Description
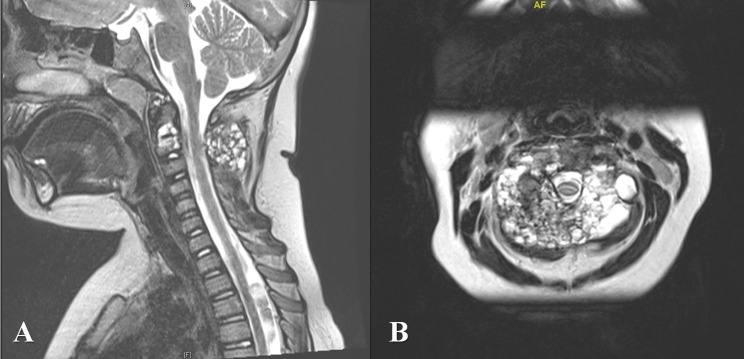
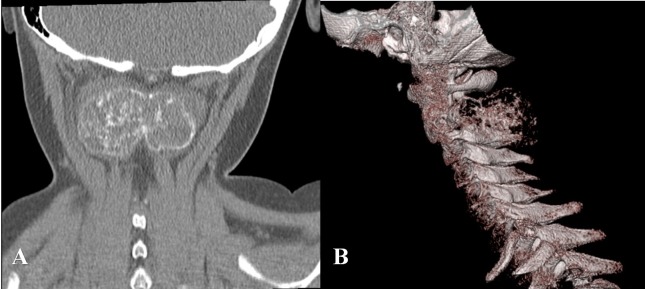
A 7-year-old girl presented to the emergency department with ‘clicking’ in her neck while trampolining, on a background history of neck pain for a year. There was no obvious history of trauma. Examination of the neck demonstrated a firm mass posteriorly with preserved neck movements and absence of any neurological deficit. In view of her atypical history and clinical examination, plain X-rays were performed which revealed lytic lesions in the body of C2. Detailed imaging was undertaken through CT and MRI. On T2-weighted MRI (figure 1), a giant dumbbell-shaped, multiseptated bony lesion involving the body, laminae, and posterior elements of C2 were noted. Multiple fluid-fluid levels were present within the lesion, resembling a giant ‘soap bubble’. CT images (figure 2) demonstrate the markedly enlarged bony lesion involving C2 with egg-shell thin cortices and increased vascular markings. Appearances were consistent with an aneurysmal bone cyst (ABC) at the C2 level. The child was transferred to the regional paediatric spinal centre where a CT-guided biopsy confirmed ABC and she subsequently underwent curettage of the lesion with autologous bone grafting for spinal stabilisation.
Figure 1.
(A) Midsagittal T2-weighted MRI image demonstrating the extent of the loculated aneurysmal bone cyst (ABC) at C2 without any compression of the neural structures. (B) Axial T2-weighted MRI image demonstrating the multiseptated ABC with fluid-fluid levels with complete involvement of C2.
Figure 2.
(A) Coronal view of non-contrast CT cervical spine demonstrating the dumbbell-shaped aneurysmal bone cyst of C2 with cortical thinning. (B) Sagittal three-dimensional reconstruction of the cervical spine demonstrating the lytic lesion at C2 associated with increasing vascular markings.
ABCs are rare but benign, highly vascular tumours and account for up to 1% of all bone tumours and 15% of primary spinal tumours.1–4 The majority of ABCs occur in the first two decades of life1–4 and uncommonly affect the cervical spine, with only 71 cases reported in the literature till recently.1
Imaging features of ABCs are characteristic and remain key to diagnosis. Plain X-rays may show expansile, well-circumscribed lytic lesions with periosteal calcification (‘eggshell-like’) and cortical thinning, often described as a ‘soap bubble’ appearance.5–7 In this case, the MRI findings were also suggestive of a ‘soap bubble’ appearance (figure 1). The typical MRI findings include the presence of a multiseptated cystic lesion with fluid-fluid levels, hypointense on T1-weighted but hyperintense on T2-weighted images, and contrast-enhancing septal walls.3 5–9 Fluid-fluid levels, in particular, are strongly suggestive of an ABC.10 However, a plethora of other diseases including giant cell tumour, eosinophilic granuloma, fibrous dysplasia, unicameral bone cyst, chondroblastoma, chondrosarcoma, chondromyxoid fibroma, Ewing’s tumour and metastatic carcinoma have all been reported to display similar imaging features as an ABC.1 4 5 A combination of both radiographs and MRI, alongside histological examination, is required to increase the likelihood of an accurate diagnosis.5
Although complete surgical excision of ABCs has been associated with high rates of cure,11 12 recurrence, however, remains a concern even after complete excision.1–4 7 8 11 13 The risks of aggressive surgery include spinal instability which may necessitate spinal instrumentation and fusion.2 3 Perioperative embolisation to aid vascular control has also been used as adjuvant therapy.1 11 Less aggressive surgical options include curettage14 while sclerotherapy is also reported to be safe and effective.11
In conclusion, we present the striking images of a giant ‘soap bubble’ representing an ABC in the cervical spine of a 7-year-old girl. Surgical management was successfully undertaken, and the patient is well at 5-year follow-up.
Learning points.
Aneurysmal bone cysts (ABCs) of the spine are benign, vascular tumours and account for up to 15% of primary spinal tumours. It is important to investigate thoroughly in cases with atypical presentations, as in this report.
Radiological features of ABCs include lytic lesions with periosteal calcification, often described as a ‘soap bubble’ appearance. MRI findings include a multiseptated lesion with fluid-fluid levels, hyperintense on T2 and hypointense on T1-weighted imaging.
Combination of both radiographic and MRI features help clinch the diagnosis although histological examination is often warranted to exclude other, more sinister, lesions.
Footnotes
Contributors: NJ and HMBI wrote the initial manuscript and created the figures. SM was in charge of the patient’s clinical care and provided critical comments on the draft. NA was the overall supervisor and helped write the final draft. All authors contributed equally to the project and agree to grant the rights to the BMJ.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Protas M, Jones LW, Sardi JP, et al. . Cervical spine aneurysmal bone cysts in the pediatric population: a systematic review of the literature. Pediatr Neurosurg 2017;52:219–24. 10.1159/000475820 [DOI] [PubMed] [Google Scholar]
- 2. Novais EN, Rose PS, Yaszemski MJ, et al. . Aneurysmal bone cyst of the cervical spine in children. J Bone Joint Surg Am 2011;93:1534–43. 10.2106/JBJS.J.01430 [DOI] [PubMed] [Google Scholar]
- 3. Sebaaly A, Ghostine B, Kreichati G, et al. . Aneurysmal bone cyst of the cervical spine in children: a review and a focus on available treatment options. J Pediatr Orthop 2015;35:693–702. 10.1097/BPO.0000000000000365 [DOI] [PubMed] [Google Scholar]
- 4. Mankin HJ, Hornicek FJ, Ortiz-Cruz E, et al. . Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol 2005;23:6756–62. 10.1200/JCO.2005.15.255 [DOI] [PubMed] [Google Scholar]
- 5. Mahnken AH, Nolte-Ernsting CCA, Wildberger JE, et al. . Aneurysmal bone cyst: value of Mr imaging and conventional radiography. Eur Radiol 2003;13:1118–24. 10.1007/s00330-002-1668-8 [DOI] [PubMed] [Google Scholar]
- 6. Kuna S, Gudena R. "Soap bubble" in the calcaneus. CMAJ 2011;183:1171 10.1503/cmaj.101525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pennekamp W, Peters S, Schinkel C, et al. . Aneurysmal bone cyst of the cervical spine (2008:7b). Eur Radiol 2008;18:2356–60. 10.1007/s00330-008-0944-7 [DOI] [PubMed] [Google Scholar]
- 8. Boubbou M, Atarraf K, Chater L, et al. . Aneurysmal bone cyst primary--about eight pediatric cases: radiological aspects and review of the literature. Pan Afr Med J 2013;15 10.11604/pamj.2013.15.111.2117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beltran J, Simon DC, Levy M, et al. . Aneurysmal bone cysts: MR imaging at 1.5 T. Radiology 1986;158:689–90. 10.1148/radiology.158.3.3945739 [DOI] [PubMed] [Google Scholar]
- 10. Davies AM, Cassar-Pullicino VN, Grimer RJ. The incidence and significance of fluid-fluid levels on computed tomography of osseous lesions. Br J Radiol 1992;65:193–8. 10.1259/0007-1285-65-771-193 [DOI] [PubMed] [Google Scholar]
- 11. Tsagozis P, Brosjö O. Current strategies for the treatment of aneurysmal bone cysts. Orthop Rev 2015;7:6182 10.4081/or.2015.6182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu JK, Brockmeyer DL, Dailey AT, et al. . Surgical management of aneurysmal bone cysts of the spine. Neurosurg Focus 2003;15:1–7. 10.3171/foc.2003.15.5.4 [DOI] [PubMed] [Google Scholar]
- 13. Frassanito P, D'Onofrio GF, Pennisi G, et al. . Multimodal management of aggressive recurrent aneurysmal bone cyst of spine: case report and review of literature. World Neurosurg 2019;126:423–7. 10.1016/j.wneu.2019.02.246 [DOI] [PubMed] [Google Scholar]
- 14. Reddy KIA, Sinnaeve F, Gaston CL, et al. . Aneurysmal bone cysts: do simple treatments work? Clin Orthop Relat Res 2014;472:1901–10. 10.1007/s11999-014-3513-1 [DOI] [PMC free article] [PubMed] [Google Scholar]