Abstract
Background
Many antibiotics prescribed in the outpatient setting result from upper respiratory tract infections (URTIs); however, these infections are often viral. Virtual visits have emerged as a popular alternative to office visits for URTIs and may be an important target for antimicrobial stewardship programs.
Methods
This retrospective cohort study evaluated adult patients diagnosed with sinusitis treated within a single primary care network. The primary objective was to compare guideline-concordant diagnosis between patients treated via virtual visits vs in-office visits. Guideline-concordant bacterial sinusitis diagnosis was based on national guideline recommendations. Secondary objectives included comparing guideline-concordant antibiotic prescribing between groups and 24-hour, 7-day, and 30-day revisits.
Results
A total of 350 patients were included in the study, with 175 in each group. Patients treated for sinusitis were more likely to receive a guideline-concordant diagnosis in the virtual visit group (69.1% vs 45.7%; P < .001). Additionally, patients who completed virtual visits were less likely to receive antibiotics (68.6% vs 94.3%; P < .001). Guideline-concordant antibiotic selection was similar between groups (67.5% vs 64.8%; P = .641). The median duration of therapy in both groups was 10 days (P = .88). Patients completing virtual visits were more likely to revisit for sinusitis within 24 hours (8% vs 1.7%; P = .006) and within 30 days (14.9% vs 7.4%; P = .027).
Conclusions
In adult patients presenting with sinusitis, care at a virtual visit was associated with an increase in guideline-concordant diagnosis and a decrease in antibiotic prescribing compared with in-office primary care visits. Virtual visit platforms may be a valuable tool for antimicrobial stewardship programs in the outpatient setting.
Keywords: antimicrobial stewardship, sinusitis, telemedicine, virtual visits
Antibiotic overprescribing and emerging antimicrobial resistance are pressing concerns to public health across the globe [1]. The majority of antibiotic prescribing occurs in outpatient settings, with the Centers for Disease Control and Prevention (CDC) estimating that primary care physicians prescribe more than 106 million antibiotics annually in the United States [2]. Unfortunately, many of these antibiotic courses are unnecessary, with a projected 40%–60% of patients receiving antibiotic treatment for viral upper respiratory tract infections (URTIs) [3, 4]. Sinusitis is the most common indication for outpatient antibiotic prescriptions; however, the CDC estimates that >90% of cases are caused by viral pathogens and that antibiotics are not warranted in most instances [5].
Antimicrobial stewardship programs (ASPs) have been created to improve antibiotic prescribing, helping to fight issues related to antimicrobial resistance while improving patient outcomes [6]. Historically, the majority of ASP initiatives were focused on improving inpatient antimicrobial prescribing. More recently, the focus of ASPs has shifted to the outpatient setting, with the CDC and The Joint Commission (TJC) proposing core elements of performance for stewardship programs in ambulatory care settings [7, 8]. As an alternative to traditional office visits, the emergence of direct-to-consumer (DTC) telemedicine through virtual visits is an increasingly popular method of health care delivery and another important ambulatory care target for ASPs. These visits provide patients with quick and convenient access to primary care providers for a wide variety of uncomplicated complaints such as URTIs. During virtual visits, antibiotic prescribing is typically determined based on an algorithm of patient-reported symptoms and severity without a physical exam [9].
Both the Infectious Diseases Society of America (IDSA) and the American Academy of Otolaryngology have developed guideline recommendations that outline key diagnostic criteria that correlate with an increased likelihood of bacterial sinusitis and define when antibiotic treatment of sinusitis may be appropriate [10, 11]. At this time, there is a paucity of literature evaluating the appropriateness of diagnosis and prescribing for URTIs in the virtual visit setting. The purpose of this study was to compare diagnosis and prescribing practices between virtual visits and office visits for adults diagnosed with sinusitis within a primary care network.
METHODS
This retrospective cohort study was conducted at Mercy Health Physician Partners’ (MHPP) primary care network in Grand Rapids, Michigan. Adult patients aged ≥18 years were eligible for study inclusion if they completed a virtual or office visit within the study period of January 1, 2018, to June 30, 2018. Included patients must have been diagnosed with viral sinusitis or acute bacterial sinusitis via virtual visit or diagnosed with an ICD-10 code corresponding to sinusitis via an office visit (J01.90, J01.8, J01.00, or J01.10). Patients were selected for inclusion via random number generating and were screened for inclusion until the target sample size of 350 patients was met. Patients were excluded if they were diagnosed with fungal sinusitis or if they were immunocompromised with any of the following: HIV with a CD4 count <200, active malignancy currently receiving chemotherapy, or receiving chronic steroid therapy equivalent to ≥20 mg/d of prednisone for at least 30 days.
The MHPP network is comprised of >500 physician and midlevel providers offering comprehensive care, including primary care at 22 offices in the Grand Rapids metropolitan area. Virtual visits, powered by Zipnosis, began being offered for URTIs, including sinusitis, by MHPP primary care providers in September 2017. The MHPP virtual visits are conducted via a text-based format, with the platform accessible from a smartphone or computer. Virtual visits are available to patients 7 days per week from 08:00 to 20:00. Patients select from a list of chief complaints and complete a corresponding questionnaire regarding symptom types, duration, and severity, with an opportunity to provide any additional information to the primary care provider within a single free text entry at the end of the questionnaire. Providers receive virtual visit notifications via an app on their phone or computer and receive a summary of the patient’s chief complaint, symptoms, and free text comments. Along with the patient summary, the virtual visit software lists criteria based on national guidelines for bacterial sinusitis to help guide provider diagnosis (Table 1). Based on the diagnoses chosen by the provider, the software will provide a drop-down menu of antibiotic choices for bacterial sinusitis or supportive care options for any diagnosis of sinusitis.
Table 1.
Diagnostic Criteria from Virtual Visit Software
| Sinusitis Adherence Criteria from Zipnosis Virtual Visit | |
|---|---|
| 7 days of symptoms AND at least 2 of the following: | • Fever |
| • Double sickening (worsening symptoms after initial improvement) | |
| • Sinus pressure or headache | |
| • Purulent nasal discharge (green or yellow) | |
| OR | |
| Symptom duration of 10 days or more |
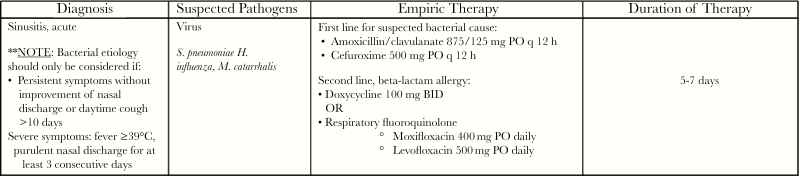
Antimicrobial stewardship efforts at MHPP are supported by an antimicrobial stewardship physician lead who provides care within the MHPP Infectious Diseases practice and an infectious diseases pharmacist who is employed by Mercy Health Saint Mary’s Hospital and provides both inpatient and outpatient ASP management and leadership. The ASP constructs an annual outpatient antibiogram and provides outpatient empiric therapy guidelines for antimicrobial therapy that include recommendations for the treatment of sinusitis based on local susceptibilities as well as national guidelines (Figure 1). Annual education is provided via an electronic educational system, whereas antibiograms and empiric therapy guidelines are made available electronically via the Mercy Health Saint Mary’s and MHPP intranet site. The virtual visit software and algorithms are developed by a third-party vendor and cannot be modified by the local ASP.
Figure 1.
Mercy Health Saint Mary’s empiric therapy guidelines for sinusitis. Abbreviations: BID, twice daily; PO, oral.
Data were collected from the AthenaHealth outpatient records system for both MHPP office and virtual visits. Patients were stratified into 2 groups for comparison based on visit type (ie, office visit vs virtual visit). Patient characteristics, including age, sex, beta-lactam allergies, and symptom type and duration, were collected. The primary objective of this study was to compare the rate of guideline-concordant sinusitis diagnosis, based on IDSA and American Academy of Otolaryngology recommendations, between virtual visits and office visits (Figure 1). Appropriate diagnosis was confirmed by an unblinded independent review from a board-certified infectious diseases physician. Secondary objectives included comparing rates of antibiotic prescribing, guideline-concordant antibiotic selection and duration, and supportive care prescribing between office and virtual visits. The appropriateness of antibiotic selection and duration were determined by local outpatient antimicrobial empiric therapy guidelines (Figure 1). The appropriateness of antibiotic prescribing was assessed for all patients, regardless of guideline-concordant diagnosis. Additional patient outcomes collected included 24-hour, 7-day, and 30-day unplanned revisits, 30-day hospitalization, and Clostridiodes difficile infection within 30 days of initial visit. A revisit included an office, urgent care, emergency department, or virtual visit.
Statistical Analysis
Assuming a baseline office visit rate of appropriate prescribing of 50%, a sample size calculation estimated that at least 350 patients would be needed to detect a 10% difference in the primary end point with 80% power and a 2-sided alpha of .05 [3, 4]. Nominal data were assessed with the chi-square or Fisher exact test as appropriate, and continuous data were assessed with a Student t test or Mann-Whitney U test based on the distribution of data. Multivariate logistic regression was conducted to assess for independent risk factors for revisits. Factors with P < .2 in bivariate analyses were considered for inclusion in the model. SPSS statistical software, version 22 (IBM Corporation, Armonk, NY), was used for all statistical analyses.
RESULTS
During the 6-month study period, 3897 patients were diagnosed with sinusitis by an MHPP primary care provider. A total of 394 patients were screened until the target sample size of 350 patients was met, with 175 patients per group. Provider type and incidence of beta-lactam allergies were similar between groups; however, the median age of patients treated in the office visit group (interquartile range [IQR]) was significantly older compared with the virtual visit group (50 [35–60] vs 38 [32–50] years; P < .001). Additionally, there were fewer females treated in the office visit group compared with the virtual visit group (64.6% vs 80.6%; P = .001).
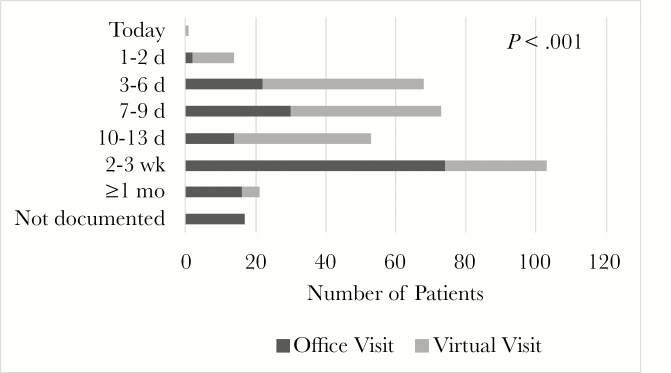
Documented patient-reported symptoms are displayed in Table 1. The majority of symptoms were more commonly reported for patients in the virtual visit group, including double-sickening, facial pain or pressure, nasal drainage, and myalgias (Table 2).In addition, patient self-request for antibiotics was also more common in the virtual visit group (3.4% vs 10.9%; P = .007). The duration of symptoms at the time of the visit was shorter in the virtual visit group compared with the office visit group (Figure 2).
Table 2.
Patient-Reported Symptoms
| Symptoms, No. (%) | Office Visit (n = 175) | Virtual Visit (n = 175) | P Value |
|---|---|---|---|
| Chills | 12 (6.9) | 41 (23.4) | <.001 |
| Cough | 113 (64.6) | 114 (65.1) | .911 |
| Difficulty breathing | 27 (15.4) | 0 (0) | <.001 |
| Double sickening | 13 (7.4) | 69 (39.4) | <.001 |
| Facial pain or pressure | 134 (76.6) | 155 (88.6) | .003 |
| Fatigue or malaise | 58 (33.1) | 149 (85.1) | <.001 |
| Fever | 20 (11.4) | 26 (14.9) | .343 |
| Headache | 64 (36.6) | 150 (85.7) | <.001 |
| Myalgia | 14 (8) | 61 (34.9) | <.001 |
| Nasal congestion | 88 (50.3) | 163 (93.1) | <.001 |
| Nasal drainage purulence documented | 97 (55.4) | 137 (78.3) | <.001 |
| Tooth pain | 1 (0.6) | 73 (41.7) | <.001 |
| Wheezing | 22 (12.6) | 13 (7.4) | .109 |
Figure 2.
Reported duration of symptoms.
Guideline-Concordant Diagnosis and Prescribing
Guideline-concordant sinusitis diagnosis based on national guidelines was less common in the office visit group compared with the virtual visit group (45.7% vs 69.1%; P < .001). All of the patients who had an inappropriate diagnosis in each group were diagnosed with bacterial sinusitis but did not meet national guideline criteria. Patients in the office visit group were more likely to receive a bacterial sinusitis diagnosis compared with patients in the virtual visit group (94.3% vs 68.6%; P < .001).
There were significantly more antibiotics prescribed in the office visit group compared with the virtual visit group (94.3% vs 68.6%; P < .001). When antibiotics were prescribed, the rate of guideline-concordant antibiotic prescribing was not different between office and virtual visits (64.8% vs 67.5%; P = .641). Antibiotic selection was similar between groups (P = .113) (Supplementary Data). The most commonly prescribed antibiotic in both groups was amoxicillin-clavulanate. Of the 25 patients who self-requested antibiotics, 100% of patients in the office visit group were prescribed an antibiotic, compared with 63.2% in the virtual visit group (P = .080).
Guideline-concordant duration of antibiotic therapy was similar in both groups (43.6% vs 40.8%; P = .636). The median duration of antibiotic therapy (IQR) was 10 (7–10) days for both groups (P = .882). Ten patients in the office visit group and 3 patients in the virtual visit group received >10 days of antibiotic therapy. Supportive care was more commonly recommended or prescribed to patients who completed a virtual visit compared with those who completed an office visit (71.4% vs 88.6%; P < .001) (Supplementary Data).
Finally, patients who completed virtual visits were more likely to have an unplanned revisit related to sinusitis within 24 hours (1.7% vs 8%; P = .006) and within 30 days (7.4% vs 14.9%; P = .027) of the initial visit when compared with office visits. There was no difference in revisits at 7 days between groups (office visit 16.6% vs virtual visit 14.9%; P = .659). In multivariate logistic regression, the only factor independently associated with 24-hour revisit was patient self-request for antibiotics, which was protective of 24-hour revisit (odds ratio, 0.20; 95% confidence interval, 0.06–0.68) (Table 3). There were no factors that independently predicted 30-day revisits. No patient in the office group or virtual visit group required hospital admission or was diagnosed with C. difficile infection within 30 days of their initial visit.
Table 3.
Multivariate Logistic Regression: Risk Factors for Revisits at 24 Hours
| Revisit Within 24 Hours | P Value | OR (95% CI) |
|---|---|---|
| Office visit | .557 | 0.62 (0.13–3.03) |
| Male | .143 | 0.21 (0.03–1.69) |
| Self-requested antibiotics | .010 | 0.20 (0.06–0.68) |
| Fatigue/malaise | .317 | 0.40 (0.07–2.39) |
| Chills | .104 | 0.39 (0.12–1.21) |
| Antibiotics prescribed | .376 | 1.68 (0.53–5.33) |
Abbreviations: CI, confidence interval; OR, odds ratio.
DISCUSSION
Our study demonstrated that adult patients treated for sinusitis via a virtual visit were more likely to receive a guideline-concordant diagnosis and were prescribed significantly fewer antibiotics when compared with patients who were evaluated at a primary care office. This resulted from a higher percentage of patients receiving an appropriate diagnosis of viral sinusitis, which was associated with a lower rate of antibiotic prescribing. The Zipnosis virtual visit platform may have aided in increasing the rate of appropriate diagnosis for sinusitis due to the presence of guideline-supported criteria for bacterial diagnosis presented to the provider directly within the visit. In contrast, providers diagnosing and prescribing at office visits may not always have a summary of guideline recommendations readily available. Additionally, we observed that patients self-requested antibiotics in both groups; however, providers were less likely to prescribe antibiotics to patients treated within a virtual visit. With the mounting pressure to prescribe antibiotics from patients in the outpatient setting, it is possible that the virtual visit platform provides a space for providers where they feel more comfortable diagnosing viral infections and counseling on antibiotic avoidance.
Despite virtual visits demonstrating significantly improved guideline-concordant diagnosis and decreased antibiotic prescribing, the selection of a guideline-concordant antibiotic agent and duration was similar between groups. The telemedicine platform currently used by MHPP is not based on local sensitivities and does not follow the organization’s current empiric therapy guidelines. Additionally, the preselected duration of therapy for most regimens is 10 days, which exceeds the 5–7-day recommendation of current national guidelines. Furthermore, current counseling language provided to patients at the close of each virtual visit for sinusitis includes language stating that antibiotics are not warranted until symptoms have lasted at least 7 days, which is in contrast to the 10 days listed in the current national guideline recommendations. As the popularity of telemedicine continues to grow, virtual visits and their software platforms could be an important tool for ASPs. Interventions to optimize platform settings, including incorporation of local guidelines and strengthening patient education, may help increase the rate of guideline-concordant prescribing.
The quality of care provided by virtual visits has been previously called into question. To date, very few studies have been published assessing the impact of direct-to-consumer telemedicine visits via text- or video-based virtual platforms on appropriate diagnosis and antibiotic prescribing. Halpren-Ruder and colleagues sought to assess virtual visit quality of care by comparing adherence to antibiotic prescribing guidelines for sinusitis between on-demand video-based virtual visits and in-person visits at either an urgent care center or emergency department [12]. Of the 570 patients included in the study, the authors found that guideline-concordant antibiotic prescribing was not different between groups (71% virtual visits vs 61% urgent care vs 68% emergency department; P = .29). The authors concluded that delivery of care through virtual visits did not compromise quality. Davis et al. evaluated 157 patients treated for sinusitis via a video-based virtual visit compared with a traditional urgent care visit. Similar to our study, antibiotic prescribing for sinusitis was significantly lower in patients treated at a virtual visit compared with in-person urgent care visits (67% vs 92%; P < .001) [13]. The authors concluded that awareness and access to prescribing guidelines, rather than care delivery method, were likely the most important factors influencing appropriate antibiotic prescribing. With the recent push from both the CDC and TJC to implement strategies for stewardship in ambulatory settings, virtual visits may represent an important opportunity to implement guidelines and improve the quality of antibiotic prescribing. Finally, Ray and colleagues evaluated prescribing via direct-to-consumer telemedicine visits compared with in-office visits or urgent care visits in a pediatric population with acute URTIs. Children treated for URTIs in virtual visits were more likely to receive antibiotics compared with those who presented for office visits or to urgent care (52% telemedicine vs 31% office visit vs 42% urgent care; P < .001) [14]. Additionally, they found that the rate of guideline-concordant antibiotic prescribing was lower for pediatric patients completing telemedicine visits (59% telemedicine vs 70% office visit vs 67% urgent care; P < .001). The authors concluded that pediatric patients treated for URTI at virtual visits were more likely to receive antibiotics and less likely to receive guideline-concordant management compared with those treated in the primary care office or at urgent care. These conclusions, which are in contrast to our own findings, are important to note. The mixed results seen in each study may be due to the different patient populations evaluated, diseases states included, and the way in which virtual visits were delivered (text- vs audio- vs video-based). The ideal method for the delivery of telemedicine has yet to be identified.
Lastly, patients who completed virtual visits were more likely to have an unplanned revisit for sinusitis-related care at both 24 hours and 30 days from their index visit. Of note, in the multivariate model, virtual visits were not an independent risk factor for revisits at either 24 hours or 30 days. We hypothesize that the increase in revisits could be due to several causes. First, the text-based virtual visit offered within MHPP lacks real-time and face-to-face interaction between the provider and patient, which limits opportunities for dialogue. Having some capability for live interaction between provider and patient may alleviate higher rates of revisits by allowing patients to convey their questions regarding diagnosis and treatment at the time of visit. Virtual visits additionally lack a physical exam, which has the potential to affect appropriate diagnosis [15]. Finally, in our multivariate model, self-requesting antibiotics was found to be protective for unplanned revisits at 24 hours. This could mean that patients who self-requested antibiotics were more likely to receive them and not feel the need to seek further care or that the refusal of self-requested antibiotics and education provided discouraged patients from further revisits.
Study Limitations
There are limitations to our study that must be considered. First, as with all retrospective investigations, there is the risk for selection bias as well as the reliance on appropriate documentation. There was a significant difference in documentation noted between visit types due to the fact that office visit documentation is provider-driven whereas virtual visit documentation is patient-driven. The text-based virtual visit platform offered by Zipnosis is formatted as a questionnaire with closed-ended and “yes/no” questions regarding symptoms; only a single comment box is available for free text patient comments. This is likely why several reported symptoms, including double-sickening, were more often reported with virtual visits compared with office visits. For example, self-request for antibiotics was extracted from the free-text patient comments for virtual visits and provider documentation for in-office visits. Additionally, the text-based platform does not allow for face-to-face interaction with a provider, which can also be considered a limitation when considering generalizability to other types of telemedicine platforms. Furthermore, the Zipnosis platform does not interface with the electronic medical health record; therefore, medical history, including comorbidities, was not available to be collected. This lack of software interface is a limitation of virtual visits, as these data are not available to providers when making decisions. We found that patient demographics were different between groups; patients completing virtual visits were more likely to be younger in age. This can likely be explained by the age restriction of 18–65 that is placed on virtual visits within our health system. Finally, we only assessed the use of virtual visits for sinusitis, which may limit the generalizability of our results to other diagnoses. Despite these limitations, our study provides important insights into the utility of virtual visits, highlighting areas for improvement and opportunities to optimize guideline-concordant diagnosis and prescribing.
CONCLUSIONS
In adult patients presenting with sinusitis, care at a virtual visit was associated with an increase in guideline-concordant diagnosis and a decrease in antibiotic prescribing compared with in-office primary care visits. As the use of telemedicine in health care continues to increase, virtual visit software with embedded guidelines supported by national recommendations and local susceptibility trends may be a valuable tool for ASPs to improve guideline-concordant diagnosis and prescribing.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Financial support. No external or internal funding was received for this study.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. CDC/MMWR resistance threats 2013 report: Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States 2013. Available at: https://www.cdc.gov/drugresistance/pdf/ar-threats-2013–508.pdf. Accessed 26 June 2019.
- 2. Centers for Disease Control and Prevention. Outpatient antibiotic prescriptions – United States 2016. Available at: https://www.cdc.gov/antibiotic-use/community/pdfs/Annual-Report-2016-H.pdf. Accessed 26 June 2019.
- 3. Schroeck JL, Ruh CA, Sellick JA Jr, et al. . Factors associated with antibiotic misuse in outpatient treatment for upper respiratory tract infections. Antimicrob Agents Chemother 2015; 59:3848–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. . Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA 2016; 315:1864–73. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Antibiotic prescribing and use in doctor’s offices – adult treatment recommendations for acute rhinosinusitis. Available at: https://www.cdc.gov/antibiotic-use/community/for-hcp/outpatient-hcp/adult-treatment-rec.html. Accessed 26 June 2019.
- 6. Barlam TF, Cosgrove SE, Abbo LM, et al. . Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016; 62:e51–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core elements of outpatient antibiotic stewardship. MMWR Recomm Rep 2016; 65:1–12. [DOI] [PubMed] [Google Scholar]
- 8. The Joint Commission. Proposed new requirement at MM.09.01.03 – antimicrobial stewardship – ambulatory health care. Available at: https://jointcommission.az1.qualtrics.com/WRQualtricsControlPanel/File.php?F=F_eJ88Q1VIj0hLKjr. Accessed 26 June 2019.
- 9. Hickson R, Talbert J, Thornbury WC, et al. . Online medical care: the current state of “eVisits” in acute primary care delivery. Telemed J E Health 2015; 21:90–6. [DOI] [PubMed] [Google Scholar]
- 10. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. . Clinical practice guideline (updated): adult sinusitis. Otolaryngol Head Neck Surg 2015; 152(2 Suppl):S1–39. [DOI] [PubMed] [Google Scholar]
- 11. Chow AW, Benninger MS, Brook I, et al. ; Infectious Diseases Society of America IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis 2012; 54:e72–e112. [DOI] [PubMed] [Google Scholar]
- 12. Halpren-Ruder D, Chang AM, Hollander JE, Shah A. Quality assurance in telehealth: adherence to evidence-based indicators. Telemed J E Health 2019; 25:599–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davis CB, Marzec LN, Blea Z, et al. . Antibiotic prescribing patterns for sinusitis within a direct-to-consumer virtual urgent care. Telemed J E Health 2019; 25:519–22. [DOI] [PubMed] [Google Scholar]
- 14. Ray KN, Shi Z, Gidengil CA, et al. . Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics 2019; 143:Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. DeJong C, Santa J, Dudley RA. Websites that offer care over the Internet: is there an access quality tradeoff? JAMA 2014; 311:1287–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.