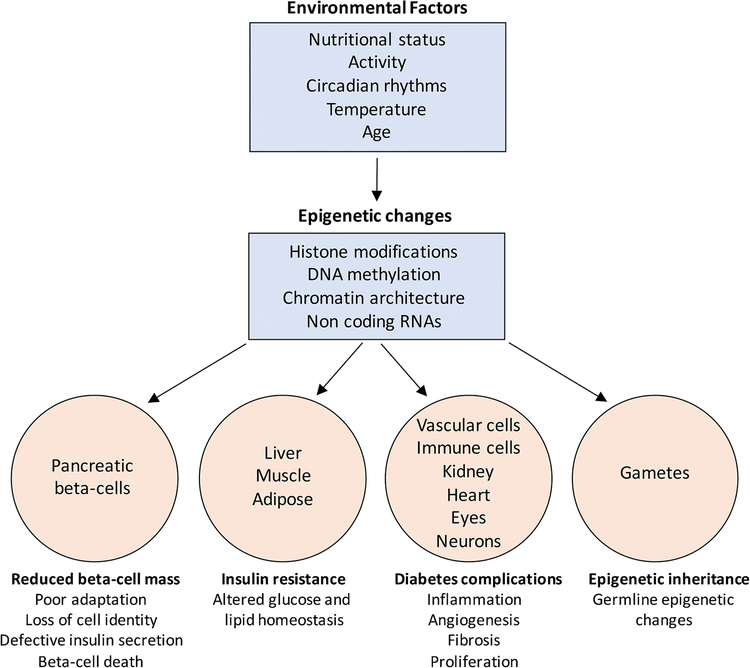
Figure 1.
Variations in environmental factors such as nutritional status (diet), activity (sedentary lifestyle), circadian rhythms (sleep disruption), seasonal changes in temperature, and even aging can alter the cellular epigenome. These changes may occur in the histone modifications, DNA methylation patterns, chromatin accessibility, as well as the expression of non-coding RNA species such as lncRNAs and miRNAs. The epigenetic dysregulation in response to adverse environmental exposure in turn drives transcriptional changes across several tissues such as the insulin producing beta-cells and insulin sensitive organs including liver, muscle, and adipose. This can eventually induce a deficit of functional beta-cell mass and impaired insulin secretion, as well as drive insulin resistance, thus disrupting glucose homeostasis towards the pathogenesis of T2D. In addition, epigenetic alterations in vascular cells, kidney, retina, neurons, and immune cells can lead to multiple micro- and macro-vascular complications of diabetes. Finally, epigenetic changes in response to adverse environment can also occur in the germline and be potentially transmitted to the offspring, contributing to the inheritance of T2D risk.