eosinophils and eosinophil granule proteins (i.e., eosinophil cationic protein (ECP) and major basic protein (MBP)) have been detected in endomyocardial biopsies from patients with hypereosinophilia [230,231]. ECP and MBP can induce the release of proinflammatory mediators from human cardiac mast cells [159]. Human cardiac mast cells interact with macrophages through the release of histamine and IL-6 (Marone, unpublished results). Mast cell tryptase modulates cardiomyocyte contractility through the engagement of the PAR-2 receptor [219]. Histamine, tryptase, TNF-α, and IL-1β can modulate several functions of cardiomyocytes [219,232]. Finally, heterogeneous and ontogenetically diverse macrophages reside in the healthy heart, and accumulate in increased numbers in diseased hearts [233].