Figure 2.
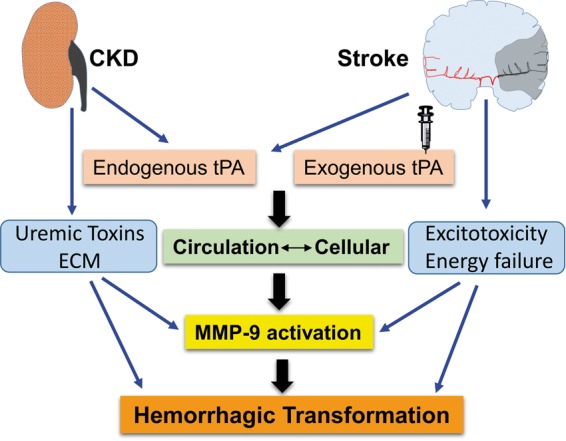
Possible mechanism of hemorrhagic transformations after thrombolysis. Cumulative endogenous tPA in circulation due to abnormalities in tPA/PAI ratio and exogenous administration affects the influx of excess circulatory tPA into the ischemic tissue. Excess accumulation of extracellular matrix components, uremic toxins, energy failure, oxidative stress, and excitotoxicity influences the effects of cellular as well as circulatory tPA. In stroke–CKD cases, bleeding complications are mediated by MMP-9, synergistically with cytokine activity of tPA, uremic toxins, and altered ECM leading to hemorrhagic transformation.
CKD: chronic kidney disease; MMP-9: matrix metalloproteinase-9; tPA: tissue plasminogen activator; ECM: extracellular matrix.
