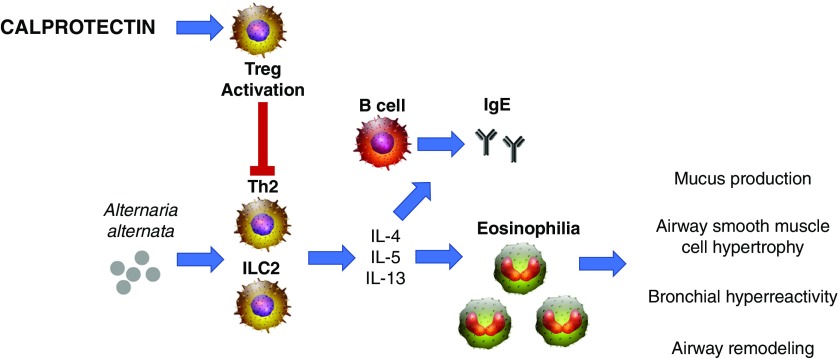
Figure 1.
Effects of calprotectin on Alternaria alternata–induced type 2 allergic airway inflammation. A. alternata challenge results in a robust type 2–driven inflammation (T-helper cell type 2 [Th2] and group 2 innate lymphoid cells [ILC2], type 2–associated cytokines [IL-4, IL-5, and IL-13], and chemokines [eotaxins, such as CCL11 and CCL24]) and recruits eosinophils to the lungs. Type 2 cytokines mediate class switching of B cells to secrete IgE upon exposure to antigen. These type 2 responses contribute to the hallmarks of asthma pathogenesis, including mucus production, subepithelial fibrosis, bronchial remodeling, and airway hyperresponsiveness. Calprotectin significantly limits allergic airway inflammation by limiting the production of IL-13, CCL11, CCL24, serum IgE, eosinophil recruitment, and airway hyperresponsiveness. Furthermore, calprotectin enhances T regulatory cell (Treg) activation, which suppresses Th2-mediated hyperinflammation.