Abstract
Background
Approximately 40,000 newborns die each year in Tanzania. Regional differences in outcome are common. Reviewing current local data, as well as defining potential causal pathways leading to death are urgently needed, before targeted interventions can be implemented
Objective
To describe the clinical characteristics and potential causal pathways contributing to newborn death and determine the presumed causes of newborn mortality within seven days, in a rural hospital setting.
Methods
Prospective observational study of admitted newborns born October 2014–July 2017. Information about labour/delivery and newborn management/care were recorded on data collection forms. Causes of deaths were predominantly based on clinical diagnosis.
Results
671 were admitted to a neonatal area. Reasons included prematurity n = 213 (32%), respiratory issues n = 209 (31%), meconium stained amniotic fluid with respiratory issues n = 115 (17%) and observation for < 24 hours n = 97 (14%). Death occurred in 124 infants. Presumed causes were birth asphyxia (BA) n = 59 (48%), prematurity n = 19 (15%), presumed sepsis n = 19 (15%), meconium aspiration syndrome (MAS) n = 13 (10%) and congenital abnormalities n = 14 (11%). More newborns who died versus survivors had oxygen saturation <60% on admission (37/113 vs 32/258; p≤0.001) respectively. Moderate hypothermia on admission was common i.e. deaths 35.1 (34.6–36.0) vs survivors 35.5 (35.0–36.0)°C (p≤0.001). Term newborns who died versus survivors were fourfold more likely to have received positive pressure ventilation after birth i.e. 4.57 (1.22–17.03) (p<0.02).
Conclusion
Intrapartum-related complications (BA, MAS), prematurity, and presumed sepsis were the leading causes of death. Intrapartum hypoxia, prematurity and attendant complications and presumed sepsis, are major pathways leading to death. Severe hypoxia and hypothermia upon admission are additional contributing factors. Strategies to identify fetuses at risk during labour e.g. improved fetal heart rate monitoring, coupled with timely interventions, and implementation of WHO interventions for preterm newborns, may reduce mortality in this low resource setting.
Introduction
In Tanzania, approximately 40,000 newborns die annually due to three major causes; birth asphyxia (BA), prematurity and presumed infections [1,2]. Approximately half of newborn deaths occur within the first 24 hours, and two thirds by the seventh day [3]. Early newborn deaths result mainly from intrapartum complications and immediate postnatal problems including apnea, meconium and hypothermia, which may be prevented or ameliorated by timely interventions.
BA defined as a 5-minute Apgar score <7 and lack of spontaneous respirations after birth, accounts for approximately 0.7 million global deaths [4]. Specifically, in Tanzania, BA accounts for 27 to 45 percent of neonatal deaths; this range in BA reflects regional differences in the country [2, 5, 6]. Globally, prematurity and its attendant complications is the leading cause of neonatal mortality [5]. In Tanzania, approximately 11 percent of newborns are born premature i.e. <37 weeks but they account for 23–35 percent of newborn deaths [1,2]. While in many resource-replete countries, the lower limit of viability approximates 24 weeks of gestation [7], low-resource countries still struggle to prevent premature deaths even at 28 weeks [8]. Recently, the WHO recommended several interventions including administration of antenatal corticosteroids to women at imminent risk of premature labour, and early initiation of continuous positive airway pressure (CPAP) for newborns with respiratory distress syndrome (RDS), geared towards reducing preterm mortality in low-resource settings [9]. A third leading cause of death are infections, which contribute to anywhere from 10 to 30 percent of newborn mortality in Tanzania [1, 2]. However, the diagnosis of infection is often presumed because blood cultures and other ancillary tool are not consistently obtained. Prior to implementation of any potential intervention current local data are needed, with a specific focus on potential causal pathways leading to mortality, in order to facilitate targeted specific interventions. The objectives of this study were to: (1) determine the presumed causes of newborn mortality in a rural hospital setting, and (2) describe the clinical characteristics and potential causal pathways contributing to newborn death within seven days.
Materials and methods
From October 2014 to July 2017, a prospective observational study was conducted at Haydom, a rural hospital in Northern Tanzania, of consecutively admitted newborns followed until discharge or death within the first seven days. Ethical approval was granted by the National Institute for Medical Research in Tanzania (Ref. NIMR/HQ/R.8a/Vol.IX/1434) and the Regional Committee for Medical and Health Research Ethics in Norway (Ref.2013/110). Informed consent was not required by the ethical committees because the study was descriptive.
HLH has approximately 4500 deliveries annually, which is about 53% of deliveries in the catchment area. Less than 10% give birth in other facilities and the remainder gives birth at home. The hospital provides emergency obstetric services 24 hours a day with a caesarean section rate of 22% [10]. Deliveries and newborn resuscitations were mainly conducted by 18–22 midwives with three shifts. Midwives were trained in Helping Babies Breathe [11] and short ventilation training sessions were conducted on a weekly basis with full HBB refresher training twice yearly. The management of newborns born through meconium stained amniotic fluid (MSAF) focused on clearing the oro-pharynx with a bulb suction, when meconium was present, followed by positive pressure ventilation for the non-breathing infant.
The hospital’s newborn area accommodates 10–15 newborns with one general practitioner in charge of the neonatal ward, supervising intern doctors. Admission criteria include prematurity, 5-minute Apgar score <7, fever (temperature >38°C), signs of respiratory compromise, i.e. intercostal, subcostal retractions or grunting and infants with congenital abnormalities. Premature newborns are nursed under shared radiant warmer and term newborns are nursed in locally made ‘baby cots’. Interventions include intravenous fluids, intravenous antibiotics, oxygen therapy using oxygen concentrators, and phototherapy, as clinically indicated. Stable newborns are allowed to breastfeed, if not, mothers express milk and it is administered either via an oro-gastric tube or via a cup. Stable premature newborns of <1800 grams are nursed skin to skin until they attain a minimum discharge weight of 1800 grams. Provisional diagnoses and presumed causes of death were assigned by the attending doctor during the ward round.
Trained research assistants (n = 14) observed and recorded every delivery in the labour ward and theatre on a data collection form. This form contained antenatal and perinatal information. Information related to admitted newborns was captured using a second data collection form. Inclusion criteria were all newborns delivered at HLH and were alive at the time of admission to the newborn area. Exclusion criteria included: all newborns delivered outside HLH, and newborns who died in the delivery room within 30 minutes of birth. Newborns who died in the delivery room were excluded as they have been reported previously [12]. More specific definitions are noted in Table 1.
Table 1. Specific definitions used to define conditions.
| Definition | |
|---|---|
| Gestational age | Self-report of the last normal menstrual period and distance measured from symphysis pubis to the fundus |
| Prematurity | Gestational age <37 weeks |
| Low birth weight | Birth weight <2500 grams. |
| Presumed Neonatal sepsis | One or more clinical signs of bacterial infection: pallor, poor perfusion, bradycardia, apnea, tachypnea (>60 breaths/minute), dyspnoea (grunting, nasal flaring, retractions), temperature instability (≥38°C or <36°C), difficulty feeding and distended abdomen. |
| Pneumonia | Difficulty in breathing, tachypnea (respiratory rate >60 breaths/minute) without history of birth asphyxia. |
| Birth asphyxia | 1) Failure to initiate spontaneous breathing and/or 5-minute Apgar score <7 in addition to clinical evidence of encephalopathy. 2) Gestational age <32 weeks with a history of suspected intrapartum related hypoxia (abnormal fetal heart rate, labour complications, no respiratory efforts or the need for positive pressure ventilation) |
| Respiratory distress syndrome | Considered in a preterm baby with chest retractions within two hours after delivery with exacerbation over the first 24–48 hours of life, followed by a stable phase till 72 hours, then improvement between the 3rd and 6th day. |
| Meconium aspiration syndrome | Onset of respiratory distress immediately after birth or few hours, with history of meconium stained amniotic fluid, meconium around the oro-pharynx or meconium stained skin. |
| Meconium stained amniotic fluid | Amniotic fluid stained with thick meconium |
| Hypoxic-ischaemic encephalopathy | Clinical diagnosis characterized as mild, moderate and severe using the Thompson scoring system |
Initial management of admitted newborns
Management of newborns followed the principles outlined in the WHO Essential Newborn Care guidelines which included routine administration of intramuscular Vitamin K injection (1 mg stat for term and 0.5 mg for preterm) to all admitted newborns [13]. Axillary temperature and blood glucose measurements were obtained using a digital thermometer and commercial glucometer, respectively, within 30 minutes of admission. Hypoglycemia, defined as blood glucose below 2.5 mmol/L [14], was treated with intravenous bolus 3 mls/kg 10% dextrose followed by feeding or maintenance with 10% dextrose. Seizures were treated with intravenous phenobarbital at a loading dose of 20 mg/kg, followed by maintenance dose of 5 mg/kg/day. Newborns with history of BA were categorized clinically as either mild, moderate and severe hypoxic ischaemic encephalopathy using the Thompson scoring system [15]. Antibiotics (ampicillin 50 mg/kg/day and gentamycin 4 mg/kg/day) were given to at risk newborns, i.e. premature newborns, infants with presumed MAS and/or BA, for at least 48 hours because of the inability to exclude infections. If sepsis was suspected based on clinical signs [16, 17], the antibiotics were changed to ceftriaxone 50 mg/kg/day for 10 days. Continuous positive airway pressure (CPAP) and intubation was not available to assist infants with respiratory difficulty. Radiological investigations such as chest x-rays and cranial ultrasounds were infrequently obtained because of difficulties transporting unstable newborns to the radiology department. Blood cultures, full blood counts and C-reactive protein measurements were rarely available.
Data analysis
The Chi-square or Fisher exact test was used to test for differences between categorical variables, as appropriate. The Mann-Whitney U test was used to test for differences between groups for continuous variables when test for normality showed that the data where not normally distributed. Logistic regression was used for modelling the impact of risk factors for death among admitted newborns. First a stepwise backward selection method with the retention of predictors with p<0.05 was used, and afterwards excluded variables were re-entered one by one and kept if found significant. The results are presented as Odds Ratio (OR) with 95% confidence intervals (CIs). Variables obtained on initial assessment during admission were not used because of missing data. Statistical analyses were performed using SPSS (IBM SPSS Statistics for Windows, version 22.0; IBM Corp., Armonk, N.Y. USA).
Results
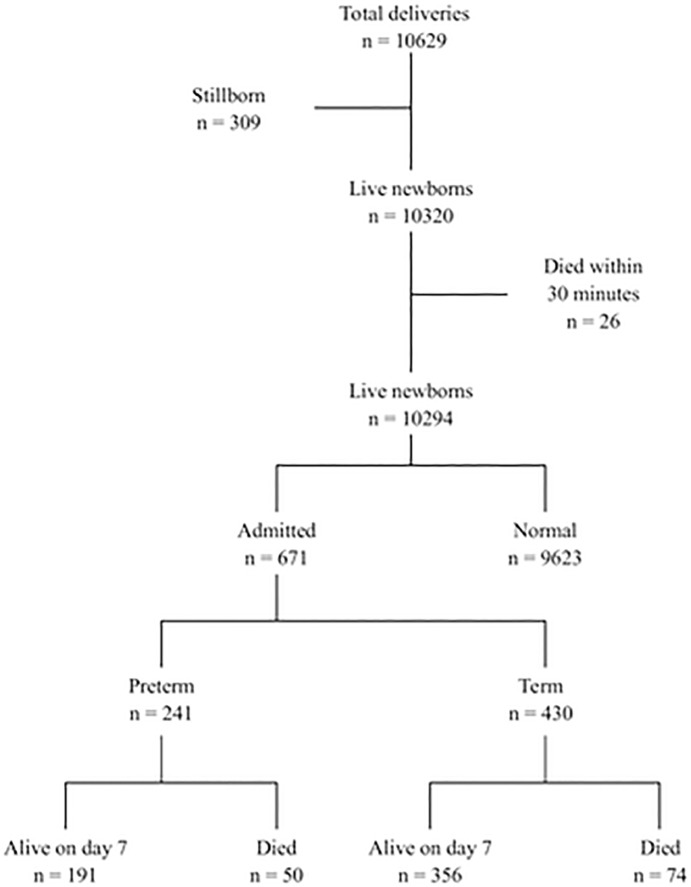
During the study period, there were 10629 deliveries, 10320 were live newborns of birth weight 3311±529 grams and GA 38.8±1.8 weeks, 309 were stillborn and 26 newborns died within 30 minutes (the latter newborns died from BA) [12]. Of the remaining 10294 newborns, 9623 were normal and stayed with the mother, and 671 were admitted to the neonatal area (Fig 1). Of the admitted newborns, a total of 124/671 (18%) died within seven days; of these 61 (49%) within 24 hours, an additional 38 (31%) within 72 hours and 25 beyond 72 hours of life.
Fig 1. Flow diagram of newborn delivered and outcome after 7 days.
Delivery room management (n = 10320)
At delivery 2785/10320 (27%) were stabilized with stimulation and/or suctioning and 691 (6.7%) of these newborns were ventilated immediately after delivery. MSAF was present in 2561 (25%) of all live newborns.
Characteristics of admitted newborns (n = 671)
Of the 671 admissions, 241 (36%) were premature and 297 (44%) were of low birth weight. A total of 314 (46%) of the admitted newborns were ventilated in the delivery room; of these 17% were premature. Reasons for admission included complications of prematurity n = 213 (32%), respiratory issues n = 209 (31%), MSAF with respiratory issues n = 115 (17%), infants admitted for observation <24 hour (e.g. post-caesarean section, infants with weight above 3.8 kg) n = 97 (14%), and other indication 37 (5%).
Presumed causes of death (n = 124)
The presumed causes of death included BA (n = 59), complications related to MSAF (n = 13), prematurity (n = 19), presumed/suspect infection (n = 19) and secondary to complication related to congenital anomalies (n = 14). Each is briefly reviewed below:
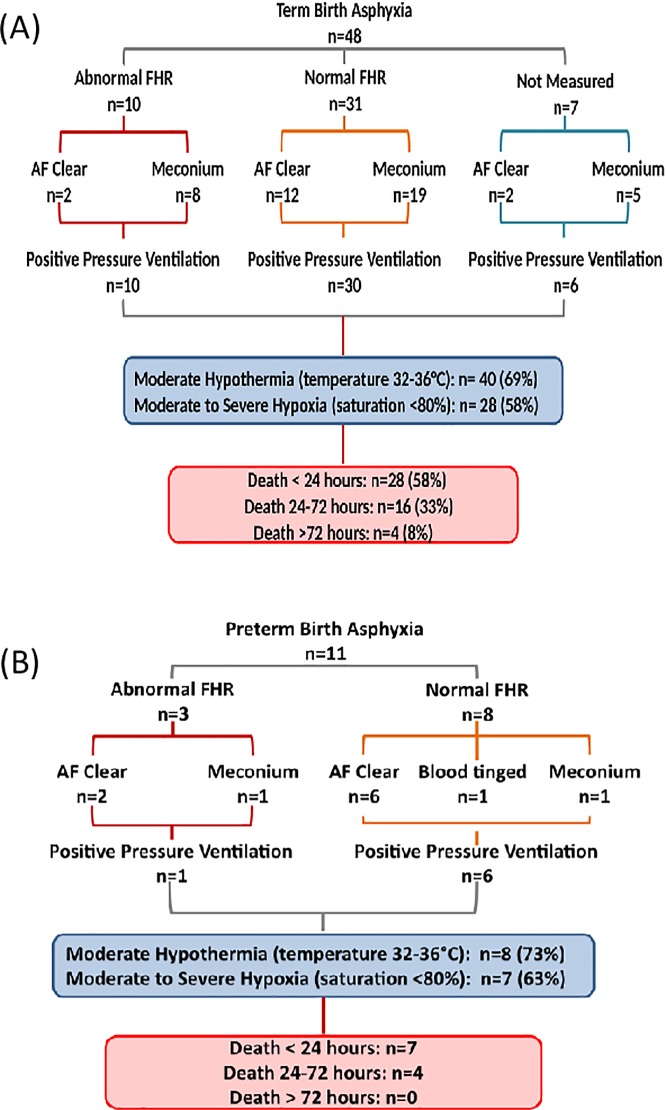
1. BA (n = 59) (47%) was the leading cause of death which included 11 (22%) premature newborns (Fig 2). Labour was complicated by an abnormal fetal heart rate in 13 (22%) cases. In 7(12%) the foetal heart rate was not measured. Delivery was via emergency caesarean section in 30 (51%) cases and in 34 (58%) there was associated MSAF (Fig 2). Positive pressure ventilation was applied in the delivery room in 54 (92%) newly borns. Upon admission to the neonatal ward, moderate hypothermia (temperature 32–36°C) was noted in 40 (69%) and moderate to severe hypoxia (saturation <80%) in 28 (58%) newborns (Fig 2). Hypoxic-ischemic encephalopathy (HIE) developed in 28 (48%) newborns, was severe in 17 (29%) and moderate in 11 (19%) of these newborns. Seizures were noted in 16 (27%) newborns. Death occurred within 24 hours in 35 (60%), and between 24 and 72 hours in 16 (33%) newborns.
Fig 2. Perinatal characteristics, hypothermia and hypoxia and timing of death in infants with birth asphyxia.
(A) Term infants. (B) Preterm infants. Abbreviations: FHR, foetal heart rate; AF, amniotic fluid.
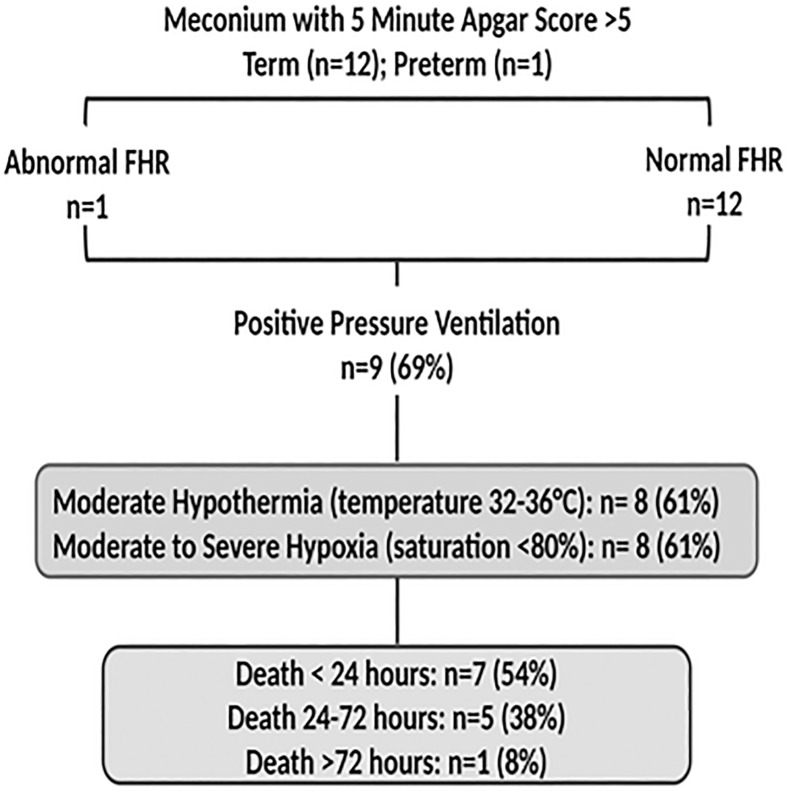
2. MSAF was present in 254/671 (38%) of newborns; 122 (48%) cases were categorized as thick. There were 51 (20%) newborns with MSAF who died including 34 (13%) with BA (see above), 4 newborns with presumed/suspect sepsis and 13 (5%) additional newborns who died secondary to presumed MAS (Fig 3). For the latter newborns, the fetal heart rate during labour was normal in 12 (92%) cases. The MSAF was categorized as thick (n = 9) (69%) and delivery was via emergency CS in 9 (69%) cases. Positive pressure ventilation was applied in 9 (69%) and the 5-minute Apgar score was > 7 in all 13 newly borns. Moderate hypothermia was noted in 8/13 (61%) and moderate to severe hypoxia in 8 (61%) newborns. Death occurred within 24 hours in 7 (54%) and between 24 and 72 hours in 5 (38%) newborns.
Fig 3. Perinatal characteristics, presence of hypothermia and hypoxia in infants with meconium aspiration syndrome.
Abbreviations: FHR, foetal heart rate.
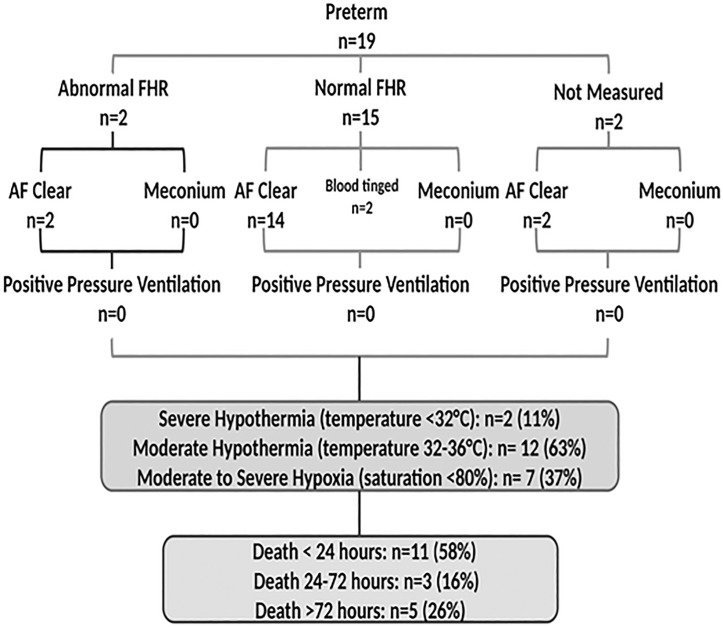
3. Prematurity and its attendant complications contributed to 19 (15%) of all newborn deaths. Upon admission, all 19 had a normal foetal heart rate and the heart rate continued to be normal during labour in 17/19 cases; in 2 cases the foetal was not measured (Fig 4). Delivery was vaginal in 14 (74%) and via emergent caesarean section in 4 (21%) newborns. No newborn received positive pressure ventilation in the delivery room. Moderate to severe hypothermia was noted in 14 (74%) and moderate to severe hypoxia in 7 (37%) newborns. Complications of prematurity that led to death included respiratory distress syndrome (n = 11) (including 8 who died within 72 hours), recurrent apnoea (n = 2), necrotizing enterocolitis (n = 1), haemorrhage due to presumed Vitamin K deficiency (n = 1) and two newborns admitted with severe hypothermia (temperature <32⁰C). Death occurred within 24 hours in 11 (58%), between 24 and 72 hours in 3 (16%) and beyond 72 hours in 5 (26%) newborns.
Fig 4. Perinatal characteristics, presence of hypothermia and hypoxia and timing of death in preterm infants.
Abbreviations: FHR, foetal heart rate; AF, amniotic fluid.
4. Presumed/ suspect sepsis contributed to 19 (15%) deaths; 16 (84%) were premature. The foetal was normal in 15 (94%) neonates; in 3 cases the heart rate was not measured (Fig 5). Positive pressure ventilation was applied in 5 (26%) newly borns and in all cases the 5-minute Apgar score was ≥7. Moderate to severe hypothermia was noted in 12 (63%) and moderate to severe hypoxia in 11 (58%) newborns. Three of the newborns had presumed pneumonia. Death occurred within 24 hours in 1 (5%), between 24 and 72 hours in 4 (21%) and beyond 72 hours in 14 (74%) newborns.
Fig 5. Perinatal characteristics, hypothermia and hypoxia and timing of death in infants with presumed/suspect sepsis.
Abbreviations: FHR, foetal heart rate; AF, amniotic fluid.
5. Congenital abnormalities (n = 14) were associated with early deaths. These included presumed congenital heart disease (n = 3), anencephaly (n = 1), gastroschisis (n = 1), presumed congenital Rubella syndrome (n = 1), trachea-oesophageal fistula (n = 1), prune belly syndrome (n = 1), Hydrops fetalis (n = 1) and Down syndrome (n = 1). Four newborns had dysmorphic features which could not be linked to a definitive syndrome.
Characteristics of newborns who died versus survivors
Newborns who died (n = 124) compared to those who survived (n = 547), were more likely to be male (p = 0.019), have a lower 1-minute (p = 0.01) and 5-minute Apgar score <7 (p = 0.001), have a lower admission temperature (p<0.001), lower oxygen saturation (p<0.001), more likely to receive supplemental oxygen administration (p<0.001), and higher random blood glucose levels (p = 0.04) (Table 2). Mode of delivery and indication for caesarean section were the same between those who died and survivors.
Table 2. Comparison of perinatal characteristics among newborns who died versus survivors within first 7 days.
| Dead n = 124 |
Survived n = 547 |
P-value | |
|---|---|---|---|
| Birth weight (grams) (IQR) | 2522 (1740–3010) | 2640 (1930–3200) | 0.07a |
| Gestational age (weeks) (IQR) | 37 (32–40) | 37 (34–40) | 0.55 a |
| Antenatal care attendance | |||
| Yes | 122 (98) | 539 (99) | |
| No | 2 (2) | 7 (1) | 0.77c |
| Antenatal complications | |||
| Yes | 6 (5) | 30 (5) | |
| No | 118 (95) | 516 (95) | 0.67b |
| FHR during labour | |||
| Normal | 92 (75) | 424 (78) | |
| Abnormal/not detected | 16 (13) | 60 (11) | |
| Not measured | 15 (12) | 62 (11) | 0.76b |
| Amniotic fluid colour | |||
| Normal | 69 (56) | 333 (61) | |
| Meconium stained | 52 (42) | 202 (37) | |
| Blood stained | 3 (2) | 12 (2) | 0.56b |
| Obstetric complication | |||
| Yes | 16 (13) | 81 (15) | |
| No | 108 (87) | 465 (85) | 0.58b |
| Mode of delivery | |||
| Vaginal | 71 (58) | 335 (61) | |
| Caesarean section | 52 (42) | 211 (39) | 0.10b |
| Gender | |||
| Male | 76 (61) | 286 (52) | |
| Female | 47 (39) | 260 (48) | 0.019b |
| PPV attempted | |||
| Yes | 73 (59) | 241 (44) | |
| No | 51 (41) | 306 (67) | 0.003b |
| Apgar score at 1 minute | |||
| <7 | 69 (56) | 178 (33) | |
| ≥7 | 55 (44) | 369 (67) | 0.001b |
| Apgar score at 5 minute | |||
| <7 | 39 (32) | 48 (9) | |
| ≥7 | 85 (68) | 499 (91) | <0.001b |
| Oxygen saturation on admission | |||
| <60% | 37 (33) | 32 (12) | |
| 60–89% | 52 (46) | 94 (36) | |
| ≥90% | 24 (21) | 132 (51) | <0.001 |
| Initial assessment on admission | |||
| Temperature (C) | 35.1 (34.6–36.0) | 35.5 (35.0–36.0) | <0.001a |
| Heart rate (beats/minute) | 143 (130–158) | 140 (130–154) | 0.48a |
| Need for oxygen therapy (n) | 93 (92) | 132 (46) | <0.001b |
| Random blood glucose (mmol/l) | 4.2 (2.4–5.5) | 3.5 (2.3–4.6) | 0.04a |
Data are presented as n (%) unless otherwise stated
FHR, fetal heart rate; C, Celsius; PPV, positive pressure ventilation
a Mann-Whitney
b Chi-square
cFisher-exact test
Additional analysis of term newborns only (excluding congenital malformations) was performed. Term newborns who died (n = 63) compared to those who survived (n = 353), were more likely to have thick meconium (p<0.001), have a 5 minute Apgar score <7 (p<0.001), have received positive pressure ventilation in the delivery room (p<0.001) and have severe hypoxia during admission (p<0.001) (Table 3).
Table 3. Comparison of perinatal characteristics among term newborns who died versus survivors within first 7 days.
| Dead | Survived | P-valuea | |
|---|---|---|---|
| n = 63 | n = 353 | ||
| FHR during labour (n = 382) | |||
| Normal | 45 (80) | 285 (87) | |
| Abnormal/not detected | 11 (20) | 41 (13) | 0.115 |
| Amniotic fluid colour (n = 306) | |||
| Normal | 17 (38) | 173 (66) | |
| Thick meconium stained | 28 (62) | 88 (34) | <0.001 |
| Apgar score at 5 minute (n = 416) | |||
| <7 | 33 (52) | 38 (11) | |
| ≥7 | 30 (48) | 315 (89) | <0.001 |
| PPV (n = 227) | |||
| <60% | 22 (39) | 21 (12) | |
| 60–89% | 19 (34) | 66 (39) | |
| >90% | 15 (27) | 84 (49) | <0.001 |
| HIE score | |||
| Mild | 11 (30) | 102 (94) | |
| Moderate | 9 (24) | 7 (6) | |
| Severe HIE | 17 (46) | 0 (0) | <0.001b |
Data is presented as n (%) unless otherwise stated
FHR, fetal heart rate; PPV, positive pressure ventilation; HIE, hypoxic ischemic encephalopathy
aChi-square test unless stated otherwise
bFisher-exact test
Logistic regression model of independent predictors of death for all admitted newborns and a subgroup of term newborns (excluding newborns with congenital malformations) is shown in Tables 4 and 5.
Table 4. Logistic regression model of independent predictors of death among all admitted newborns.
| Variables | Bivariate analysis | P-value | Multivariable analysis with all variables into the model | P-value | Multivariable analysis after backward LR elimiation | P-value |
|---|---|---|---|---|---|---|
| OR (95%CI) | AOR (95%CI) | AOR (95%CI) | ||||
| Gestational age (weeks) | 97 (0.92–1.03) | 0.34 | 0.99 (0.87–1.13) | 0.91 | ||
| Birth weight (kg) | 0.79 (0.62–1.02) | 0.05 | 0.58 (0.31–1.08) | 0.08 | 0.64 (0.48–0.84) | 0.036 |
| Gender | ||||||
| Female | 1 | |||||
| Male | 1.47 (0.98–2.19) | 0.06 | 1.50 (0.96–2.37) | 0.07 | ||
| Foetal heart rate | ||||||
| Normal | 1 | |||||
| Abnormal | 1.30 (0.73–2.34) | 0.36 | 1.20 (0.63–2.36) | 0.55 | ||
| Amniotic fluid colour | ||||||
| Normal | 1 | 1 | ||||
| Thick meconium | 1.43 (0.87–2.36) | 0.15 | 1.48 (0.67–3.26) | 0.33 | ||
| PPV attempted | ||||||
| No | 1 | 1 | ||||
| Yes | 1.81 (1.22–2.69) | 0.003 | 1.49 (0.68–3.24) | 0.31 | ||
| Apgar score 5 minute | ||||||
| ≥7 | 1 | 1 | 1 | |||
| <7 | 4.76 (2.94–7.70) | <0.001 | 2.81 (1.17–6.70) | 0.020 | 3.20 (1.42–7.22) | 0.005 |
| Oxygen saturation on admission | ||||||
| ≥90% | ||||||
| 60–89% | 3.04 (1.75–5.28) | 3.06 (1.47–6.41) | 0.003 | 3.10 (1.50–6.43) | 0.002 | |
| <60% | 6.36 (3.34–12.10) | 4.53 (1.92–10.71) | 0.001 | 4.73 (2.02–11.13) | 0.001 |
PPV, positive pressure ventilation; OR, odds ratio; AOR, adjusted odds ratio; CI, confidence interval; LR, logistic regression. Temperature not included in the model because of missing data
Table 5. Logistic regression model of independent predictors of death among term admitted newborns (excluding congenital malformations).
| Variables | Bivariate analysis OR (95%CI) | P-value | Multivariable analysis with all variables into the model | P-value | Multivariable analysis after backward LR elimination | P-value |
|---|---|---|---|---|---|---|
| AOR (95%CI) | AOR (95%CI) | |||||
| Foetal heart rate | ||||||
| Normal | 1 | 1 | ||||
| Abnormal | 1.69 (0.81–3.54) | 0.15 | 1.12 (0.35–3.53) | 0.84 | ||
| Amniotic fluid colour | ||||||
| Normal | 1 | 1 | ||||
| Thick meconium | 3.24 (1.68–6.23) | <0.001 | 2.36 (0.95–5.86) | 0.063 | ||
| Apgar score 5 minute | ||||||
| ≥7 | 1 | 1 | ||||
| <7 | 9.11 (5.01–16.58) | <0.001 | 3.74 (1.44–9.68) | 0.006 | 3.61 (1.67–7.81) | 0.001 |
| PPV | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 7.35 (3.09–17.49) | <0.001 | 4.58(1.23–17.06) | 0.023 | 4.00 (1.40–11.44) | 0.010 |
| Oxygen saturation | ||||||
| <60% | 5.8 (2.61–13.21) | <0.001 | 3.7 (1.24–11.10) | 0.019 | 4.60 (1.82–11.65) | 0.001 |
PPV, positive pressure ventilation; OR, odds ratio; AOR, adjusted odds ratio; CI, confidence interval; LR, likelihood ratio.
An Apgar score <7 at 5 minutes (p = 0.005), oxygen saturation on admission (p = 0.001) and birth weight (p = 0.036) were associated with increased odds of death in the final model for all admitted neonates. Temperature was not included in the model because of missing data points (Table 4). The odds of dying versus survival increased 4.5 fold (p = 0.010) with positive pressure ventilation, 3.6 fold (p = 0.006) with a 5 minute Apgar Score <7, and 4.6 fold (p = 0.001) with an admitted saturation <60% among term newborns (Table 5).
Discussion
This report highlights the major contributors of neonatal mortality in a low resource rural setting in Northern Tanzania. The findings are consistent with prior reports indicating that BA is the commonest cause of death, with prematurity and its attendant complications, presumed/suspect sepsis, MAS and congenital abnormalities as other important contributing factors. In addition, term newborns who died were 3.7 old more likely to have received positive pressure ventilation in the delivery room, 3.6 fold more likely to have an initial saturation <60% and more likely to present with moderate hypothermia upon admission to the neonatal unit compared to term survivors.
BA and MAS, which were associated with 58% of all deaths, represent intrapartum related complications, likely resulting from interruption of placental blood flow. This number is underrepresented in the present study, due to exclusion of newborns who died in the delivery room within 30 minutes of birth, presumed to be associated with BA [12]. Potential pathways contributing to death in this group included severe hypoxia and moderate to severe hypothermia noted upon admission to the neonatal ward. The severe hypoxia may reflect poor respiratory effort secondary to evolving brain injury (approximately 50% presented with moderate to severe encephalopathy), ventilation/perfusion mismatch (possibly related to MAS or moderate hypothermia) or myocardial dysfunction (possibly related to hypoxia ischemia or moderate hypothermia) [18,19,20]. These newborns were much more likely to evolve to moderate to severe encephalopathy with seizures noted in 30% of cases. The constellation of these clinical findings in the newborns with BA likely contributed to their early death within the first 24 hours, in most infants.
MAS contributed to 10% of all presumed causes of death, which is also higher when compared to the 1.5 to 5% from previous reports [6, 21]. This may represent an over diagnosis due to the inability to obtain chest radiographs, and/or to definitely exclude other pulmonary complications such as pneumothorax, congenital pneumonia and/or concurrent infection. This high mortality rate may reflect the absence of continuous end positive pressure (CPAP) and/or mechanical ventilation, as well as an inability to intubate and potentially administer surfactant, interventions which are regarded as standard of care in developed countries [22].
The above findings offer potential opportunities for reducing mortality related to BA and/or MAS. More than half of newborns who died of BA and MAS had a normal foetal heart rate during labour determined intermittently using a fetoscope in most cases. This raises an important question whether these fetuses could have been identified with continuous foetal heart rate monitoring. The more recent availability of a continuous foetal heart rate monitor termed Moyo, may more readily identify high risk fetuses during labor [23,24]. However our group has recently shown while continuous as opposed to intermittent foetal heart rate monitoring results in the detection of more foetal heart rate abnormalities, it does not reduce the time from detection to delivery, suggesting bottlenecks in the system (i.e. lack of operating rooms and/or skilled clinical providers) [23,24]. Post-delivery, more effective resuscitation including the provision of CPAP and/or endotracheal intubation as indicated above, minimizing hypoxia and maintaining temperature in the normal range are basic first step strategies to potentially reduce early mortality [25, 26]. While both the diagnosis of BA i.e. WHO criteria of a 5-minute Apgar <7 in a non-breathing baby, and that of MAS were made clinically, without evidence of severe fetal acidemia (umbilical cord arterial pH <7.00), multiple organ failure [18,27] or radiological confirmation with MAS, we consider the constellation of clinical findings and potential basic interventions as described above, specific enough to have broad generalizability in potentially reducing early mortality.
Globally, preterm births accounts for 25% of all newborn deaths [6]. In this report, prematurity as the primary diagnosis contributed to 15% of neonatal deaths which is lower than prior Tanzanian and global studies [2, 5, 6]. Preterm newborns who died in this study did not have evidence of intrapartum related complications and their delivery room transitional phase was uneventful. However, more than half of the deaths occurred within the first 24 hours. This is most likely attributed to early respiratory distress due to surfactant deficiency, no CPAP, absence of surfactant replacement therapy and further exacerbated by moderate to severe hypothermia noted upon admission to the neonatal unit [28]. Preterm newborns are highly susceptible to infections and the majority of newborns who died of presumed/suspected sepsis were premature; these infants also had an uneventful delivery room transition. Thus, overall when all diagnoses are combined, prematurity contributed to nearly 30% of deaths in this cohort. Adopting WHO recommended interventions such as administration of antenatal corticosteroids to women who are at imminent risk of preterm labour, antibiotic administration to women with preterm premature rupture of membranes, and initiation of CPAP for newborns with RDS, could improve premature mortality in this setting [9]. In a recent publication from Tanzania, Massawe et al. reported a reduction in mortality in premature newborns of gestational age 28 to 34 6/7 weeks, after administration of antenatal corticosteroids and antibiotics, to both the mother and her newborn [29].
The rate of congenital malformation in this report of 11% is in line with WHO worldwide estimates, as well as the estimates in Tanzania of 14% [5, 6]. The contribution of congenital abnormalities to specific causes of death is probably significantly underestimated in this setting, because of the limited resources to screen with chromosomal analysis or more recent techniques such as microarray and to perform an autopsy after death.
Moderate hypothermia has been linked to an increased risk of death in a dose dependent manner [30]. In this cohort, most admitted newborns with measured temperatures were moderately hypothermic, noted in approximately two thirds of those who died. A recent study from Brazil showed that admission hypothermia was significantly associated with early neonatal deaths even in a presence of good quality newborn care [31]. Continuous improvement of thermal care immediately after birth is critically needed. Potential strategies include early skin to skin care immediately after birth [32], the introduction of overhead heaters or plastic wraps in the delivery room [33] and during transfer of newborns.
From the above it should be apparent that strategies to reduce neonatal mortality in the low-resource setting are complex, influenced by many factors. Reducing mortality due to intrapartum complications will require a multiple prong approach, targeting interventions such as enhanced foetal heart rate monitoring coupled with expedited delivery where indicated, as well as optimizing delivery room resuscitation and in particular, focusing on efforts to maintain the warmth of the newly born. The perinatal management of newborns who are born through thick MSAF requires further study in low-resource countries, with efforts directed towards enhancing respiratory support i.e. CPAP.
The findings of this study should be interpreted cautiously. First, this was a single center study with many resource limitations. Second, this study only included inborn neonates in an area where admitted outborn births are primarily premature neonates, who contribute considerably to mortality in this setting. Third, the challenges of accurate diagnosis without laboratory or radiological studies were substantial, and diagnosis relied mostly on the clinical acumen of the practitioner. Furthermore, postmortem examination to confirm causes of deaths is rare in this setting.
Conclusion
Intrapartum related complications such as BA and MAS contributed to almost two thirds of the deaths, with prematurity and presumed/suspect sepsis additional important causes. Intrapartum complications and prematurity are the main pathways leading to death in this rural setting. Hypothermia likely played a significant role in increasing mortality in this setting. Strategies to identify fetuses at high risk of intrapartum hypoxia/ischemia, coupled with timely interventions should be a priority in this setting. Implementation of WHO recommended interventions for improving preterm outcome, including improving thermal control and enhancing basic diagnostics such as completed blood count, C-reactive protein and imaging studies is critical to facilitate targeted interventions.
Supporting information
(SAV)
Acknowledgments
The authors would like to acknowledge research assistants and all staff at Haydom Global Health Research Centre who made this study possible.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was funded by the Laerdal Foundation and the Global Health and Vaccination Research (GLOBVAC) program at the Research Council of Norway (project number 228203). The external funding sources had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the paper for publication.
References
- 1.Tanzania Demographic Health Survery and Malaria Indicator. 2015.
- 2.Afnan-Holmes H, Magoma M, John T, Levira F, Msemo G, Armstrong CE, et al. Tanzania’s Countdown to 2015: An analysis of two decades of progress and gaps for reproductive, maternal, newborn, and child health, to inform priorities for post-2015. Lancet Glob Heal. 2015;3: e396–409 [DOI] [PubMed] [Google Scholar]
- 3.Lawn JE, Cousens S, Zupan J. 4 Million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. 10.1016/S0140-6736(05)71048-5 [DOI] [PubMed] [Google Scholar]
- 4.Lawn JE, Blencowe H, Oza S, You D, Lee ACC, Waiswa P, et al. Every newborn: Progress, priorities, and potential beyond survival. Lancet. 2014;384:189–205. 10.1016/S0140-6736(14)60496-7 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Global Health Observatory (GHO): Data Repository GHO; 2018. Available from: http://apps.who.int/gho/data/node.home [Google Scholar]
- 6.Mmbaga BT, Lie RT, Olomi R, Mahande MJ, Kvåle G, Daltveit AK. Cause-specific neonatal mortality in a neonatal care unit in Northern Tanzania: a registry based cohort study. BMC Pediatr. 2012;12:116 10.1186/1471-2431-12-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity-moving beyond gestational age. N Engl J Med. 2008;358:1672–81. 10.1056/NEJMoa073059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Straughn HK, Goldenberg RL, Tolosa JE, Daly S, Codes J De, Festin MR. Birthweight-specific neonatal mortality in developing countries and obstetric practices. Int J Gynaecol Obstet. 2003;80:71–8. 10.1016/s0020-7292(02)00309-0 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. WHO Recommendations on Interventions to Improve Preterm Birth Outcomes. 2015. Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/preterm-birth-guideline/en/%5Cn [PubMed]
- 10.Mdoe PF, Ersdal HL, Mduma E, Perlman JM, Moshiro R, Wangwe PT, et al. Intermittent fetal heart rate monitoring using a fetoscope or hand held Doppler in a rural Tanzania: a randomized controlled trial. BMC Pregnancy Childbirth. 2018;18:134 10.1186/s12884-018-1746-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The American Academy of of Pediatrics. Helping Babies Breathe. 2009. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/helping-babies-survive/Pages/Helping-Babies-Breathe.aspx
- 12.Ersdal HL, Eilevstjønn J, Linde JE, Yeconia A, Mduma ER, Kidanto H, et al. Fresh stillborn and severely asphyxiated neonates share a common hypoxic-ischemic pathway. Int J Gynecol Obstet. 2018;141:171–180. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Maternal, Newborn, Child and Adolescent Health. Essential newborn care. World Health Organization. 2010. http://www.who.int/maternal_child_adolescent/documents/newborncare_course/en/
- 14.Cornblath M, Hawdon JM, Williams AF, Aynsley-Green A, Ward-Platt MP, Schwartz R, et al. Controversies Regarding Definition of Neonatal Hypoglycemia: Suggested Operational Thresholds. Pediatrics. 2000;105:1141–5. 10.1542/peds.105.5.1141 [DOI] [PubMed] [Google Scholar]
- 15.Thompson CM, Puterman AS, Linley LL, Hann M, van der Elst CW, Molteno CD, et al. , The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr, 1997. 86(7): p. 757–61. 10.1111/j.1651-2227.1997.tb08581.x [DOI] [PubMed] [Google Scholar]
- 16.Ohlin A, Björkqvist M, Montgomery SM, Schollin J. Clinical signs and CRP values associated with blood culture results in neonates evaluated for suspected sepsis. Acta Paediatr. 2010;99:1635–40. 10.1111/j.1651-2227.2010.01913.x [DOI] [PubMed] [Google Scholar]
- 17.Griffin MP, Lake DE, O’Shea TM, Moorman JR. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr Res. 2007;61:222–7. 10.1203/01.pdr.0000252438.65759.af [DOI] [PubMed] [Google Scholar]
- 18.Perlman JM, Tack ED, Martin T, Shackelford G, Amon E. Acute Systemic Organ Injury in Term Infants After Asphyxia. Am J Dis Child.1989;143:617–20 10.1001/archpedi.1989.02150170119037 [DOI] [PubMed] [Google Scholar]
- 19.Kiley JP, Eldridge FL, Millhorn DE. The effect of hypothermia on central neural control of respiration. Respir Physiol 1984;58:295–312 10.1016/0034-5687(84)90006-9 [DOI] [PubMed] [Google Scholar]
- 20.Askin D. Newborn adaptation to extrauterine life In: Simpson K. R. & Creehan P. A.. AWHONN’s Perinatal Nursing. (3rd ed). Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- 21.Vain NE, Szyld EG, Prudent LM, Wiswell TE, Aguilar AM, Vivas NI. Oropharyngeal and nasopharyngeal suctioning of meconium-stained neonates before delivery of their shoulders: Multicentre, randomised controlled trial. Lancet. 2004;364:597–602 10.1016/S0140-6736(04)16852-9 [DOI] [PubMed] [Google Scholar]
- 22.Wiswell TE, Henley MA. Intratracheal suctioning, systemic infection, and the meconium aspiration syndrome. Pediatrics. 1992;89:203 [PubMed] [Google Scholar]
- 23.Mdoe PF, Ersdal HL, Mduma E, Moshiro R, Dalen I, et al. Randomized controlled trial of continuous Doppler versus intermittent fetoscope fetal heart rate monitoring in a low-resource setting. Int J Gynaecol Obstet. 2018;143:344–350. 10.1002/ijgo.12648 [DOI] [PubMed] [Google Scholar]
- 24.Kamala BA, Ersdal HL, Dalen I, Abeid MS, Ngarina MM, et al. Implementation of a novel continuous fetal Doppler (Moyo) improves quality of intrapartum fetal heart rate monitoring in a resource-limited tertiary hospital in Tanzania: An observational study. PLoS One. 2018;13:e0205698 10.1371/journal.pone.0205698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ersdal HL, Mduma E, Svensen E, Perlman JM. Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries. A prospective descriptive observational study. Resuscitation. 2012;83:869–73. 10.1016/j.resuscitation.2011.12.011 [DOI] [PubMed] [Google Scholar]
- 26.Moshiro R, Ersdal HL, Mdoe P, Kidanto HL, Mbekenga C. Factors affecting effective ventilation during newborn resuscitation: a qualitative study among midwives in rural Tanzania. Glob Health Action. 2018;11:1423862 10.1080/16549716.2018.1423862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perlman JM, Risser R. Severe fetal acidemia: Neonatal neurologic features and short-term outcome. Pediatr Neurol.1993;9:277–82 10.1016/0887-8994(93)90063-i [DOI] [PubMed] [Google Scholar]
- 28.Patel Ravi M, Sarah Kandefer, Walsh Michele C., Bell Edward F., Carlo Waldemar A., et al. Causes and Timing of Death in Extremely Premature Infants from 2000 through 2011N Engl J Med 2015; 372:331–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Massawe A, Kidanto HL, Moshiro R, Majaliwa E, Chacha F, Shayo A, et al. A care bundle including antenatal corticosteroids reduces preterm infant mortality in Tanzania a low resource country. PLoS One. 2018;13:e0193146 10.1371/journal.pone.0193146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laptook AR, Salhab W, Bhaskar B. Admission Temperature of Low Birth Weight Infants: Predictors and Associated Morbidities. Pediatrics. 2007;119:e643–9. 10.1542/peds.2006-0943 [DOI] [PubMed] [Google Scholar]
- 31.de Siqueira Caldas JP, Ferri WAG, Marba STM, Aragon DC, Guinsburg R, et al. Eur J Pediatr (2019). 10.1007/s00431-019-03386-9 [DOI] [Google Scholar]
- 32.Mccall EM, Alderdice F, Halliday HL, Vohra S, Johnston L. Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants. Cochrane Database of Systematic Reviews. 2018. Issue 2. Art. No.: CD004210. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leadford AE, Warren JB, Manasyan A, Chomba E, Salas AA, Schelonka R, et al. Plastic Bags for Prevention of Hypothermia in Preterm and Low Birth Weight Infants. Pediatrics. 2013;132:e128–34 10.1542/peds.2012-2030 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.