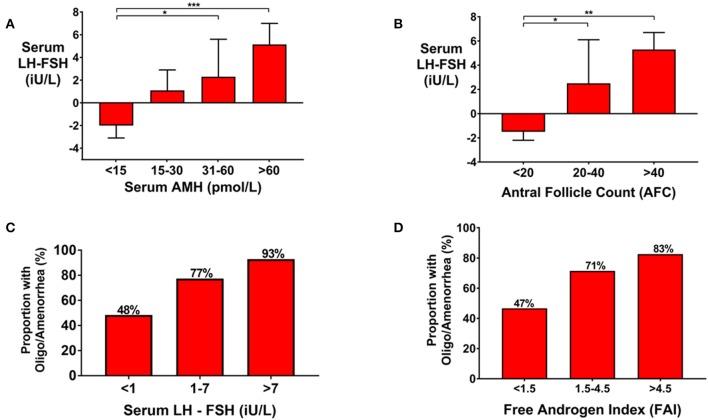
Figure 3.
(A) Bar graph (Median ± IQR) of serum LH-FSH (iU/L) by categories of serum AMH (pmol/L) in women presenting with oligo/amenorrhea, or eumenorrheic women in the follicular phase of the menstrual cycle (days 1–8). Groups were compared by the Kruskal Wallis test with post-hoc Dunn's multiple comparison test. Gonadotropin secretion was more LH-predominant with increasing category of AMH. *P < 0.05, ***P < 0.001. (B) Bar graph (median ± IQR) of serum LH-FSH (iU/L) by categories of AFC in women presenting with oligo/amenorrhea or eumenorrheic women in the follicular phase of the menstrual cycle (days 1–8). Groups were compared by the Kruskal Wallis test with post-hoc Dunn's multiple comparison test. Gonadotropin secretion was more LH-predominant with increasing category of AFC. *P < 0.05, **P < 0.01. (C) Frequency of oligomenorrhea was higher by increasing categories of serum LH-FSH (iU/L) when compared by univariate logistic regression (P = 0.003). The number of women in each category were as follows: serum LH-FSH < 1 iU/L (n = 29); 1–7 iU/L (n = 44), >7 iU/L (n = 14). The odds of oligomenorrhea was increased by 3.6-fold (95% CI 1.3–10.0) in those with serum LH-FSH 1–7 iU/L and by 13.9-fold (95% CI 1.6–121) in those with serum LH-FSH >7 iU/L compared to those with serum LH-FSH < 1 iU/L. (D) The frequency of oligomenorrhea were higher by category of Free Androgen Index (FAI). The number of women in each categories of FAI were as follows: FAI < 1.5 (n = 34); 1.5–4.5 (n = 94); >4.5 (n = 44). When compared by univariate logistic regression, the odds of oligomenorrhea was increased 2.9-fold (95% CI 1.0–16.8) in those with FAI > 4.5 compared to those with FAI < 1.5 (P = 0.039).