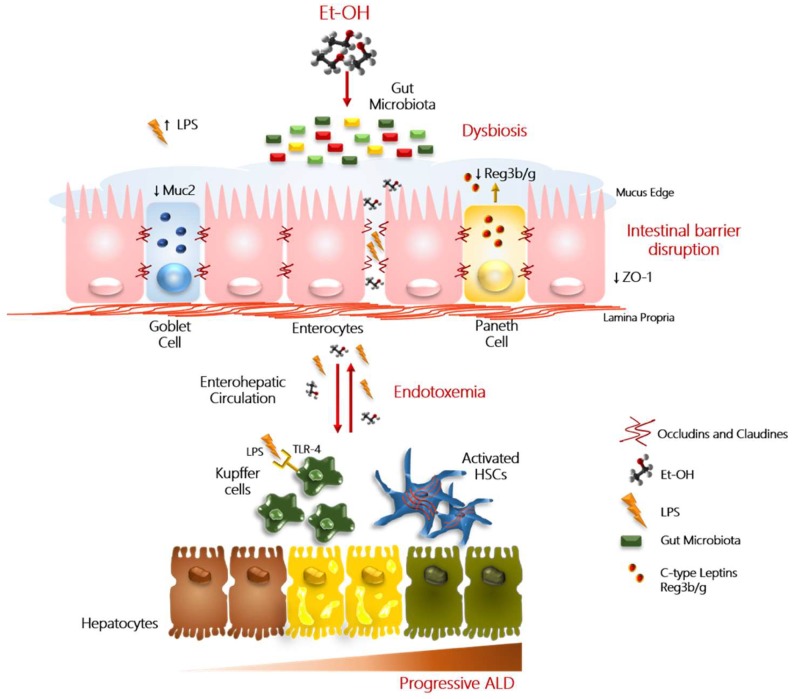
Figure 1.
Role of ‘leaky gut’ in progressive ALD. In this figure, we reported a schematic illustration of the main alterations that contribute to alcohol-induced liver injury. Excessive alcohol abuse (Et-OH) exerts a direct detrimental effect on the intestinal barrier integrity by affecting the tight junction protein (i.e., zonula occludens 1 (ZO-1)) expression and mucus layer. Physiologically, mucus (Muc2) is produced by the goblet cells, instead, the Paneth cells (immune cells) secrete antimicrobial peptides (i.e., c-lectin Reg3b/g), that contribute to maintain the inter-species bacterial balance. Alteration in quality/quantity of microflora taxonomic composition (referred to as ‘dysbiosis’) may trigger the dysfunction of barrier properties and enhance intestinal permeability. The hyperpermeability facilitates the translocation into the enterohepatic circulation of viable pathogenic bacteria, Gram-negative microbial products, mainly lipopolysaccharides (LPS). LPS, peptidoglycans, and β-glucans bind Toll-like receptor 4 (TLR4)/CD14 complex, TRL2, and C-type lectin-like receptor (CLEC7A), respectively, and mediate the activation of hepatic Kupffer cells and peripheral blood mononuclear cells (PBMCs), via NF-κB and IL6/STAT3 signaling. Activated Kupffer cells and PBMCs, in turn, release a large amount of pro-inflammatory cytokines and chemokines (such as TNFα and IL1β), further perpetuating the hepatic inflammation and oxidative stress in the context of already damaged hepatocytes. These events can even contribute to the worsening of hepatic injury to advance stages, favoring also the activation of hepatic stellate cells (HSCs), involved in fibrogenic processes.