Figure 1.
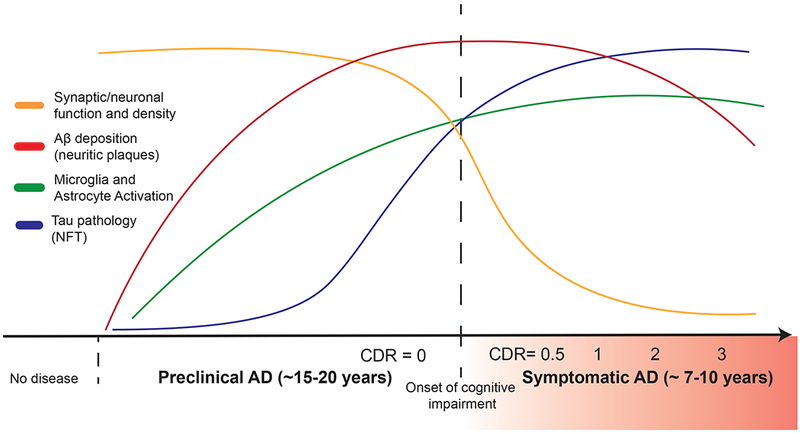
Timing of major AD pathophysiological events in relation to clinical course. A protracted preclinical phase of disease is characterized by the early onset of amyloid deposition. This is detected by a reduction in CSF and plasma levels of Aβ42 or increased global signal on amyloid PET imaging. Concurrently, there are early neuroinflammatory changes (such as microglial activation). Microgliosis can be detected longitudinally via use of PK11195 PET imaging though better agents are needed. This is followed by the spread of neurofibrillary tangle (NFT) tau pathology from the medial temporal lobes into neocortex. Increased signal on tau PET imaging and increased CSF phospho-tau levels mark this change in patients. Synaptic dysfunction, synapse loss and neurodegeneration accumulates with pathologic spread of tau aggregates. Imaging analysis of hippocampal and cortical volumes allows for longitudinal tracking of neurodegenerative changes. Onset and progression of cognitive impairment correlates with accumulation of tau and hippocampal volume loss but not amyloid deposition. Onset and severity of clinical symptoms in AD can be staged by use of the Clinical Dementia Rating (CDR) scale, where a score of 0 indicates normal cognition and scores of 0.5, 1, 2 and 3 indicate questionable, mild, moderate and severe dementia, respectively.
