Figure 2. Topographic location of the EZ break relative to the foveal center.
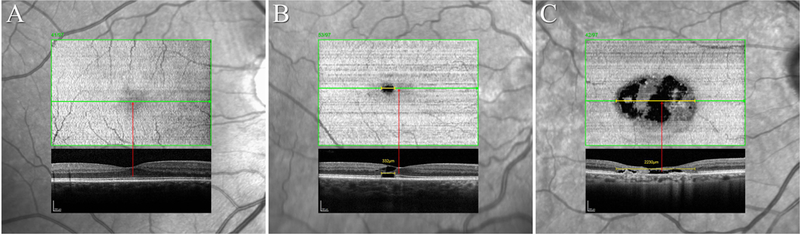
The diagnosis in MacTel may be established based on any satisfactory combination of the characteristic signs of the disease: a redistribution of luteal pigment, the concomitant pattern of hyper-reflectivity to short-wavelength light, OCT low reflective spaces in the inner/outer retina without retinal thickening, OCT focal outer retinal atrophy, mostly with overall retinal thinning; vascular abnormalities (telangiectatic and/or dilated capillaries in the deep plexus, dilated, blunted or right angle veins), or perivascular pigment plaques predominantly in the mid-retina, all in the absence of extensive retinal thickening or cystoid macular edema. Given an established diagnosis, the incidence of an EZ break and when it reaches the foveal center are landmark events in MacTel. Based on these two events, as reflected by OCT volume imaging, viewed either in B-scans or in transverse images of the Ellipsoid Zone, cases may be grouped: [A] Established MacTel disease, but no detectable EZ break. Contrast sensitivity, scotopic retinal sensitivity and reading speeds may be affected, BCVA and mesopic retinal sensitivity are preserved. [B] An EZ break is present but the nearest edge does not reach the foveal center. In these cases, mesopic microperimetry will demonstrate a scotoma co-locating with the area of the EZ break. BCVA is likely to be unaffected. [C] An EZ break is present and it also affects the foveal center. BCVA is likely to be affected. Subretinal neovascular proliferation (SRNV) or post-SRNV scarring is a secondary complication of MacTel, and may occur at any point in its natural history. SRNV may threaten central vision directly and responds to anti-vEGF therapy, whereas the basic disease process does not. At least a quick cursory en face glance is recommended in all eyes to exclude extreme cases e.g. with vertically oblong EZ breaks or major EZ breaks located largely outside the transfoveal scan. The functional relevance of the location of the EZ break is shown in Figure 5.
