Figure 1. Mindfulness state mediates social signal transduction at CNS phase.
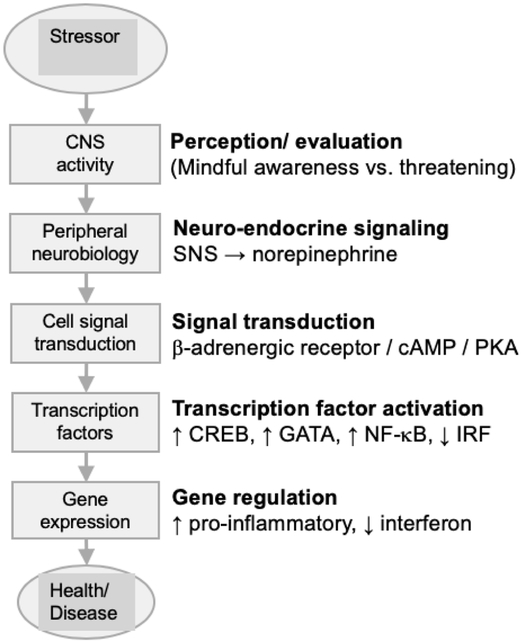
Brain-mediated attention and awareness serve as the detection filter for cognitive evaluation of threat associated with a stimuli (potential stressor) arising either from an actual challenge in the environment or one mentally imagined. Perception of the stimuli as a threat can activate the sympathetic nervous system (SNS), leading to release of norepinephrine (NE) at SNS nerve terminals, activation of b-adrenergic receptors on adjacent cells, and the cAMP/PKA signaling pathway that ultimately regulates gene expression by stimulating transcription factors such as cAMP response element-binding protein (CREB), GATA, and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB). We speculate that the conscious state of mindfulness cultivated during mindfulness meditation and carried forth in daily living functions as a filter in attention and awareness that functions to reduce the valence of an imagined threat, resulting in reduced activation of the transcription factors that influence gene expression, and so improve health via reduction in chronic diseases and illnesses such as cardiovascular disease (CVD), cancer, and depression. Figure adapted with permission (Cole, 2014). We acknowledge that SNS activation caused by acute environmental challenges, such as escaping from danger, are short lived and adaptive to human health and survival. Therefore, it is reasonable that mindfulness would be more health protective, and relevant from a social genomics perspective, for stressors that are chronic in nature (e.g., social isolation, chronic pain, cancer survivorship, caregiving, insomnia) or elicited mentally from previous experience or future concern (e.g., burnout, post-traumatic stress disorder, social phobias and anxieties, job loss, financial concerns)
